This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Pancreatitis Symptoms: 11 Natural Ways to Prevent & Manage
November 8, 2017
Every year in the United States 210,000 people are admitted to hospitals with acute pancreatitis and 56,000 people are hospitalized each year due to chronic pancreatitis. This is a serious condition that can result in death if not treated properly and promptly. (1, 2)
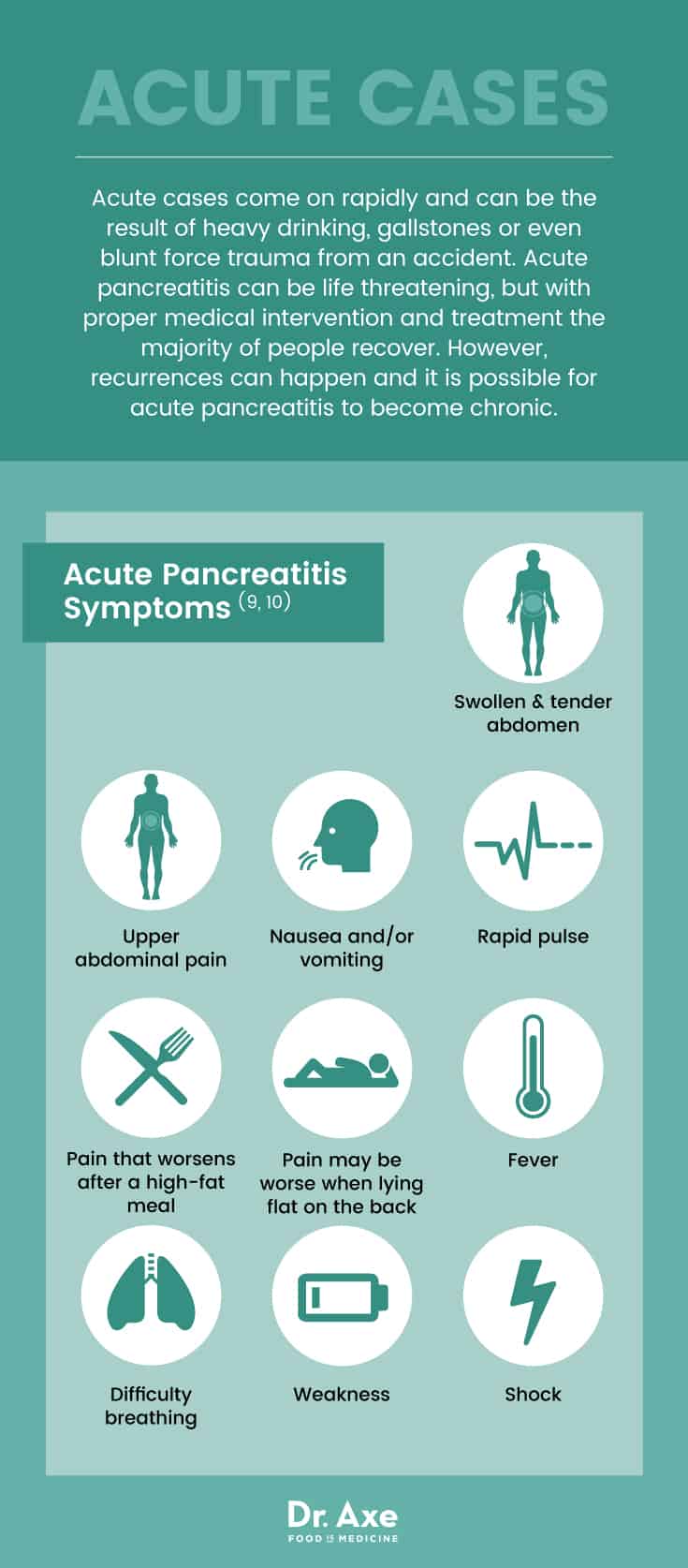
The symptoms of pancreatitis depend on whether it is an acute or chronic case. Acute cases come on rapidly and can be the result of heavy drinking, gallstones or even blunt force trauma from an accident. Acute pancreatitis can be life-threatening, but with proper medical intervention and treatment the majority of people recover. However, recurrences can happen and it is possible for acute pancreatitis to become chronic.
