This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Fetal Alcohol Syndrome Signs + Prevention
March 7, 2018

Researchers first identified alcohol as a fetal toxin only in the early 1970s, after an association was made between fetal exposure to alcohol during pregnancy and certain physical and mental impairments. (1) Today fetal alcohol syndrome (FAS) and related fetal alcohol spectrum disorders (FASD) are considered prevalent, life-long disabilities that are difficult and costly to treat.
How common are fetal alcohol syndrome and fetal alcohol spectrum disorders?
A February 2018 study published in the Journal of the American Medical Association (JAMA) aimed to answer the question “How common are fetal alcohol spectrum disorders in the United States?” Findings from the study suggested that recent rates of fetal alcohol syndrome spectrum disorders in the U.S. are much higher than previous estimates.
The study included more than 13,100 first-grade children from four regions of the United States. (2) The children were examined for symptoms related to FASD, including: dysmorphic features, impaired physical growth and/or impaired neurobehavioral development. When it was suspected that a child had symptoms due to FAS, the child’s mother was also asked to answer survey questions about her use of alcohol during pregnancy. It was found that between 1 percent to 5 percent (and possibly up to 10 percent) of the children surveyed were believed to be affected by some type of FAS disorder, depending on the community they lived in.
What Is Fetal Alcohol Syndrome?
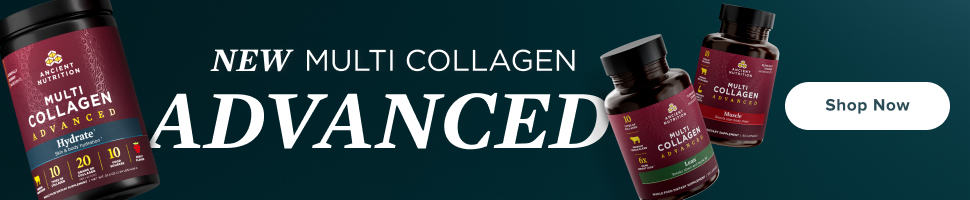
Alcohol is considered “a physical and behavioral teratogen,” or an agent that causes malformations of an embryo. (3) According to the National Organization on Fetal Alcohol Syndrome,”Fetal Alcohol Syndrome (or FAS) is a disorder resulting from prenatal exposure to alcohol” (in other words, caused by maternal consumption of alcohol during pregnancy). It is characterized by abnormalities in three domains: (4)
- Growth deficiency
- Central nervous system dysfunction resulting in neurobehavioral disorders
- A specific pattern of facial abnormalities
Slightly different than FAS are fetal alcohol spectrum disorders (FASD). When a fetus is exposed to alcohol prenatally, but does not have identifiable deficits in all three domains required for an FAS diagnosis, then they might be diagnosed with a fetal alcohol spectrum disorder instead.
Fetal Alcohol Spectrum Disorders:
Fetal alcohol spectrum disorders occur on a spectrum, also called a continuum (similar to how autism or attention deficit disorders occur). FAS has somewhat been replaced by the FASD classification system that specifies whether the effects of fetal exposure to alcohol are only physical, only related to the development of the nervous system or brain, or a combination of both.
Below are the different types of fetal alcohol spectrum disorders:
- Partial fetal alcohol syndrome (pFAS) — When a person does not meet the full diagnostic criteria for FAS but has a history of prenatal alcohol exposure and some abnormalities as a result.
- Fetal alcohol effect (atypical FAS) — Used to describe effects of fetal alcohol exposure with an incomplete picture of nonspecific physical and psychological manifestations.
- Alcohol-related birth defects (ARBD) — This describes physical birth defects that are caused by prenatal alcohol exposure.
- Alcohol related neurodevelopmental disorder (or ARND, sometimes also called neurobehavioral disorder associated with prenatal alcohol exposure)— This describes impairments to the nervous system and abnormal neurological functioning. While ARBD and ARND are not considered to be the same as a diagnosis of FAS, their symptoms and effects can be just as severe.
Signs & Symptoms of Fetal Alcohol Syndrome
How does fetal alcohol syndrome affect a child?
Can fetal alcohol syndrome be deadly?
- Neurodevelopmental abnormalities and neurological impairment. Alcohol is one of the leading causes of mental deficiency in the world and neurological problems are the leading cause of disability in children with fetal alcohol spectrum disorders. Central nervous system dysfunction due to FAS can affect intelligence, activity and attention, learning and memory, language and motor abilities, and behavior. (6)
- Nonfebrile seizures.
