This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Valley Fever: 8 Natural Tips to Help Prevent This Soil-Borne Illness
July 1, 2018

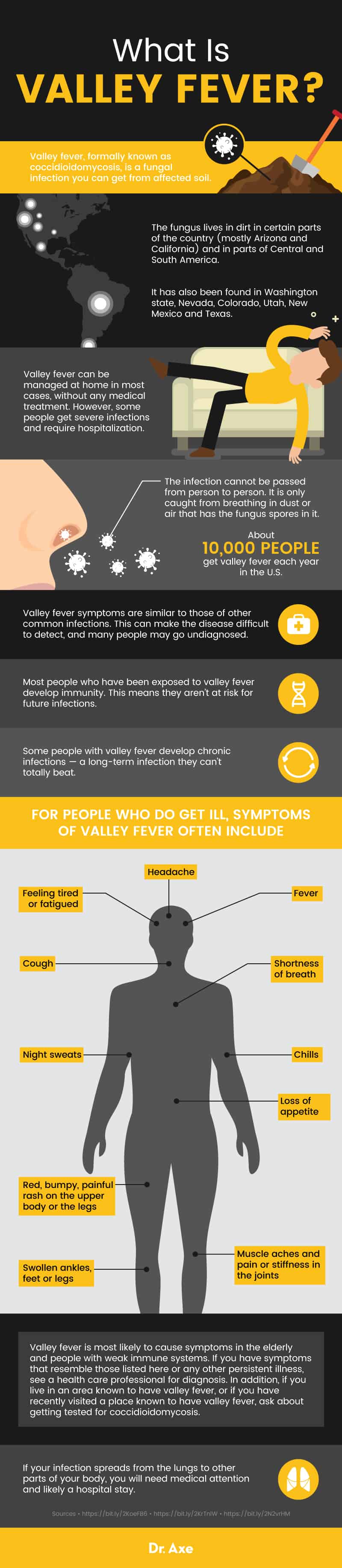
Valley fever is a fungal infection that is most common in the Southwestern United States and parts of Central and South America. The fungus lives in the soil and can cause the infection when you breathe in dust or fungal spores in the air. The disease is also called coccidioidomycosis.
Valley fever can be managed at home in most cases, without any medical treatment. However, some people get severe infections and require hospitalization. The best way to protect your health is to learn about the disease and how you can manage valley fever symptoms.
What Is Valley Fever?
Valley fever, formally known as coccidioidomycosis, is a fungal infection you can get from affected soil. The fungus lives in dirt in certain parts of the country (mostly Arizona and California) and in parts of Central and South America. It has also been found in Washington state, Nevada, Colorado, Utah, New Mexico and Texas.
The infection cannot be passed from person to person. It is only caught from breathing in dust or air that has the fungus spores in it.
According to the Centers for Disease Control and Prevention (CDC), about 10,000 people get valley fever each year in the United States. In most cases, people recover on their own in a few weeks or months. Some people need a prescription antifungal treatment to speed recovery or manage symptoms, and others develop a serious lung infection that requires hospitalization. (1)
Most people who have been exposed to valley fever develop immunity. This means they aren’t at risk for future infections. However, some people with valley fever develop chronic infections — a long-term infection they can’t totally beat. These people may have valley fever symptoms, such as a cough or low-grade fever and other flu- or tuberculosis-like symptoms, for years.
Signs and Symptoms
Valley fever symptoms are similar to those of other common infections. This can make the disease difficult to detect, and many people may go undiagnosed. Some people never have symptoms of valley fever, even if they have been exposed to the fungus. If you do get them, symptoms usually appear five days to three weeks after exposure. For people who do get ill, symptoms of valley fever often include: (1, 2)
- Fever
- Chills
- Muscle aches and pain or stiffness in the joints
- Cough
- Night sweats
- Feeling tired or fatigued
- Red, bumpy, painful rash on the upper body or the legs
- Headache
- Shortness of breath
- Swollen ankles, feet or legs
- Loss of appetite
If your infection spreads from the lungs to other parts of your body, you will need medical attention and likely a hospital stay. When the infection spreads, it is called disseminated coccidioidomycosis. Symptoms of disseminated coccidioidomycosis include: (3, 4)
- Skin problems, such as ulcers, lesions or nodules that are worse than a rash
- Skeletal problems, such as lesions on your bones, skull and spine
- Joint problems, such as achy or swollen ankles and knees
- Severe and deadly secondary infections, such as meningitis. This can cause a stiff neck, a sudden spiked fever, confusion, severe headache or a headache with nausea or vomiting, seizures, sensitivity to light, difficulty staying awake, lack of appetite and other sudden changes in how you feel
Some people also develop a chronic valley fever infection. This is most common in people with compromised immune systems, such as people with HIV/AIDS and the elderly. The symptoms of valley fever in these cases may resemble tuberculosis symptoms. They include: (3)
- Coughing up blood
- Chest pain
- Fever
- Weight loss
- Pneumonia
- Cough
- Lung nodules
Valley fever is most likely to cause symptoms in the elderly and people with weak immune systems. If you have symptoms that resemble those listed here or any other persistent illness, see a health care professional for diagnosis. In addition, if you live in an area known to have valley fever, or if you have recently visited a place known to have valley fever, ask about getting tested for coccidioidomycosis.