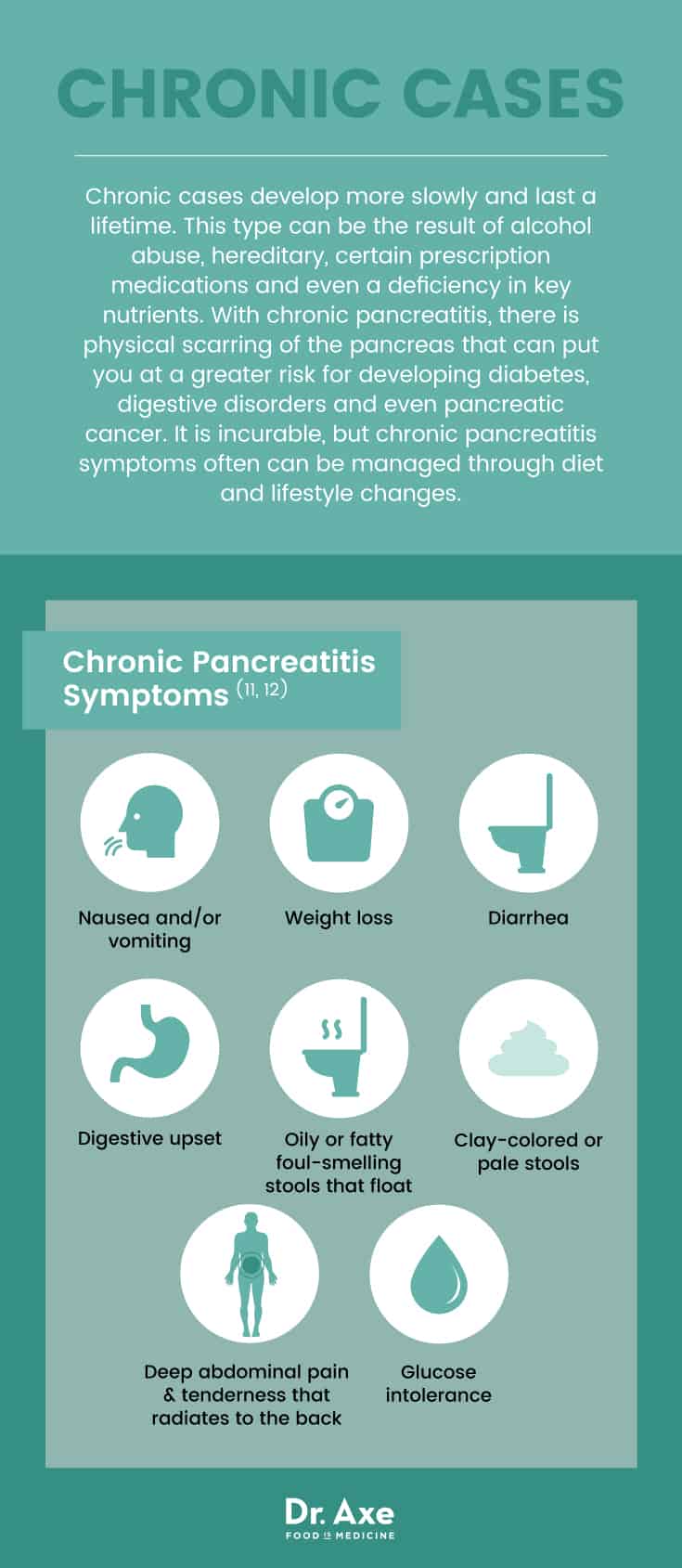
Chronic cases develop more slowly and last a lifetime. This type can be the result of alcohol abuse, hereditary, certain prescription medications and even a deficiency in key nutrients. With chronic pancreatitis, there is physical scarring of the pancreas that can put you at a greater risk for developing diabetes, digestive disorders and even pancreatic cancer.
Diagnosing this condition requires a thorough examination and often multiple tests. The severity and the type will determine the course of action. For acute cases, a few days on clear liquids may resolve the problem, while more severe cases may require surgical intervention. For chronic pancreatitis, adjusting the diet and finding ways to manage the pain and discomfort is typical. However, antibiotics, IV hydration and nutritional support may be required.
