This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Shorter Life Expectancy in the U.S.: 8 Reasons (and Solutions!)
December 17, 2019

Did you know that the U.S. is spending nearly twice as much on health care than other developed, high-income countries, but we have a lower life expectancy?
Recent data, published in November of 2019, highlights that U.S. life expectancy has actually decreased since 2014, after it continued in rise after 1959.
And research conducted in 2018 by the Harvard T.H. Chan School of Public Health, the Harvard Global Health Institute and the London School of Economics establishes that although U.S. citizens are paying much more than our peer countries on things like prescription drugs, diagnostic tests, physician’s salaries and administrative costs, our average life expectancy in the U.S. is still years lower.
So what’s to blame for the shorter life expectancy rates in the United States? It may be hard to believe, but evidence shows that the U.S. is at a health disadvantage, despite our hefty spending on healthcare. Researchers are pointing to social factors and lifestyle choices playing major roles in our lower life expectancy rates.
Maybe we need to take some advice from the happiness study that suggests social connections and good relationships can boost our happiness and health. Or we can take a look at the blue zones, where the life expectancy is up to 100 years because individuals practice natural life extenders.
We can keep spending our hard-earned money on pharmaceuticals, procedures and testing, but if we don’t change the day-to-day habits that affect our health and take a deeper look at what’s not working in the U.S., it won’t matter much.
What Is Life Expectancy?
“Life expectancy” refers to the number of years that a person can expect to live based on a statistical average. This number is estimated by evaluating the average age of death among people of the same population, and it will vary from geographical area and era.
To determine the life expectancy of a particular group or population, researchers must track a group of people that were born in the same year and indicate the average age-at-death in order to predict the mortality rate.
But the tricky part is that life expectancy rates also take into account observed improvements in mortality, so researchers must be able to project death rates for future years as well.
Life expectancy depends on a particular person or population’s access to:
- healthcare
- lifestyle choices
- dietary choices
- economic status
These factors, however, certainly aren’t set in stone and actually changes throughout the course of your life.
Life expectancy is the average age that a person will die, which means that most people aren’t going to live exactly that long. Some will die earlier and some will live later than the predicted life expectancy, but it gives us an idea of a certain population’s health.
Plus, once you’ve hit a certain age, your life expectancy is expected to be higher. For instance, the life expectancy of a 30-year-old adult may be a few years less than the life expectancy of an adult over the age of 65 because he or she has already lived through years that are associated with risk factors.
The Latest Study Findings
An analysis published last month in JAMA found that U.S. life expectancy decreased for three consecutive years after 2014. For the most part, researchers suggest that the reduced life expectancy is due to excess deaths among young and middle-aged adults.
From 2010-2017, the increase in midlife mortality was associated with an estimated 33,307 excess deaths. Researchers also found that by 2014, the midlife death rate increased across all racial groups. The causes of death in this age group were:
- drug overdoses
- alcohol abuse
- suicides
- organ system diseases
On top of that, the analysis indicates that the largest relative increases in midlife mortality rates occurred in New England, in states including New Hampshire, Maine, Vermont, Ohio, West Virginia, Indiana and Kentucky.
Life Expectancy in the U.S. vs. Other Countries
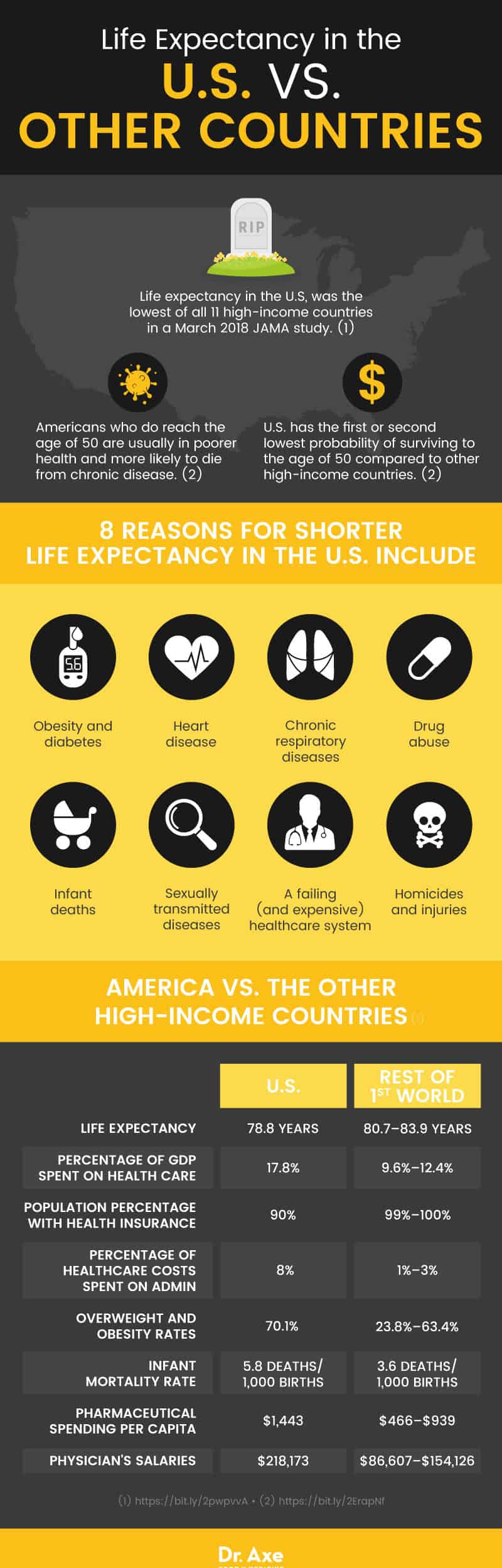
The March 2018 report published in JAMA found that life expectancy in the U.S. was the lowest of all 11 high-income countries included in the research, such as the United Kingdom, France, Germany, the Netherlands, Sweden, Switzerland, Denmark, Australia, Japan and Canada.
