This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Graves’ Disease: 7 Ways to Help Manage Hyperthyroid Symptoms
December 19, 2015
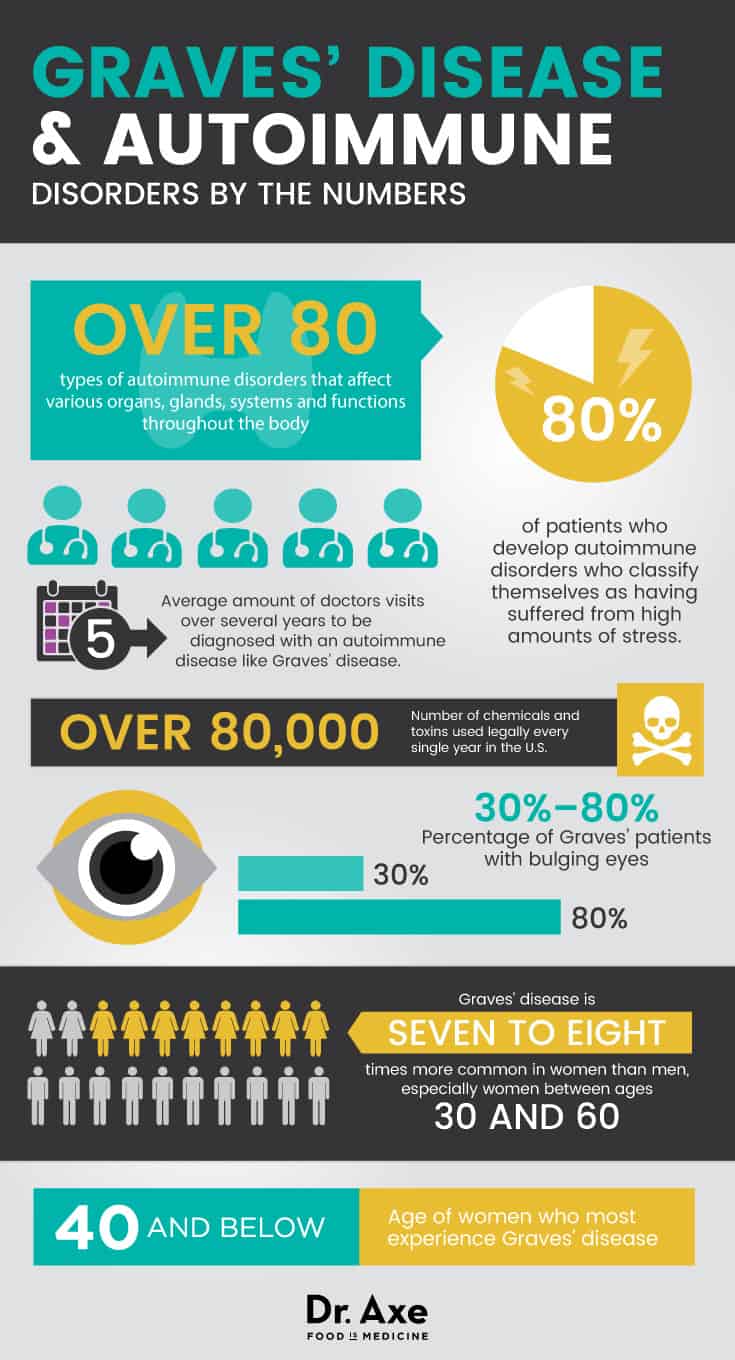
Did you know that there are over 80 different types of autoimmune disorders that affect various organs, glands, systems and functions throughout the body? Graves’ disease is a common autoimmune disorder characterized by an overproduction of thyroid hormones.
The thyroid is considered one of the most important endocrine glands in the body, since it produces hormones that affect nearly every aspect of life: hunger, sleep, reproduction, energy levels, metabolism, body weight and more. You may have heard more about disorders caused by hypothyroidism, since they tend to be more common than hyperthyroid disorders. Hypothyroid conditions cause the thyroid to be underactive, meaning it doesn’t produce enough thyroid hormones.