Natural treatments can help with pancreatitis symptoms and may help prevent future episodes. And there are even some natural treatments that may help protect against pancreatic cancer.
What Is Pancreatitis?
Pancreatitis is an inflammation of the pancreas, which is a small organ tucked in the upper abdomen behind the stomach and in front of the spine. The pancreas is responsible for converting food to fuel, aiding in digestion by producing essential enzymes to break down fats and carbohydrates and creating two vital hormones, insulin and glucagon. (3)
There are two main types of pancreatitis: acute and chronic.
Acute: Acute pancreatitis symptoms come on suddenly and may last only a few days. The enzymes that are normally released remain in the pancreas, causing it to become inflamed and swollen. This slows digestion, causes pain and is associated with some severe complications that can become life-threatening. (4)
Chronic: This form is incurable. The severity and frequency of chronic pancreatitis symptoms vary from person to person. Worsening symptoms are often linked to eating a large high-fat meal or drinking alcohol. As the disease continues to create scar tissue and damage the pancreas, the risk for certain conditions like diabetes and pancreatic cancer increases. In addition, the body can start to have a difficult time processing and absorbing nutrients causing vitamin deficiencies.
More rare forms of this disease include childhood pancreatitis and autoimmune pancreatitis.
Childhood Pancreatitis: This condition is considered fairly rare and is most often found in children with cystic fibrosis or after a physical trauma. In some cases, the anatomy of the ducts in the liver or pancreas may cause this disease in children. Anti-seizure medications, certain antibiotics and chemotherapy may also cause childhood pancreatitis. However, in nearly one-third of cases a cause will not be identified. (6)
Autoimmune Pancreatitis: Sharing many of the same symptoms as both chronic and acute, here the inflammation is caused by the body’s immune system attacking the pancreas directly. This condition is broken into two types, Type 1 can affect multiple organs while Type 2 affects only the pancreas. Autoimmune pancreatitis is rare and newly-recognized disease that can be misdiagnosed as pancreatic cancer. (7)

A Note About Pancreatic Cancer
Because of the location of the pancreas, pancreatic cancer is often not diagnosed until late stages when it begins to spread to other organs. If you have been diagnosed with any form of pancreatitis and experience any of the symptoms below, please consult with your doctor immediately about your concerns. Chronic pancreatitis is considered a risk factor for this cancer. (8)
- New diagnosis of diabetes
- Unintended weight loss
- Weight loss and diabetes co-occurring
- Jaundice
- Pain in the upper abdomen
- Loss of appetite
- Depression
- Blood clots
- Fatigue
Pancreatitis Signs & Symptoms
Pancreatitis symptoms vary from person to person, and whether it is acute or chronic.
Acute Pancreatitis Symptoms: (9, 10)
- Swollen and tender abdomen
- Upper abdominal pain
- Nausea and/or vomiting
- Rapid pulse
- Pain that worsens after a high-fat meal
- Pain may be worse when lying flat on the back
- Fever
- Difficulty breathing
- Weakness
- Shock
Chronic Pancreatitis Symptoms: (11, 12)
- Nausea and/or vomiting
- Weight loss
- Diarrhea
- Digestive upset
- Oily or fatty foul-smelling stools that float
- Clay-colored or pale stools
- Deep abdominal pain and tenderness that radiates to the back
- Glucose intolerance
Causes & Risk Factors
Pancreatitis occurs when digestive enzymes become activated while in the pancreas, irritating the cells, causing inflammation and scarring. There are a number recognized causes for pancreatitis including: (13)
- Alcohol use and abuse. Long-term or a single binge can inflame the pancreas.
- Gallstones
- Surgery of the abdomen, heart or lungs where the blood supply to the pancreas is temporarily cut off.
- Certain medications including azathioprine, sulfonamides, corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics
- Cigarette smoking.