If you cough up blood, have chest pain, or experience any symptoms of meningitis, seek emergency care.
Causes and Risk Factors
Valley fever is caused by inhaling spores of the Coccidioides fungus. Two types of Coccidioides fungi can cause valley fever: Coccidioides posadasii and Coccidioides immitis. The fungus lives in dirt and may enter the air in dust and wind. The spores can travel in the air for hundreds of miles and often enter the wind when soil is disturbed by construction, weather and farming. When the spores are breathed in, they land in the lungs and start to reproduce. If your body doesn’t fight them off, they can reproduce enough to cause an infection with noticeable symptoms.
Risk factors for valley fever infection include: (1, 4, 5)
- Living in or visiting an area with Coccidioides in the soil
- Being near construction or farming sites in these locations
- Working in construction, agriculture, ranching, archeology, the military (outside) or other professions with a lot of exposure to the soil in a region with valley fever
- Being in a dust storm or other weather event in one of these areas
- A weak immune system
- This can include people with other infections, such as HIV/AIDS, people who have had an organ transplant or people taking medications that weaken the immune system, such as corticosteroids
- Diabetes
- Older age
- Pregnancy or recent childbirth
- Black, Filipino, Hispanic or Native American race/ethnicity
Diagnosis and Conventional Treatment
Valley fever is diagnosed with a blood test. A health care professional will take a blood sample and send it for laboratory analysis, where it will be checked for signs that your body is fighting off Coccidioides. You can also expect to give a medical and travel history, describe your symptoms and have a physical exam. Doctors may also request a tissue sample (biopsy) or a sputum sample. If you have severe respiratory symptoms, health care providers may image your lungs using a chest X-ray or CT scan.
Valley fever diagnosis is often delayed since it resembles other infections. However, if your symptoms last for a long time and you are in an area with valley fever, it is reasonable to request a test for coccidioidomycosis.
Conventional valley fever treatment includes at-home management of symptoms. Most people get better in a few months with no special medical care. In low-risk cases, most health care providers will just recommend resting. However, some people may receive treatment to prevent the infection from getting worse. (2)
- Antifungal medication may be given to people at high risk for serious infections
- This usually involves fluconazole or another antifungal drug for three to six months
- If you have a serious lung infection or valley fever that has spread beyond the lungs, you may need to stay at the hospital for monitoring and treatment
- Treatment will last longer than six months in these cases
- People with meningitis caused by valley fever may need lifelong fungal treatment, since meningitis can lead to death when not treated
- People with joint or muscle pain may be given itraconazole to help speed healing and reduce pain
Tips for Managing Valley Fever Symptoms
If you have been diagnosed with valley fever, talk to a health care professional about the best treatment approach. You should also monitor your symptoms carefully and get medical attention for any sudden changes in symptoms or if your symptoms get worse.
There are many natural ways you can help manage your symptoms. These may bring some relief during the weeks or months of symptoms associated with valley fever. Consider the tips below for managing common symptoms.
1. Soothe a rash
Valley fever rash can be red, spotted and painful or itchy. It may appear on your upper body and legs. If your health care provider agrees, consider the following natural treatments for a rash:
- Herbs, ointments and topical decoctions have long been used to treat rashes and skin irritation. A review of herbs used on the skin in South Africa for this purpose (which did not study how well they work) included: (6)
- Bulbine frutescens, also called the burn jelly plant, grass aloe or cat’s tail. The South African Herb Academy and other herbal experts also say the plant’s jelly-like juice can be applied to the skin much like that of a standard aloe plant (7)
- Cassine transvaalensis or bark of saffronwood
- Diospyros mespiliformis or African ebony
- Opuntia ficusindica or prickly pear or barbary fig
- Rauvolfia caffra or bark of the quinine tree
- Note: Always consult a health professional before using herbal remedies. If you notice increased skin irritation, stop using the treatment immediately and consult a physician
- Try Dr. Axe’s suggestions for topical natural rash remedies:
- Three drops of geranium, rose or lavender oil mixed with a half-teaspoon of coconut oil, applied to the irritated skin three times per day
- Bentonite clay, particularly if your rash is itchy
- Cocoa butter (without added alcohol, fragrance or other chemicals)
- Aloe vera gel or ointment
- Consider an oatmeal bath
- Use cool compresses on your affected skin to relieve some pain or irritation. Make sure they are clean and don’t apply ice packs directly to the skin. Instead, wrap them in a thin towel first.