In the U.S., Graves’ disease is the No. 1 cause of hyperthyroidism, or an overactive thyroid gland. (1) So, what is Graves’ disease, and how can you treat this common thyroid issue naturally?
What Is Graves’ Disease?
Graves’ disease was first identified by Irish physician Robert Graves about 150 years ago. (2) Graves’ disease symptoms can vary a lot depending on the individual and how severe the disorder has become. Because the thyroid gland has such widespread and important roles in the body, symptoms of Graves’ disease are usually very apparent and can affect overall well-being and health in many different ways. Graves’ disease is an autoimmune disorder that affects the entire thyroid gland and results from the overproduction of thyroid hormones, known as thyrotoxicosis.
In the medical world, an autoimmune disorder is considered a chronic illness, having no permanent cure and needing to be controlled over time through various lifestyle changes and sometimes medications, too. The primary goal of controlling Graves’ disease is to stop the overproduction of thyroid hormones, which helps lower Graves’ symptoms, including trouble sleeping, weight loss, eye bulging (known as Graves’ orbitopathy) and personality changes. (3)
As you’ll come to learn, managing stress is one of the most important ways to fight autoimmune disorders, since some studies find that up to 80 percent of patients who develop autoimmune disorders classify themselves as having suffered from high amounts of stress!
It can be hard to diagnose and treat Graves’ disease because many people who have symptoms of abnormal thyroid activity also experience symptoms that can confused with other disorders. Some studies have found that for someone to be diagnosed with an autoimmune disorder like Graves’ disease, it usually requires the patient to visit an average of five doctors over the course of several years, causing a lot of uncertainty and grief in the process.
So it’s often a stressful road to arrive at a diagnosis of Graves’ disease, but fortunately many people are able to help control the disorder well once they make certain adjustments to their diets, stress levels and lifestyles.
How Graves’ Disease Develops
Normally, thyroid-stimulating hormone (TSH) is released by the pituitary gland in the brain and usually determines how much hormones the thyroid produces. But people with Graves’ disease experience a break in normal communication between the pituitary glad and thyroid gland, resulting in abnormal antibodies being released that mimic TSH and therefore cause too much thyroid hormone to be circulated into the bloodstream.
These antibodies are called thyroid stimulating immunoglobulin (TSI) and thyrotropin receptor antibody (TRAb). TSI cells have a similar effect to TSH, which we need in adequate amounts to help the thyroid function normally. But TSI antibodies cause the thyroid gland to produce excess thyroid hormones above and beyond what is necessary and healthy.
Since the thyroid mistakes these antibodies for TSH, they can override normal signals sent from the pituitary gland and therefore cause hyperthyroidism. As TSI and TRAb levels rise, inflammation increases, which indicates that the immune system is working on overdrive and accidentally attacking the body’s own healthy tissue. A harmful cycle can develop in people with Graves’ disease because the more active the immune system becomes, the more bodily tissue is damaged and then more activated T-cells and auto-antibodies are released.
We produce several different kinds of thyroid hormones normally, including the types called T3 and T4. Compared to healthy people without autoimmune or thyroid disorders, on a blood test people with Graves’ disease show abnormally high levels of T3 and T4, low TSH, and a high presence of TSI antibodies.
Some of the most noticeable effects of Graves’ disease are changes in someone’s weight, mood and appearance. That’s because hormones secreted by the thyroid gland control your metabolism — meaning your body’s ability to use nutrients and calories from the food you eat in order to have enough energy. You’ve likely heard and noticed that genetics play a big part in determining someone’s body weight. That’s because thyroid gland activity is somewhat hereditary — therefore so is the rate of someone’s metabolism. The metabolic rate is determined by the amount of available circulating thyroid hormones. So when the thyroid gland secretes an overabundance of these hormones, the metabolism can shoot up and cause weight loss, anxiousness and irritability.