- Cystic Fibrosis
- Family history of pancreatitis
- High levels of calcium in the blood
- High triglyceride levels in the blood
- Infection like the mumps, hepatitis, rubella, Epstein Barr or cytomegalovirus
- Blunt force trauma to the abdomen
- Pancreatic cancer
- Deficiency in nutrients, including A, C, E, selenium and carotenoids
The following conditions indicate a higher risk for developing pancreatitis symptoms:
- Biliary tract disease
- Binge alcohol use
- Chronic alcohol abuse
- Recent surgery
- Family history of high triglycerides
- Being 35 to 64 years old
- Smoking
- Being African-American
Conventional Treatments
There is no single test that can detect pancreatitis. When symptoms arise, you doctor will order a variety of tests that may include:
- Blood tests to check for elevated levels of pancreatic enzymes.
- Stool tests to measure levels of fat that may suggest the digestive system isn’t absorbing fats as needed.
- CT scan to look for the level of inflammation and to identify gallstones.
- Abdominal ultrasound to look at the inflammation in the pancreas and gallstones.
- Endoscopic ultrasound to look for blockages in pancreatic or bile ducts and surrounding inflammation.
- MRI to identify abnormalities in the pancreas, ducts and gallbladder.
Once diagnosed, treating pancreatitis requires medical intervention as complications can occur. Mild cases of acute pancreatitis may go away without treatment, but severe acute cases can cause life-threatening complications and require hospitalization. (14)
Treatment protocols will be determined based on the type, the symptoms that are presenting, and the severity of symptoms. For acute cases, once hospitalized, fasting will provide the pancreas the opportunity to recover. Once the inflammation is under control, clear liquids and bland foods will be introduced. If inflammation persists, a feeding tube may be required to ensure that the patient is receiving adequate nutrition.
Pain, sometimes severe, is common and treatment for both acute and chronic forms often includes prescription pain medications.
- To prevent dehydration, patients are often provided fluids through an IV.
- If necessary, a surgical procedure may be required to remove obstructions.
- Enzymes may be prescribed to improve digestion and nutrient absorption.
- Ongoing treatment will include recommendations for small low-fat meals that are nutrient-dense.
Research shows that treatment plans differ depending on many factors, including whether pancreatitis is hereditary or acquired. (15)
11 Natural Ways to Prevent & Manage Pancreatitis Symptoms
A severe pancreatitis attack can be life-threatening; seek emergency medical attention as quickly as possible. Chronic pancreatitis symptoms often can be managed through diet and lifestyle changes. Also, if you’re at-risk for pancreatitis, making some of these changes may help prevent the development of pancreatitis.
- Improve your diet.
- Try alternative therapies for pain.
- Address nutrient deficiencies.
- Supplement with vitamins A, C, D, E and K.
- Boost omega-3 fatty acids.
- Add a probiotic supplement to your diet.
- Drink green tea.
- Add a rhodiola supplement to your diet.
- Try a reishi mushroom supplement.
- Try grape seed extract.
- Include foods high in glutamine in your diet.
1. Improve Your Diet. Diet plays a huge role in the development of pancreatitis, as well as the severity of symptoms and recovery. Follow the food recommendations below to help prevent pancreatitis. (16)
Foods to Avoid:
- Eliminate all suspected food allergens including dairy, soy, wheat, corn, food preservatives and chemical food additives.
- Eliminate all stimulants including caffeine, alcohol and tobacco.
- Dramatically reduce or eliminate all trans-fatty acids in the diet.
Foods to Enjoy:
- Focus on small, low-fat meals that emphasize fresh fruits, vegetables, lean proteins and whole grains, avoiding any foods that cause sensitivities or allergies.
- Add healthy oils like olive oil and coconut oil.
- Enjoy lean meats including grass-fed beef, organic poultry and cold-water fish.
- Enjoy foods high in iron like spirulina, organic grass-fed beef liver, lentils and even dark chocolate.
- Add more antioxidant-rich foods like cherries, blueberries, tomatoes and bell peppers to the diet.
2. Alternative Therapies for Pain. Pain, often severe, is common for both types of pancreatitis. The Mayo Clinic recommends the following alternative therapies to help ease the pain and discomfort. (17)
- Meditation. In addition to easing pain, meditation fights depression and anxiety, lowers cortisol levels, improves mental performance and aids in recovery from chronic illnesses. (18)
- Relaxation. The symptoms of pancreatitis cause discomfort, pain and often anxiety. Incorporating effective relaxation techniques like breathing exercises can help with the symptoms.
