This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Contact Dermatitis: 16 Natural Ways to Soothe Skin Irritation
March 30, 2023

When an irritant or something we have a sensitivity to touches our skin, an itchy, blistery rash can be the result. In fact, virtually everyone will develop contact dermatitis at some point during their lives.
Generally, it resolves without medical intervention, but if it persists for a month — or reoccurs and you don’t know the cause — visiting a dermatologist is recommended.
Fortunately, for the millions people in the United States affected each year, natural contact dermatitis treatments can help relieve the symptoms and speed healing.
Lesions and blisters commonly appear somewhere between 24 and 72 hours, depending on the irritant or allergen you have encountered. This inflammatory skin reaction can be caused by cosmetics and other beauty products, chemical solvents, certain medications, and plants.
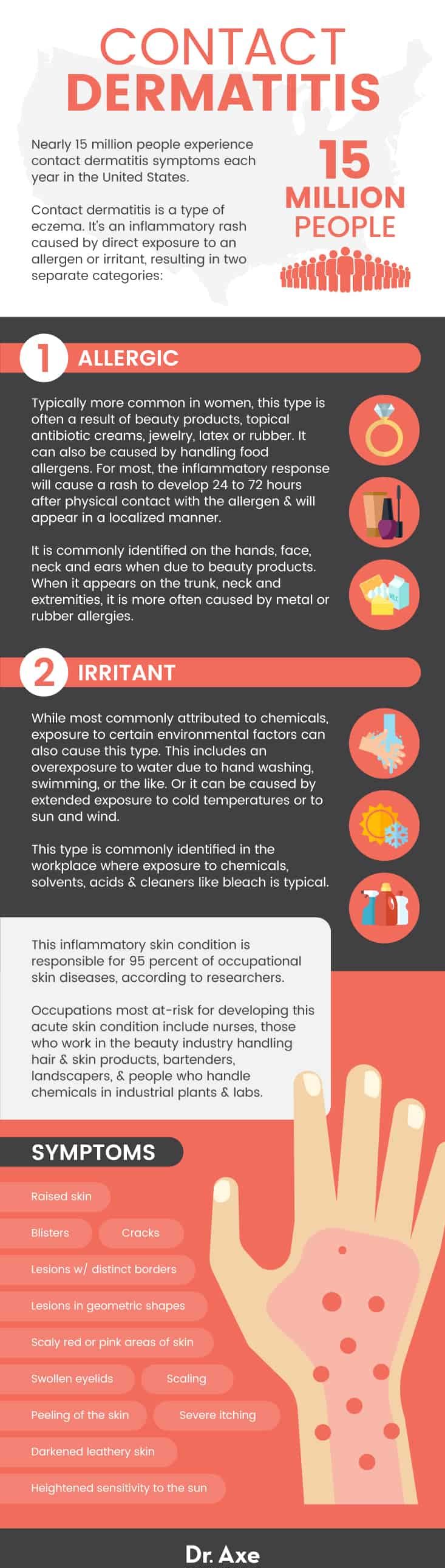
Contact dermatitis is responsible for 90 percent to 95 percent of occupational skin diseases and one of the most common reasons to see a dermatologist. Occupations most at-risk for developing this acute skin condition include:
- nurses
- those who work in the beauty industry handling hair and skin products
- bartenders
- landscapers
- people who handle chemicals in industrial plants and laboratories
One of the things that puzzles researchers is that there seems to be evidence that repeated exposure to certain compounds can increase the risk of the immune system becoming sensitized to them, resulting in a new allergic response. This has been shown, for example, in people who seemingly awaken to find themselves allergic to their wedding rings, those who suddenly become allergic to latex after wearing gloves for years or professional musicians who suddenly develop rashes as a result of their instruments.
While unsightly and uncomfortable, this skin condition is not contagious. It often heals within two to four weeks with effective home remedies. Plus, reoccurrences can often be limited by avoiding the offending compounds causing the inflammatory response.
What Is Contact Dermatitis?
This skin condition is an inflammatory rash caused by direct exposure to an allergen or irritant, resulting in two separate categories. Generally, in contact dermatitis caused by an irritant, an immediate inflammation of the skin occurs. If it’s caused by an allergen, the response may be delayed for several days.
While different compounds cause each of the different types, the symptoms and treatments are similar.
Allergic: Typically more common in women, this type is often a result of beauty products, topical antibiotic creams, jewelry, latex or rubber. For most, the inflammatory response will cause a rash to develop 24 to 72 hours after physical contact with the allergen and will appear in a localized manner.