- Deficient brain growth and dysmorphogenesis (abnormal tissue formation) of the brain. The most common impact of infant growth retardation is small head circumference. Microcephaly of the brain (when the baby’s head is smaller than expected) can also occur, along with tissue loss, cerebral malformation, and abnormalities of neuronal migration. In severe cases the brain might fail to divide into two hemispheres and abnormalities of the corpus callosum, brainstem and the cerebellum can develop.
- Poor growth, including related to a child’s height and weight.
- Abnormalities of organ development.
- Facial abnormalities, especially affecting the upper lip and eyes. Facial abnormalities can include short palpebral fissures, increased distance between the eyes, a flattened face with a short nose, and a bow-shaped mouth with a thin upper lip.
- Developmental delay and difficulty learning.
- Abnormalities in glucose metabolism.
- Increased motor activity and alterations in orientation.
- Rarely, hearing disorders, eye abnormalities, and congenital abnormalities may occur.
Fetal Alcohol Syndrome Causes & Risk Factors
As the name implies, fetal alcohol syndrome is alcohol-related. But what amount of alcohol during pregnancy is too much, and which types of behaviors in regards to alcohol consumption increase the risk for a child developing FASD?
- Alcoholic drinks — meaning all types including beer, wine, hard cider and liquor — can be toxic during pregnancy because they contain ethanol. Ethanol is a “clear, colorless liquid rapidly absorbed from the gastrointestinal tract and distributed throughout the body.” (7) It taxes the liver, blocks absorption of certain nutrients, affects blood sugar and has other negative effects.
- In regards to how much alcohol during pregnancy is OK, The National Organization on Fetal Alcohol Syndrome states on their website “Prenatal Alcohol Exposure: No safe amount. No safe time. No safe alcohol. Period.”
- Generally speaking, most experts think that pregnant women should avoid all alcohol. But some experts have stated that very small amounts, about a half glass to one glass of wine per week for example (or even several drinks per week), have not been proven to be harmful. A 2012 study of more than 1,600 Danish 5-year-old children concluded that “This study did not observe significant effects of low to moderate alcohol consumption during pregnancy on executive functioning at the age of 5 years.” (8) Still, overall women who are pregnant are advised to completely abstain from consuming all alcohol.
- Certain studies have found that that there is “no relation between maternal drinking and neurodevelopmental outcome with a threshold intake of less than 15 mL (0.5 ounces) of absolute alcohol per day, but above this level, infants of mothers older than 30 years of age were two to five times more likely to be functionally impaired than those of younger mothers.” (9)
- Research also shows that significant birth defects primarily occur in infants whose mothers drank more than five drinks per occasion, an average of at least once a week.
- One study found some evidence that low alcohol consumption (about one drink per day or less) may be unlikely to cause FAS, and that FAS depends on high blood alcohol levels. The researchers concluded that the number of drinks consumed at a time is more important than the average alcohol consumption. (10) However, authorities still encourage pregnant women to avoid even small amounts.
Although alcohol is commonly consumed around the world, even by adults who mostly live healthy lifestyles, alcohol is still a drug. When consumed in high amounts, especially within a short period of time, alcohol can even cause poisoning and be deadly. To understand how alcohol affects the body, just consider the symptoms of alcohol poisoning: repeated vomiting, seizures, loss of coordination and balance, hypothermia, confusion, slowed breathing and even death.
How does drinking alcohol during pregnancy affect a mother’s developing fetus?
Here are some of the negative effects that alcohol has on both a pregnant woman and her child:
- Blocks absorption of important minerals, including zinc (zinc deficiency is a co-teratogen with alcohol)
- Depletes choline, which is essential for fetal brain development
- May contribute to too much weight gain during pregnancy, and potentially metabolic problems like gestational diabetes
- Negatively impacts cholesterol homeostasis
- Interferes with expression of vitamin-associated genes, especially those related to retinoic acid, niacin, vitamin D and folic acid intake
- May contribute to iron deficiency
- Alcoholism may also alter a woman’s appetite and result in low protein and low calorie intake, which doesn’t supply enough energy for growth and development
- Can cause low birth weight in infants and make nursing more difficult (some FAS babies tend to consume less breastmilk and suffer from nutrition-related problems)
- Negatively impacts infants’ sleep-wake patterns and leads to restlessness and mood-related problems
- Can change a child’s responses to alcohol in the future, even when they grow to a teenager or adult
Who is most likely to get fetal alcohol syndrome?