- Acupuncture. Used for thousands of years for a wide array of physical and mental ailments, acupuncture is a safe and effective way to reduce chronic pain.
- Yoga. In addition to pain, a recent study focusing on patients with chronic pancreatitis found that biweekly yoga for 12 weeks significantly improved stress, mood, appetite, overall feelings of well-being and alcohol dependence. (19)
3. Address Nutrient Deficiencies. According to research, there is a causal link between certain nutrient deficiencies and the development of pancreatitis. A simple blood test to determine if you are deficient in vitamins A, C or E as well as selenium and carotenoids can help you make wise dietary choices.
4. Vitamin Supplements: In a review of clinical trials published in the journal Advances in Nutrition, researchers found that bioactive vitamins A, C, D, E and K all show promise for pancreatic cancer intervention. (20)
- Vitamin A. Aids in pancreatic cancer prevention and is an essential nutrient for strong bones and immune function. Incorporate plenty of vitamin A-rich foods like beef liver, carrots and sweet potatoes into your diet.
- Vitamin C. Slows tumor growth. Take 1–6 milligrams daily, but never take a vitamin C supplement and vitamin B12 supplement together as they affect each other’s absorption. If diarrhea occurs, back off until tolerated. Include vitamin C-rich foods that you tolerate well like red bell peppers, black currants, guava, and even broccoli in your diet.
- Vitamin D. Shows anti-proliferative effects and repression of cancer cells in the pancreas and, more importantly, a study has found that it reduces inflammation and fibrosis in pancreatitis. (21) With pancreatitis, try to get 15–30 minutes each day of sunshine, without sunscreen, to increase vitamin D levels in your body. In addition, focus on cold-water fish like halibut, mackerel and salmon in your diet.
- Vitamin E. Shown to inhibit tumor cell growth and helps protect against heart disease. A high-quality vitamin E or, even better, foods like sunflower seeds, almonds and hazelnuts are recommended.
- Vitamin K. Shown to inhibit pancreatic tumor cells, which is imperative for those with chronic pancreatitis. If well-tolerated, aim for 300 micrograms of vitamin K through organic foods like dandelion greens, mustard greens or Swiss chard.
5. Omega-3 Fatty Acids: Adding 1 to 2 tablespoons each day of a high-quality omega-3 fatty acid supplement is shown to reduce inflammation and improve immunity. In a meta-analysis published in the journal Nutrients, supplementation reduced the risk of mortality, infectious complications, and reduced the length of hospital stays for pancreatic patients. Authors encouraged large-scale multi-center randomized clinical trials. (22)
6. Probiotics. Adding a high-quality probiotic supplement for those with acute pancreatitis is shown to reduce intestinal inflammation, organ dysfunction and pancreatitis symptoms. Take 50 billion CFUs of probiotics daily while symptoms persist for best results. The introduction of probiotics will also help rebuild health gut function during and after a round of antibiotics. (23, 24)
7. Green Tea. According to a recent study, regular consumption of green tea inhibits the development and the progression of pancreatic cancer. Researchers note that for women this results in a 32 percent reduction in pancreatic cancer risk, and they also note that a lower temperature of the tea is linked to its benefits. (25)
8. Rhodiola. This powerful adaptogen herb that has been shown to enhance energy and boost brain power has also been shown to improve kidney and pancreas function in rats. Take 350 milligrams to 500 milligrams of rhodiola twice a day for immune system support and to help with symptoms of pancreatitis. (26)