It is commonly identified on the hands, face, neck and ears if due to beauty products. When it appears on the trunk, neck and extremities, it is more often caused by metal or rubber allergies.
When this type of rash occurs around the genitals, it is often a result of exposure to an allergen like latex found in condoms or certain chemicals found in spermicides and certain feminine hygiene products.
Poison ivy, sumac and oak rashes also fall into this category.
Irritant: While most commonly attributed to chemicals, exposure to certain environmental factors can also cause this type. This includes an overexposure to water due to hand washing, swimming (like a chlorine rash) or the like — or it can be caused by extended exposure to cold temperatures.
This type is commonly identified in the workplace where exposure to chemicals, solvents, acids and cleaners like bleach is typical. However, it can also be a result of licking your lips, exposure to the sun and the wind, and moisture trapped against the body. This is a rather wide category as both diaper rash and acid burns are included.
Signs and Symptoms
Contact dermatitis is a type of eczema, along with atopic dermatitis and seborrheic dermatitis, among others. Commonly recognized symptoms include:
- Scaly red or pink areas of skin
- Raised skin
- Blisters
- Lesions with distinct borders
- Lesions in geometric shapes
- Swollen eyelids
- Severe itching
- Peeling of the skin
- Scaling
- Cracks
- Heightened sensitivity to the sun
- Darkened leathery skin
When caused by poison ivy, poison sumac or poison oak, fluid-filled blisters appear in a line and continue to worsen for a couple of weeks. While the fluid in the blisters is not contagious, any residual urushiol — the compound that causes the reaction — can cause a reaction in others. This compound can remain active under fingernails, on clothing and on footwear for several days.
Causes and Risk Factors
This inflammatory skin condition is typically caused by irritants or allergens. Typical compounds associated with this skin rash include:
- Nickel and other metals. Some coins, jewelry, snaps, zippers and buckles can cause an uncomfortable rash. For those who display a sensitivity to metals, even leaning on a metal table, working on a laptop, talking on a mobile phone, carrying keys or wearing eyeglasses can cause irritation.
- Rubber and latex. Commonly found in balloons, gloves, mouse pads, condoms, goggles and even in the elastic in clothing like underwear, latex allergies are relatively common. An allergy to latex is more commonly associated with people who have had prolonged exposure to latex. This includes health care professionals, individuals who have had multiple surgeries, rubber industry workers, and people with seasonal or food allergies.
- Cosmetics. Even well-known luxury brands of cosmetics can contain chemicals and compounds that result in a rash. Lipstick, foundation, mascara, anti-aging eye creams, moisturizers and nail polish are all recognized for their potential to cause an inflammatory skin reaction.
- Grooming products. Like cosmetics, shampoo, conditioner, body wash, soap, shaving creams, hair dyes and styling products can cause a rash. Common ingredients that have been shown to cause an allergic response include lanolin, sodium lauryl sulfate, formaldehyde, Balsam of Peru, parabens and certain artificial fragrances.
- Antibiotic ointments. Two compounds commonly found in antibiotic ointments, bacitracin and neomycin, are known to cause a rash and symptoms associated with this skin condition in some people. While most reactions to these medications are minor, for some they can cause anaphylaxis, a dangerous, life-threatening reaction. Take extreme caution when using antibiotic or triple antibiotic ointments or creams.
- Fabric detergents. Certain chemicals in laundry detergents and fabric softeners, as well as the solvents used in dry cleaning and to clean leather, can cause the symptoms and rash in some people. As it can be difficult without trial and error to identify the exact chemical causing the reaction, an allergist can test patients so appropriate products can be used.
- Household cleaners. Window cleaners, dishwashing soap, dishwasher soap, floor cleaners, bathroom cleaners and grease removal products can cause skin rashes and irritation. Use gloves, or better yet, switch products to avoid harmful chemicals. Try my recipe for Homemade Melaleuca Lemon Household Cleaner, an effective cleaner that uses vinegar, essential oils and water.
- Fertilizers and pesticides. If you work in the agriculture field or are a home gardener, fertilizers and pesticides can cause irritant contact dermatitis. Use caution as these harsh chemicals are not safe for consumption, nor are they safe for your skin.
- Musical instruments. Individuals who play certain musical instruments are at a heightened risk of developing contact dermatitis. Brass instruments including the flute, trombone, trumpet and tuba may contain common allergen metals like nickel, palladium, silver, gold and cobalt. Woodwind instruments including the saxophone, oboe, clarinet and bassoon also contain allergens like nickel and cobalt and organic compounds from exotic woods and cane reeds. String instruments, mainly violins, violas and cellos, can include metals and exotic woods, as well as rosins, propolis and staining agents known to cause an inflammatory allergic response with continued use.