Life expectancy in the U.S. was 78.8 years, while the life expectancy range in our peer countries was between 80.7 and 83.9 years.
According to a report published by the National Academy of Sciences, among other high-income countries, the U.S. has had the first or second lowest probability of surviving to the age of 50.
Plus, Americans who do reach the age of 50 are usually in poorer health and face greater morbidity and mortality from chronic diseases than older adults of peer countries. This is generally due to risk factors that arise earlier in life, like obesity, diabetes and smoking.
8 Reasons (and Solutions!) for Shorter Life Expectancy in the U.S.
1. Obesity and Diabetes
The U.S. has the highest percentage of adults who are overweight or obese, at about 70 percent of the population being affected, while peer countries have rates that range from 23.8 percent to 63.4 percent of the population. And research shows that American adults aged 20 years and older have the highest prevalence rates of diabetes among peer countries.
Although Americans are less likely to smoke than citizens of our peer countries, and even drink alcohol less heavily, they consume the most calories per person. Plus, patterns of food consumption in the U.S. is very much shaped by environmental factors, including actions made by food and agriculture industries, and the foods that are being offered at our grocery stores and restaurants.
To treat obesity naturally, and eliminate this preventable reason why we have a shorter life expectancy in the U.S., focus on bringing whole, nutrient-dense foods into your diet and cutting out sugary, processed and packaged foods.
That dietary change alone can make a huge difference, and can add 12 years to your life, or more! People with diabetes need to follow a diabetic diet plan that will help to reverse the disease naturally.
2. Heart Disease
According to a 2013 report entitled U.S. Health in International Perspective, the death rate in the U.S. from ischemic heart disease is second highest among 17 peer countries.
The report explains that “Americans reach age 50 with a less favorable cardiovascular risk profile than their peers in Europe, and adults over age 50 are more likely to develop and die from cardiovascular disease than are older adults in other high-income countries.”
To reduce the prevalence of coronary heart disease, it’s important to adjust your diet, reduce stress levels and exercise regularly. It’s also important to get five heart disease tests that will help you to better predict your risk of heart disease. These tests include an EKG, a limited CT scan and three blood tests.
3. Chronic Respiratory Diseases
Research published in JAMA indicates that chronic respiratory diseases, including COPD and asthma, are causing a substantial health and financial burden in the U.S. In 2015, chronic respiratory diseases were the fifth leading cause of death in this country.
The World Health Organization suggests that chronic respiratory disease rates may be caused by environmental factors, like air pollution and unhealthy housing, poor indoor air quality, smoking and occupational exposure to chemicals and dusts.
Although this may be a bigger environmental issue than you can improve on your own, you can work to improve COPD and asthma symptoms by avoiding exposure to smoke, pollution, irritants and allergens, improving your diet and maintaining a healthy weight.
4. Drug Abuse
Compared to our peer countries, Americans lose more years of life because of drug abuse. According to the Centers for Disease Control and Prevention, death by unintentional injuries, which includes drug overdose, has become the third leading cause of death in 2016, right behind heart disease and cancer.
The rate of unintentional injuries increased by 9.7 percent from 2015 to 2016, with 64,000 drug overdose deaths occurring in 2016. Statistics show that the sharpest increase occurred among deaths related to fentanyl and fentanyl analogs (synthetic opioids).
So what’s to blame for the opioid epidemic? Researchers believe it’s the use of prescription painkillers, which serve as a gateway for other addictive opioid drugs, like heroin.