Risk factors for fetal alcohol syndrome and fetal alcohol spectrum disorders include:
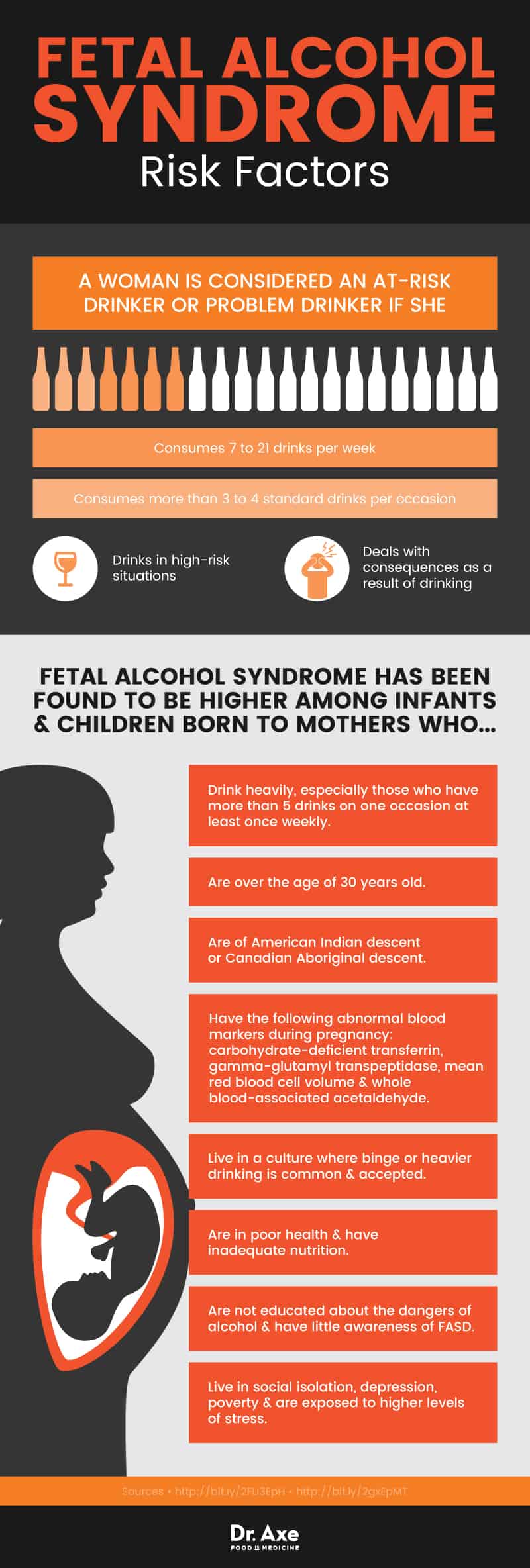
Fetal alcohol syndrome has been found to be higher among infants and children born to mothers who: (11)
- Are heavy drinkers, especially those who engage in binge/heavy drinking that involves having more than five drinks on one occasion at least once weekly.
- Are over the age of 30 years old.
- Are of American Indian descent or Canadian Aboriginal descent.
- Have the following abnormal blood markers during pregnancy: carbohydrate-deficient transferrin, gamma-glutamyl transpeptidase, mean red blood cell volume and whole blood-associated acetaldehyde. One study found that all mothers who consumed at least 29.6 mL of alcohol per day had at least one of these markers, and all of the mothers’ infants were born with abnormal heights, weights and head circumferences. (12)
- Are in poor health and have inadequate nutrition.
- Living in a culture where binge or heavier drinking is common and accepted.
- Have no education about dangers of alcohol and little awareness of FASD.
- Live in social isolation, depression, poverty and are exposed to higher levels of stress.
Diagnosis & Conventional Treatments for Fetal Alcohol Syndrome
How Is Fetal Alcohol Syndrome Diagnosed?
As of 2016 guidelines for diagnosing fetal alcohol spectrum disorders, sponsored by the National Institute on Alcohol Abuse and Alcoholism, have been updated to include information from the latest research findings. The most recent guidelines include precise definitions about prenatal alcohol exposure and the symptoms it can cause. Below are some of the key points from the FASD diagnosis guidelines: (13)
- To be diagnosed with fetal alcohol syndrome or partial fetal alcohol syndrome, a child must display signs of neurobehavioral plus cognitive or behavioral impairment. Following neurodevelopment and neuropsychology assessment, a child must be at least 1.5 standard deviations below the mean for their age group.