Commonly identified risk factors for developing this skin condition include:
- A history of eczema
- Living in a dry climate
- Frequent hand washing
- Repeated exposure to water
- Exposure to chemicals and solvents, like fiberglass, alkalis and acids
- Having fair skin
- Wearing a diaper
- Being a landscaper, laboratory worker, nurse, hairdresser, cosmetologist, health care worker, mechanic, machinist, chef or food service worker, metal worker, or musician
16 Natural Contact Dermatitis Treatments
A definitive diagnosis requires a medical history and a physical examination. In most cases, a physician or dermatologist will be able to identify this skin condition without further testing. However, patch tests and allergy tests may be required if the allergen or irritant isn’t readily identifiable.
The most common contact dermatitis treatments in conventional medicine include:
- Hydrocortisone creams to reduce itching and redness
- Antihistamines for allergens
- Antibiotics if skin lesions or blisters become infected
- Oral steroids
However, there are also natural treatments for contact dermatitis that don’t come with common side effects of medications.
The goal is to restore and protect the skin while relieving the itching, burning and discomfort, much like proven eczema treatments. In addition, known allergens and irritants must be removed from the diet and environment to heal and prevent future outbreaks.
1. Avoid exposure to known food allergens
If you are allergic or sensitive to certain foods, avoid them. This means don’t consume them, and it also means not to handle or prepare them.
Common allergens include:
- conventional dairy
- soy
- citrus
- peanuts
- wheat
- gluten
- fish and shellfish
- eggs
- corn
- tomatoes
2. Avoid exposure to known chemical irritants and allergens
If you develop a sensitivity to a cosmetic, hair product, household cleaner, latex, metal or other compound, avoid all contact with the product to support healing and prevent further outbreaks, symptoms and rashes.
3. Eat blueberries and blackberries
Blueberries and blackberries have powerful flavonoids that exhibit strong anti-inflammatory properties known to strengthen connective tissue while reducing allergic reactions — two key things for treating contact dermatitis. Enjoy my favorite recipe for Gluten-Free Blueberry Muffins to help spur healing.
4. Omega-3 fatty acids
Boost your intake of omega-3 rich foods like mackerel, wild-caught salmon, salmon fish oil or cod liver oil, walnuts, chia seeds, and flaxseeds. Omega-3s help support skin health, cardiovascular functioning and healthy blood sugar levels; boost immune system response; lower inflammation; and ease depression while improving mood.
5. Probiotics
Boost your immune system response and help control allergies by taking a high-quality probiotic supplement and increasing consumption of probiotic-rich foods. Research shows that taking probiotics during pregnancy or early infancy can protect children against dermatitis in the future while boosting immune system response and helping control allergies.
6. Vitamin C
With its strong antihistamine properties, vitamin C may reduce symptoms of contact dermatitis for some people. As citrus is a common allergen, look for a high-quality supplement made from rose hips, and enjoy plenty of non-citrus vitamin C foods, including black currants, red peppers, green peppers, strawberries, broccoli and pineapple.
7. Collagen
Recognized as an essential element in skin health, collagen is essential during an outbreak to speed healing. According to a study published in the Journal of Cosmetic Dermatology, oral collagen supplementation significantly increases skin hydration while significantly decreasing fragmentation of skin.
Enjoy homemade bone broth, a high-quality supplement, or add a collagen-based protein powder to morning smoothies to relieve worrisome symptoms.
8. Bromelain
This powerful enzyme from pineapple reduces inflammation. Select a high-quality supplement, or purchase organic pineapples to juice.
The core has the highest concentration of bromelain and should never be discarded!
9. Quercetin
This powerful flavonoid is found in leafy greens, berries, broccoli and tomatoes, and it is known for its anti-inflammatory properties. It has been shown to support healing from inflammatory diseases.
Take 1,000 milligrams three times each day during an outbreak to reduce inflammation and allergic reactions. Select a high-quality quercetin supplement, and enjoy quercetin-rich foods like cocoa, apples, cherries, berries, leafy greens, and black and green tea.
10. Vitamin D
Researchers from the Department of Pediatrics at CHA University School of Medicine in Korea identified that individuals with a vitamin D deficiency are at a greater risk of developing this condition. To improve vitamin D levels, spend more time in the sun (without sunscreen) and enjoy wild-caught seafood like halibut, mackerel, eel, salmon, sardines and tuna. Foods high in vitamin D that are not ocean-based include maitake mushrooms, portobello mushrooms, raw milk and eggs.