In fact, research published in the New England Journal of Medicine shows that 63 percent of people who have been prescribed opioid drugs, typically for the treatment of chronic pain, have reported misusing them.
To reduce and hopefully end opioid addictions and the U.S., the CDC recommends starting with the biggest risk factor — the high amount of opioid painkillers that are being prescribed. Plus, the country could benefit from increased access to substance abuse treatment services and professionally trained therapists.
5. Infant Deaths
The infant mortality rate is the highest in the U.S., at 5.8 deaths per 1,000 live births, compared to other high-income countries, with a rate of 3.6 per 1,000 infant deaths.
According to the CDC, the leading causes of infant death in the U.S. are birth defects, low birth weight due to preterm birth, sudden infant death syndrome, maternal pregnancy complications and injuries.
To lower the U.S. infant death rate, the CDC recommends addressing social, behavioral and health risk factors that contribute to infant mortality. This includes improving perinatal care in the U.S., educate new parents about the risk of SIDS and accidental injuries during infancy, and building maternal and child support through health agencies and institutions.
You can find more information on the CDC website under their Division of Reproductive Health.
6. Homicides and Injuries (Especially from Gun Violence)
Researchers at the National Academy of Sciences state “since the 1950s, U.S. adolescents and young adults have died at higher rates from traffic accidents and homicide than their counterparts in other countries.”
Risk factors like not fastening your seatbelt, drinking while driving and using illicit drugs are reducing the U.S. life expectancy.
Plus, research shows that American citizens own more firearms than their peers in other countries. The U.S. has dramatically higher rates of death from violent injuries when compared to peer countries, especially injuries from firearms.
In 2003, the U.S. homicide rate was 6.9 times higher than other high-income countries and the rate of firearm homicides was 19.5 times higher. And these numbers have stayed pretty consistent since then, according to the National Institute of Justice.
The National Institute of Justice indicates that “a key lesson learned from several decades of gun violence intervention programs is that sustained federal-local partnerships improve effects to reduce gun violence within a city or community.”
7. Sexually Transmitted Infections
It appears that adolescents in the U.S. are less likely to practice safe sex than those in other high-income countries. Plus, U.S. citizens are becoming more sexually active at an earlier age and they have more sexual partners.
This may explain why STDs are on the rise in America and may be contributing to our national health disadvantage.
The U.S. has the highest incidence of AIDs among other high-income countries and the prevalence of chlamydia, gonorrhea and syphilis continue to rise, with more than 2 million new cases of these STDs being reported in 2016. And this doesn’t include the number of STD cases that aren’t reported.
A lack of access to healthcare and education are both contributing to the high prevalence of STDs in this country. Plus, behavioral choices pertaining to safe sex are also contributing to the problem.
The dangers of fracking in America now includes STDs, too. A 2018 Yale study published in the journal PLOS ONE found that compared to Ohio counties with no shale gas (fracking) activity, counties with fracking recorded 21 percent higher rates of chlamydia and 19 percent higher rates of gonorrhea.
Fracking operations often involve work camps full of out-of-state workers, increasing STD infection rates through sexual mixing patterns associated with labor migration, according to the study authors.
8. A Failing Healthcare System?
Research suggests that our current healthcare system may be at least partially to blame for the health disadvantage in the U.S..
Some weaknesses in the system that may impact the health of our citizens and life expectancy in the U.S. are the practice of defensive medicine instead of preventative medicine, the misalignment of physician and patient incentives and limited access to good quality healthcare for many people living in this country.
Of course, our healthcare system alone is not solely responsible for our lower life expectancy because lifestyle, behavioral, social, environmental and economic factors also play a major role.
Final Thoughts
- The life expectancy in the U.S. is 78.8 years, while it ranges from 80.7 to 83.9 years in other high-income countries. This estimation does not align with the fact that Americans are spending almost double on healthcare compared to peer countries.
- Recent research has actually found that the U.S. life expectancy rate has decreased since 2014, which is due to excess deaths among young and middle-aged adults of all races.
- Clearly, spending more money on healthcare doesn’t lead to a longer, healthier life in the U.S. So what can we do to increase the life expectancy in America? Research suggests that promoting healthy lifestyles, strengthening our health, social and educational systems, and working to design healthier environments can make an impact.
- Many of the reasons why our life expectancy is lower in the U.S. is because of preventable conditions that are caused by behavioral and lifestyle choices. The eight reasons for shorter life expectancy in the U.S. include:
- Obesity and diabetes
- Heart disease
- Chronic respiratory diseases
- Drug abuse
- Infant deaths
- Homicides and injuries
- Sexually transmitted diseases
- A failing (and expensive) healthcare system?