A link also has been identified between Graves’ disease and another thyroid disorder known as Hashimoto’s thyroiditis. Hashimoto’s is the most common cause of hypothyroidism and, like Graves’ disease, it’s also an autoimmune disorder. Hashimoto’s can sometimes develop after taking antithyroid medication as a treatment for Graves’ disease as the medication causes the thyroid to slow production of thyroid hormones and move towards hypothyroidism. (4)
Conventional Treatment of Graves’ Disease
Many people with Graves’ suffer from physical feelings associated with anxiety, including fast heartbeat (or “pounding heart”), increased sweating, trembling, changes in appetite, trouble with digesting food normally and difficulty getting good sleep. Your physician will likely refer you to an endocrinologist, or hormone specialist, to diagnose these symptoms and develop a treatment plan.
There are three standard conventional treatment options for Graves’ disease: (5)
-
-
- Antithyroid medications: The two most common medications used to treat Graves’ disease are methimazole (MMI; brand name: Tapazole) and propylthiouracil (PTU). Antithyroid medication works by limiting the amount of thyroid hormones released into the body. It can result in hypothyroidism. Methimazole can cross the placental membrane, risking harm to the developing fetus, therefore pregnant women are cautioned to speak with their doctor before taking, or continuing to take, this medication. No adverse effects have been found in nursing infants, but it’s best to consult your doctor before breastfeeding while taking this medication. Propylthiouracil can be used during the first three months of pregnancy but should only be used if needed. It is not recommended during the last six months of pregnancy. Check with your doctor before breastfeeding.Your endocrinologist may also prescribe other medications to manage symptoms of Graves’ disease such as anxiety, palpitations, heat intolerance, sweating and tremors. These medications may include beta-blockers, calcium channel blockers and central-acting agents.
- Radioactive iodine (RAI) therapy: A treatment involving the administration of radioactive iodine, which destroys the cells that make up the thyroid gland. This procedure results in hypothyroidism and requires lifelong treatment with the medication levothyroxine to replace the thyroid hormone. A loss of taste sensation and damage to salivary glands, resulting in dry mouth, may occur. RAI is not recommended for pregnant patients.
- Thyroidectomy (surgical removal of the thyroid gland): Surgical removal of the thyroid gland also results in hypothyroidism and includes the added risk of other complications such as vocal cord nerve damage and hypoparathyroidism. Surgery is not as common as it once was now that medication and RAI are available options.
-
There is controversy surrounding the best way to manage the disease. Each case is individual, requiring a discussion between the patient and her endocrinologist. Each option has its own risks and benefits and none is particularly ideal. The choice of treatment plan may also be impacted by other factors such as patient preference; geographical location and availability of health care services (such as access to certain treatments); whether or not the patient is pregnant; and the potential impact of co-existing morbidities. (6)
Natural Treatment for Graves’ Disease
1. Manage Stress Levels
Several studies, involving both humans and animals, show that stress can ignite autoimmune reactions and worsen inflammation. That’s probably why such a high percentage of Graves’ disease patients report having experienced trauma or chronic stress before developing the disease. Research demonstrates that stress causes both physical and psychological changes that impact how the immune system works, causing a downstream of neuro-endocrine alterations that can wind up leading to autoimmune disorders and tissue damage. (7)
Stress can raise levels of cortisol and adrenaline, which disturb neurotransmitter function and worsen symptoms of thyroid disease. To keep stress from aggravating Graves’ disease, build stress-reducing practices into your day, including natural stress relievers such as: exercise, meditation, prayer, spending time in nature, using essential oils, massage therapy, acupuncture or volunteering for a good cause.
2. Eat an Anti-inflammatory Diet
Reducing inflammation through a healthy diet is one of the best ways to enhance immune function, create a healthy gut environment and manage your autoimmune symptoms. Inflammation can partially be traced to an unhealthy gut “microbiota” that is caused by nutrient deficiencies, food allergies or sensitivities, which all raise autoimmune activity. (8)
Some of the ways that your diet might trigger autoimmune reactions include eating common allergens like gluten and dairy products, which the immune system can actually register as a threat when they aren’t digested properly. Allergens can contribute to leaky gut syndrome, in which small particles leak out into the bloodstream through tiny openings in the gut lining, triggering autoimmunity.