11. Soothe and moisturize the rash
Apply a moisturizing and healing cream made from coconut oil, shea butter, soothing lavender essential oil and germ-fighting tea tree oil. Apply my DIY homemade Eczema Cream Recipe at least twice each day, or you can simply apply coconut oil.
Few things hydrate the skin, keep it soft and smooth, and support healing as well as coconut oil. Apply liberally several times each day until the lesions heal and the rash is gone. Coconut oil also has antifungal and antimicrobial properties.
Studies also indicate that urea cream can help soothe dermatitis and psoriasis.
12. Evening primrose oil
Topically, evening primrose is shown to reduce itching. In addition, researchers point to the high concentration of gamma-linolenic acid as supporting skin health by improving moisture levels, firmness and elasticity.
A study found taking 1,500 milligrams of evening primrose daily significantly improved skin health. If you are on blood thinners or have a history of seizures or schizophrenia, speak to your physician before taking evening primrose oil or applying it topically.
13. Oatmeal baths
A study published in the Journal of Drugs in Dermatology found that colloidal oatmeal, an ingredient in moisturizing creams, bath soaps, shampoos and bubble baths, is effective in treating a wide array of inflammatory skin conditions, including atopic dermatitis and eczema. Researchers attribute the healing nature of oats to the high levels of phenolic compounds.
To make a soothing oatmeal bath, blend 3 tablespoons of organic, gluten-free oats in a grinder until fine. Mix the powder into 1 cup of warm water, and stir well. Add to a warm tub of water, along with 5–7 drops of lavender oil and lie back, relax and soak for 20 to 30 minutes.
14. Damp dressings
To relieve the bothersome symptoms including itching, redness and the crust that develops when the rash weeps, cover with a warm, damp, sterile dressing. Soak a bandage in a mixture of apple cider vinegar, water and a few drops of your favorite essential oil with antibiotic qualities, like cinnamon oil, thyme oil, oregano oil or tea tree oil.
Use a wrap to secure it, and replace several times a day.
15. Apple cider vinegar
The benefits of apple cider vinegar far surpass even generational old wives’ tales. Apple cider vinegar’s proven benefits include soothing skin, reducing inflammation and fighting bacteria — all challenges associated with this condition.
Try my favorite recipe for a DIY Apple Cider Vinegar Toner for a gentle cleansing and to speed healing while protecting against fungi and bacteria that commonly attack open sores of a rash.
16. Dead Sea salt baths
A study reported in the International Journal of Dermatology found that bathing in a solution of Dead Sea salt enhances skin hydration, reduces inflammation and improves the skin barrier function. Contributing researchers believe Dead Sea salts are effective because of the high magnesium content.
Take a relaxing bath adding 1 cup of Dead Sea salt to a tub of water. If you have a localized rash, mix a couple of tablespoons with a cup of warm water, and apply gently with cotton pads. It is safe to use on the face and near mucous membranes.
Precautions
When symptoms include blisters or lesions that break open, the risk of infection and scarring increases dramatically. It is imperative that you keep the area clean and protected from bacteria and fungi.
Watch for common signs of infection, including tenderness, redness, a warmth in the rash or an elevated temperature.
Final Thoughts
- Millions people experience contact dermatitis symptoms each year in the United States. This inflammatory skin condition is responsible for 90 percent to 95 percent of occupational skin diseases, according to researchers.
- There are two main categories: allergic and irritant. The allergic group is often caused by beauty products, metals, plants, household cleaners and other substances that you have an allergy or sensitivity to. The rash tends to appear between 24 and 72 hours after exposure.
- The irritant category is typically caused by chemical compounds and environmental factors, like cold, trapped moisture and dry climates.
- It is not contagious, and natural contact dermatitis treatments typically resolve the rash and symptoms within a few weeks. Health care workers, landscapers, musicians, food service workers, mechanics and those who work with chemicals are at a greater risk of developing this skin condition.
- To speed healing and prevent additional outbreaks, avoid foods that you are allergic to, as well as common allergens like seafood, soy, dairy, wheat, gluten and corn. Avoid products with chemicals that you know will cause a rash. Many chemicals hide in beauty products and household cleaning products. An allergist can help you narrow down the culprit if you don’t know what is causing the symptoms.
- Take care to avoid scratching as this can cause an infection and scarring. Keep affected areas clean and moisturized with an organic compound like coconut oil.