- Prenatal exposure is assessed by the amount of maternal alcohol intake per occasion and timing of consumption during pregnancy.
- Physical characteristics related to birth defects, malformation and problems with growth and development are also assessed (called a dysmorphology evaluation). Children who are diagnosed with FASD must be in the lowest 10th percentile for height, weight, head circumference, and palpebral fissure length based on their age.
Can fetal alcohol syndrome be cured?
Experts stress that in order to give a child with FASD the best chance of managing their condition and progressing as they age, early recognition of FASD is important to maximize functional outcomes. A child with FAS may struggle with certain impairments throughout adulthood, although many treatment options can help. Below are some of the ways that experts try to prevent and treat fetal alcohol syndrome:
- Primary care clinicians (such as a pregnant woman’s OB-GYN) are encouraged to routinely screen for alcohol use. Doctors are advised to speak about alcohol use even with women of childbearing age who are not pregnant.
- Once a woman becomes pregnant, her doctor should discuss preconceptual health with her in detail, including giving her information about avoiding drugs, alcohol, and other dangerous products or behaviors during pregnancy. It’s also important for pregnant women, or those trying to conceive, to learn about eating a healthy pregnancy diet to support their baby’s growth and development.
- For women who wish to avoid pregnancy, especially if they are dealing with a drug or alcohol problem, they should have access to contraceptive counseling and help with family planning.
- If needed, a woman who is pregnant or trying to conceive should be given a referral to substance abuse programs if a drug or alcohol use disorder is diagnosed.
Natural Symptom Management for Fetal Alcohol Syndrome
1. Optimizing Development from a Young Age
When FAS or FASD is diagnosed, early childhood intervention can help to prevent secondary disabilities and to improve quality of life. It’s recommended that parents provide their infant or child with help as soon as possible if FAS is suspected. The parent can work with a professional to receive special care and guidance in managing behaviors.
- Allowing an infant or child to get enough sleep and rest is important for managing their moods and energy levels.
- A healthy diet is also critical for supporting development. Ideally infants will be breast-fed for at least six months and young children will be slowly introduced to healthy whole foods. Stimulating, inflammatory foods like sugary snacks, juices and soda, processed meats, caffeine and refined grains should be avoided or limited. Allergens (like dairy, wheat, peanuts, tree nuts, eggs and shellfish) should also be avoided if these cause any distress.
- Parents and caregivers can learn to take cues from their baby in order to properly handle and comfort them. They are encouraged to gently stroke and coddle their infants, to make frequent eye contact, and to use soft, soothing words since the infants can be startled easily. Sudden, startling movements, aggressive handling, yelling and bouncing should be avoided.
- A routine (eating, napping, play time, etc.) should be established as early as possible.
2. Managing Behavioral Difficulties
What type of psychological disorders can result from FAS? Children with FAS or FASD can struggle with delayed motor and speech development, decreased cognitive abilities, difficulties with interpersonal relationship skills, attention deficits, hyperactivity and impulsive behaviors (similar to those found in children with attention deficit hyperactivity disorder (ADHD).
- Counselors and health care providers are encouraged to work with children with FAS to develop appropriate interpersonal behaviors so the children can learn in a way that promotes self-worth and self-esteem by building on the child’s strengths.
- Parents and caregivers should also be involved in the process and given information about what to expect from the infant or child regarding their academic performance, attention, relationship skills and behavior.
- It helps for the child to have an organized schedule and routine to prevent feeling overwhelmed or unfocused. Parents and teachers may create a checklist of daily “to dos,” place a chart on the wall, or give other reminders.
- Regular physical activity, breaks, and playtime and prevent burnout and poor moods.
- Time to be creative can help burn off steam and improve self-confidence. This can include time for artwork, painting, sketching, music, dancing, etc.
- As the child gets older a healthy diet is still very important for cognitive development, mood management and preventing spikes and dips in energy.
3. Providing Appropriate Help in School
Some children with FAS will struggle with learning impairments in language and number processing, hearing and speech problems, and olfactory difficulties — all of which makes schoolwork more difficult. While there’s some evidence that children with FAS have mostly normal IQs, they have a higher risk of dealing with poor short-term memory problems, difficulty establishing routines, decreased academic performance, problems with verbal memory, defects in spatial memory, and poor retention of learned tasks.