A well-rounded diet that’s filled with anti-inflammatory foods and free from toxin overload helps resolve bacterial imbalances in the gut that make symptoms worse.
Focus on limiting or avoiding foods capable of aggravating autoimmune disorders, including:
It’s also important to avoid foods that are high in iodine as it increases levels of thyroid hormone. These include foods such as iodized salt, egg yolks and seaweed. For this same reason, avoid certain herbs and plants, including bladderwrack (a sea plant). Some herbs also have thyroid-stimulating properties, such as ashwaganda. Speak with your natural health care practitioner or herbalist before taking herbal supplements.
Foods that can help control Graves’ disease symptoms include:
-
-
-
-
- fresh vegetables/green juices: these provide vital nutrients and fight inflammation
- fresh fruit: a great source of antioxidants and electrolytes, but avoid processed fruit juices
- anti-inflammatory herbs: basil, rosemary, parsley and oregano are all anti-inflammatory
- spices like tumeric, garlic and ginger: known to help boost immune system function
- bone broth: helps heal the gut and improve detoxification
- probiotics: balance bacteria within the digestive tract and fight leaky gut syndrome
- healthy fats including omega-3s: lower inflammation and helps with neurotransmitter functions
-
-
-
3. Get Some Exercise
Exercise is a great way to help control stress and lower inflammation, as long as it’s enjoyable and doesn’t involve overtraining, which may make you even more irritable. Do some sort of exercise daily that makes you feel happier, less anxious and hopefully helps you sleep. Soothing exercises that can work well include dancing, yoga, cycling or swimming. Listening to music while exercising is another great way to “get into the zone” and feel more relaxed afterward. (9)
Another reason to eat a nutrient-rich diet and to exercise is to help protect your bones, since having a thyroid disorder already interferes with your ability to maintain bone strength. Having very high levels of thyroid hormone interferes with your body’s normal ability to incorporate calcium or other minerals into your bones. This means you need to do whatever you can to lower bone loss in other ways. Strength training, including doing bodyweight exercises at home, helps keep bones strong as you age.
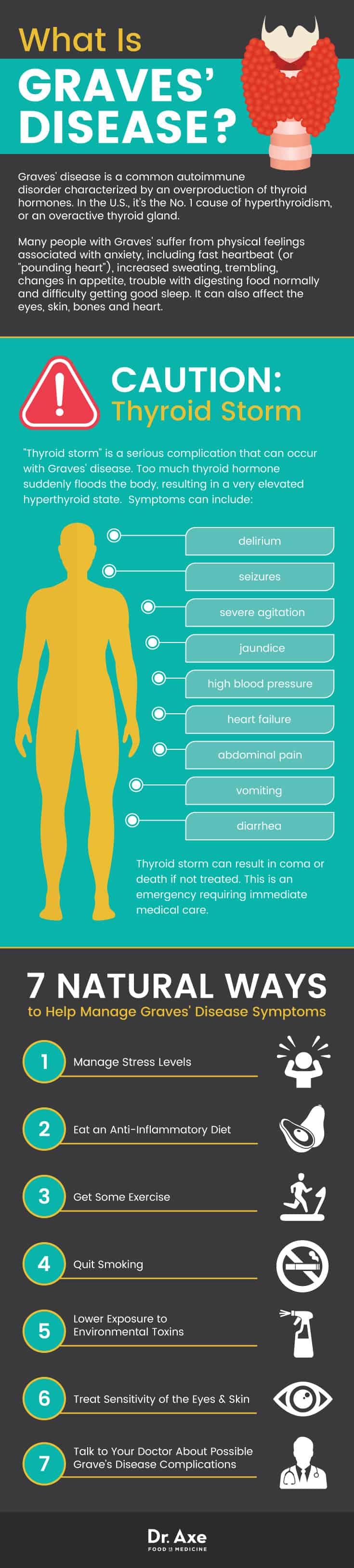
4. Quit Smoking
Cigarette smoking and exposure to tobacco and other recreational drugs has been found to be a potential trigger for autoimmune disorders, including Graves’ disease. It’s not exactly clear how cigarettes might make Graves’ disease worse, but it’s very likely that the high amount of toxins present in cigarettes (and other drugs) raises inflammation, damages healthy cells and tissue, and therefore activates the immune system to release more T-fighter cells. (10)
5. Lower Exposure to Environmental Toxins
Most of us come into contact with various chemical or environmental toxins multiple times every single day. There are over 80,000 chemicals and toxins used legally every single year in the U.S. in common household or beauty products, chemically-sprayed crops, prescription medications, birth control pills, and antibiotics. These can all wind up accumulating in the water supply and elsewhere, making their way into our homes and bodies.