9. Reishi Mushroom. Used in holistic medicine practices, a recent study on chronic pancreatitis found that Ganoderma lucidum (the scientific name for reishi mushroom) increased the abundance of beneficial bacteria. And researchers noted this study shows potential for use of this mushroom as a possible therapy for chronic pancreatitis. Take 150 milligrams to 300 milligrams twice a day to help relieve inflammation while boosting immune system response. (27)
10. Grape Seed Extract. There are over 30 studies on grape seed extract and pancreatitis. Many of these studies cite its protective nature, particularly against cancer cells. Also noted is its anti-inflammatory effect and ability to fight against oxidative stress. Take 100 milligrams to 300 milligrams daily of a high-quality supplement. (28)
11. Glutamine. According to a study published in the journal Pancreatology, glutamine is associated with a significant reduction in the length of hospital stays and a decrease in complications for patients with acute pancreatitis. Add three servings of foods rich in L-glutamine like bone broth, grass-fed beef and cottage cheese, aiming for a total of 8–12 grams each day. (29)
A special note on Ghrelin, Leptin and Melatonin. These three hormones are noted in research to significantly reduce the severity of pancreatitis symptoms and protect pancreatic tissue from inflammatory damage. Learning how to improve your levels of ghrelin and leptin can be helpful. Resist restricting calories, get plenty of sleep and manage stress, avoid processed foods and eat plenty of protein to optimize your levels. (30)
Precautions
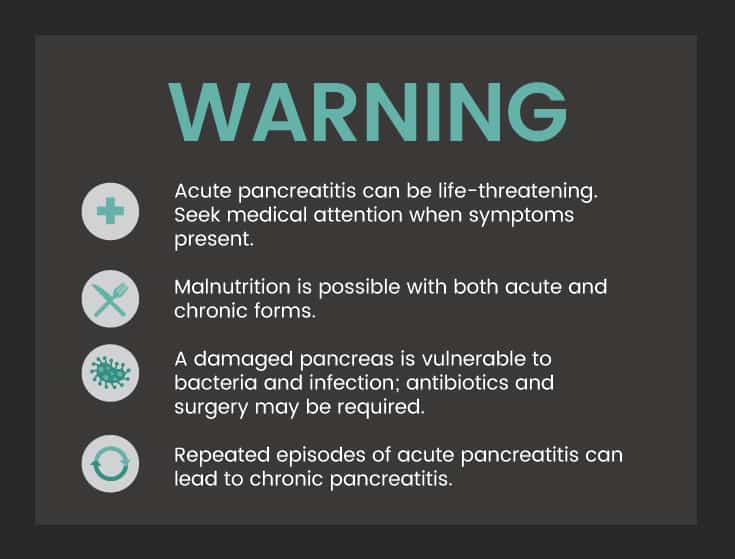
- Acute pancreatitis can be life-threatening. Seek medical attention when symptoms present.
- Chronic pancreatitis is associated with an increased risk for developing diabetes and pancreatic cancer.
- Malnutrition is possible with both acute and chronic forms.
- A damaged pancreas is vulnerable to bacteria and infection; antibiotics and surgery may be required.
- Acute pancreatitis can cause fluid and debris to develop pockets in the pancreas causing internal bleeding and infection.
- Repeated episodes of acute pancreatitis can lead to chronic pancreatitis.
Key Points
- Chronic pancreatitis is incurable; managing pancreatitis symptoms, including pain, through diet and natural treatments is recommended.
- Acute pancreatitis may come on suddenly. While it can resolve in a few days, it can also cause complications that are life-threatening.
- Recognized causes of pancreatitis include: heavy alcohol use, gallstones, genetics, smoking, blunt force trauma or injury to the abdomen, and certain nutrient deficiencies.
- Symptoms of acute pancreatitis include: nausea and/or vomiting, abdominal pain that radiates to the back, fever and an elevated pulse rate.
- Symptoms of chronic pancreatitis include: unintended weight loss, new diagnosis of diabetes, diarrhea, oily foul-smelling stools and abdominal pain.
- Diagnosis often requires multiple laboratory and imaging tests; a delayed diagnosis complicates treatment and therapy.
- Chronic pancreatitis increases the risk for pancreatic cancer and diabetes.
- IV fluids, pain medications, antibiotics, enzyme supplements and surgery may be required.
11 Natural Ways to Prevent & Manage Pancreatitis Symptoms
- Improve your diet.
- Try alternative therapies for pain, such as yoga and acupuncture.
- Address nutrient deficiencies.
- Supplement with vitamins A, C, D, E and K.
- Boost omega-3 fatty acids.
- Add a probiotic supplement to your diet.
- Drink green tea.
- Add a rhodiola supplement to your diet.
- Try a reishi mushroom supplement.
- Try grape seed extract.
- Include foods high in glutamine in your diet.