- Counseling/therapy and tutoring are two options that may help children with FASD advance in school. Cognitive problems (poor attention, short term memory, flexibility and planning) may improve with help from a school psychologist or special-needs therapist.
- As part of an educational intervention, academic expectations might need to be scaled down.
- Learning can be improved by enhancing a child’s self-image, which is also helpful for preventing acting out.
- Teachers can help their students with FAS by giving clear directions, keeping tasks simple, using concrete examples, and giving one direction or assignment at a time.
Fetal Alcohol Syndrome Prevention
There are two prongs to fetal alcohol syndrome prevention: identifying women who are drinking while pregnant and reducing their consumption.
1. Community/Patient Education
- The very best way to prevent FAS is through education, whether in classrooms (such as in high schools or universities/colleges) or through community-outreach fetal alcohol syndrome prevention programs. One aim is to change attitudes toward drinking in young people of school age, in order to make them understand how this affects their fertility and future offspring.
- Women can also be educated by their doctors, who can help prevent FAS by encouraging their patients to avoid consuming alcohol before conception and throughout pregnancy. Medical practitioners are typically taught that they should recommend abstinence from alcohol starting with their patients’ first prenatal visit.
- Many women hoping to become mothers aren’t aware that drinking alcohol can even reduce her chance of getting pregnant and also increase her risk of having a miscarriage. How early does alcohol affect a fetus? During the earliest stages of pregnancy, such as in the first six to eight weeks, avoiding alcohol is important because this is a time period when the fetus is developing very fast. Alcohol can block the absorption of certain essential minerals and start to cause damage just when the fetus is starting the mature.
2. Screening
- Another important aspect of fetal alcohol syndrome prevention is identifying high-risk pregnant women who are struggling with drinking. The goal is to help reduce, or ideally to end, their consumption of alcohol (and use of other drugs).
- If possible, it’s best for high-risk women to be screened before pregnancy occurs, allowing for early intervention and enough time to change their habits.
- Primary care physicians, midwives or nurse practitioners should all ask their patients about their drinking habits and offer help if needed. A woman is considered an at-risk drinker or problem drinker is she consumes seven to 21 drinks per week; consumes more than three to four standard drinks per occasion; drinks in high-risk situations and deals with consequences as a result of drinking. (14)
3. Intervention
- If a pregnant woman is unable to stop drinking, it’s important that she is promptly referred for alcohol treatment.
- Advice may be given to the woman’s spouse, family and friends who are closest to her in order to help her stop drinking. An intervention might need to take place in order to admit the pregnant woman into a rehab program or for her begin professional therapy.
- If stress is contributing to a woman’s drinking, then she should strongly consider incorporating stress relieving activities into her life like: meditation, yoga, exercise, joining a support group or spiritual community, journaling and therapy.
- If an expecting mother eats a nutrient-dense diet during pregnancy this may be able to protect against some of the effects of alcohol. It’s important for all expecting moms to consume enough protein, iron, folate, fiber and antioxidants.
4. Therapy
- Expecting mothers who find it hard to stop drinking while pregnant should consider seeing a cognitive behavioral therapist, or another type of therapist, who can help with managing stress, dealing with underlying psychological problems and decision making.
- If depression is an underlying cause of an alcohol problem, then this should be addressed. Besides seeking therapy, natural ways to cope with depression include: exercise, eating a healthy diet, meditation, use of supplements, and support from loved ones or a support group.
Key Points About Fetal Alcohol Syndrome
- Fetal alcohol syndrome (or FAS) is a disorder resulting from prenatal exposure to alcohol. It causes abnormalities in growth, central nervous system dysfunction or neurobehavioral disorders and facial abnormalities.
- Fetal alcohol spectrum disorders (FASD) can be diagnosed if a fetus is exposed to alcohol prenatally, but does not have identifiable symptoms in all three domains required for an FAS diagnosis.
- Other symptoms of FAS and FASD can include poor growth (below normal height and weight), abnormalities of organ development, developmental delay and difficulty learning, hyperactivity, hearing disorders, eye abnormalities and poor relationship skills.
- Ways to prevent fetal alcohol syndrome include: educating and screening pregnant women, community outreach, educating students about FAS in high school and college, intervention programs when necessary, and therapy for substance abuse.
- Symptoms of fetal alcohol syndrome can be managed by diagnosing a child with FAS as early as possible, being patient with the child’s development and academic achievement, school counseling, therapy and special classroom instruction.