I recommend buying organic produce as much as possible, using natural household products (including essential oils), avoiding unnecessary medications however you can, and drinking high-quality water that’s been filtered to eliminate chlorine and fluoride.
6. Treat Sensitivity of the Eyes and Skin
If you develop Graves’ complications in the eyes or on the skin, there are some simple remedies you can try at home to ease inflammation and pain. One particular complication that can occur with this disease is Graves’ ophthalmopathy, also known as Graves’ orbitopathy, which causes the eyes to bulge and can cause vision problems. It can also cause dry, puffy eyes, sometimes with a sensation of grittiness. Try using a cool compress pressed against your eyes to keep them moisturized, as well as applying lubricating eyes drops. Also, always wear sunglasses when outdoors, since sensitive eyes are more prone to damage from ultraviolet rays. If your eyes become puffy overnight, try raising your head while you’re sleeping to keep blood and fluid from building up around your face. (11)
If Graves’ affects your skin, you can use soothing essential oils combined with coconut oil to fight itchiness, swelling and reddening. Essential oils that are gentle and anti-inflammatory include lavender, frankincense, rose and tea tree oil.
7. Talk to Your Doctor About Potential Graves’ Disease Complications
There are certain complications that develop when Graves’ disease is untreated. This is especially true if you’re pregnant, have other forms of inflammatory diseases or if you suffer from another autoimmune disorder.
If you’re pregnant, it’s important to get Graves’ under control since it raises the risk for miscarriage, preterm birth, fetal thyroid dysfunction, poor fetal growth, maternal heart failure and preeclampsia (high blood pressure). If you have a history of heart disease or complications, Graves’ disease can lead to heart rhythm disorders, changes in the structure and function of the heart muscles, and even lead to possible heart failure in some rare cases. Also, because the high thyroid hormone levels can impact bone density, it’s important to discuss the risk of osteoporosis (weak, brittle bones) with your doctor as well.
While there’s plenty you can do on your own to lower Graves’ disease risks and symptoms, always make sure to get professional help if you notice symptoms worsening suddenly or you’re under a lot of stress/anxiety, which can trigger a relapse. Luckily, if it’s treated, and at least mostly resolved, Graves’ disease isn’t likely to cause permanent damage or lead to other disorders.
Graves’ Disease Signs and Symptoms
Some of the most common signs and symptoms of hyperthyroidism caused by Graves’ disease include: (12)
-
-
-
-
- changes in mood, including irritability and anxiousness
- muscle pains and weakness
- weight loss despite normal or increased appetite
- trouble sleeping, restlessness and sometimes insomnia
- a fast heartbeat
- sensitivity to heat and changes in temperature
- digestive problems, including diarrhea
- tremor of the hands or fingers
- an increase in perspiration or warm, moist skin
- enlargement of the thyroid gland (goiter)
- irregular periods
- erectile dysfunction or reduced libido
- changes in skin texture, including thickening of the skin on the lower legs or red bumps (called Graves’ dermopathy, or pretibial myxedma)
- eye problems, including bulging of the eyes (known as Graves’ orbitopathy or Graves’ ophthalmopathy), which affects a high percentage of Graves’ patients (some studies show about 30 percent to 80 percent) (13)
- pain in the eyes, red eyes, sensitivity to light or vision loss (a less common complication than eye bulging)
-
-
-
Who’s at the biggest risk for developing Graves’ disease? While autoimmune disorders of all kinds can affect both men and women, younger people and the elderly, and people of all nationalities, Graves’ disease is believed to be much more common among women, especially younger women who are below the age of 40. (14) In fact, thyroid disorders and autoimmune disorders in general usually impact women much more than men, which is believed to be the case partially because women’s hormones are more susceptible to changes caused by stress. Graves’ disease is seven to eight times more common in women than men, especially women between ages 30 and 60.
For some people, Graves’ disease can go into remission or even disappear completely after several months or years of living with the disease. Usually, however, it won’t go away on its own without making changes, and it’s important to track the disease since left untreated it can sometimes cause serious complications, just like other autoimmune disorders (such as diabetes). This includes the potential for a rare but very serious and life-threatening complication of Graves’ disease: “thyroid storm,” which is also called thyrotoxic crisis.
Thyroid storm is basically an extreme form of hyperthyroidism, in which symptoms suddenly become worse due to a flooding of thyroid hormones into the body. This excess amount of thyroid hormone may be the result of radioactive iodine therapy or too much thyroid hormone replacement.
Symptoms of thyroid storm can include: (15)
-
-
-
-
- vomiting
- diarrhea
- high blood pressure
- jaundice
- seizures
- delirium
- severe agitation
- abdominal pain
- heart failure
-
-
-
Thyroid storm can lead to coma or death if not treated. If you experience these symptoms, get emergency medical help immediately.
There is also a greater risk of thyroid cancer, particularly papillary thyroid cancer, among individuals with Graves’ disease. (16) Even though a cancer diagnosis is scary, thyroid cancer is usually very treatable, most often by surgical removal (thyroidectomy).
Causes of Graves’ Disease
How does this autoimmune disease develop and manifest in the body? Graves’ disease is not the only reason that someone might produce more thyroid hormone than normal, but it’s one of the most common reasons. Like other autoimmune disorders, there isn’t a clear-cut cause for Graves’ disease, but rather people are believed to develop Graves’ due to a combination of several factors, which can include: a genetic predisposition, a poor diet, high stress levels and exposure to certain environmental toxins. (17)
Someone who has a family member with Graves’ disease is more likely to be affected, since there seems to be certain genes that increase the chances of developing Graves’. Many experts also believe that autoimmune disorders of all kinds can be triggered by high amounts of chronic stress in someone’s life or a traumatic episode. Other risk factors include having poor immune function and frequent infections, pregnancy, being a smoker/using drugs, or having another autoimmune disease (such as diabetes or rheumatoid arthritis, two of the most common autoimmune conditions).
Graves’ disease develops when the immune system experiences changes in levels of antibodies, which is usually kicked off by high levels of inflammation. The human immune system is designed to respond to a wide variety of “threats,” some that are actually harmful and some that are not. Normally, the immune system’s protective mechanisms keep us free from diseases or infections caused by bacteria, viruses, fungi or cell mutations, but in people with autoimmune disorders, overactivity of the immune system starts to actually harm the body and affect healthy cells, organs and glands.
In an attempt to protect the body from perceived threats (like toxins found in a poor food supply or within the environment), the immune system can raise levels of antibodies, also called “fighter cells,” which look for anything in the body that seems unusual or dangerous. (18) Graves’ is a type of autoimmune disorder with an “organ specific immune response,” meaning these fighter cells begin to attack a specific location in the body (the thyroid gland in this case) instead of raising inflammation throughout the body.
Graves’ Disease Takeaways
-
-
-
-
- Graves’ disease is a form of hyperthyroidism, in which the thyroid produces too much thyroid hormone. Symptoms can include: anxiety, changes in mood; changes in skin texture; goiter; bulging eyes; tremor; muscle pain and weakness; heart palpitations; digestive issues; and insomnia, among others.
- Thyroid storm is a rare, but very serious, episode of hyperthyroidism that requires immediate medical attention. It is life-threatening and can lead to coma or death if not treated quickly.
- Conventional treatment includes medication, radioactive iodine therapy and surgery.
- Certain lifestyle changes can go a long way in helping to resolve symptoms whether you choose to take antithyroid medications or not.
- You can find additional information by visiting the American Thyroid Association online.
-
-
-