2. Manage your fever
You can follow Dr. Axe’s general tips for how to get rid of a fever, which include:
- Rest! Get plenty of sleep, avoid strenuous activity and take time off of work or school if needed.
- Drink plenty of fluids, especially water and clear juices.
- Eat a mild, bland diet until you feel well enough to return to a normal diet.
- Take a lukewarm bath (not a hot or cold one).
- Resist the urge to overdress or use too many blankets.
Some natural remedies for fever may also be useful. However, research is not conclusive regarding how well certain herbs and supplements work for managing fever. Always speak with a health care professional prior to trying any herbal remedies or supplements. A few options include:
- Virgin coconut oil. Early animal research suggests that coconut oil prepared from coconut milk, without using chemicals or high heat, offers some anti-inflammatory, pain relief and fever reducing effects. (8)
- Caesalpinia bonducella F. Known as the “fever nut” in English, this plant’s whole seeds and seed extracts have been used in Ayurdevic medicine to relieve fever for quite some time. Early animal research also suggests it may have anti-inflammatory, pain relief and fever-reducing properties. (9)
- Viola betonicifolia. Also known as arrowhead violet or mountain violet, this plant’s extracts have shown anti-inflammatory, pain relief and fever-reducing effects on multiple animal models. Both the violet and its close relative, the pansy, have long been used in herbal medicine for fever relief. (10)
- Mangrove. Many different types of mangrove have been studied for their medicinal properties. So far, lab and animal research indicate that extracts of the plants often have anti-inflammatory, pain-relieving and fever-reducing qualities. (11)
- Moringa oleifera. The bark of this traditional herbal remedy were found to be very effective against fever in an animal model. More research is needed to confirm its anti-fever effects in humans, however. (12)
- Citruslatifolia Tanaka (Persian or Tahiti lime) essential oil and lemon essential oil. Some research in lab models may confirm traditional medicine’s use of citrus oils for fever and inflammation relief. (13)
- Meadowsweet. Early studies suggest Filipendula ulmaria (L.) Maxim, Rosaceae), traditionally used to treat fever and inflammatory conditions, may indeed have some of these properties. Animal studies and lab studies confirm anti-inflammatory effects of the plant’s extracts. (14)
3. Relieve aching muscles and joints
Just as with the flu, you may have sore muscles and tender, achy or swollen joints during your stint with valley fever. Get some natural relief by trying some natural ways to ease pain in the muscles or to address bone and joint pain:
- Massage therapy
- Oil or ointment with arnica oil added
- Oil or ointment with essential peppermint or lemongrass oil added
- Epsom salt bath in lukewarm water
- Dr. Axe’s homemade muscle rub
- Heating pads or cold packs. Apply them to your own comfort, generally no more than 15 minutes at a time. You can apply heat or cold several times per day
4. Address a headache
How you manage a headache may vary based on the type of pain you feel. However, many types of headaches respond to natural therapies. Speak with a health care professional before trying any herbs, supplements or other therapies for your headaches, as they may interact with other medications or health conditions.
Consider these tips for natural headache relief: (15)
- Use essential oils. Many people find headache relief by inhaling or applying diluted essential oil to the temples and forehead. Common picks include peppermint, lavender, thyme, rosemary, cinnamon and clove.
- Apply a cold pack. An ice pack on the back of your neck, forehead, temples or wherever you feel the pain in your head may relieve pain. Wrap it in a thin towel first.
- Drink tea. Chamomile, basil and ginger teas are said to give some people headache relief.
- Try herbal remedies. A review of many studies found that feverfew can often decrease headaches with regular use. (16) Dr. Axe recommends 50–100 milligrams of feverfew extract in capsule, tablet or liquid form.
- Try massage therapy or physiotherapy. These involve applying pressure and massage to the temples, neck, back or the painful part of your head. You can simply ask a family member or friend for a back and neck rub or get a professional session.
- On your own, you can apply gentle, steady pressure using your pointer finger or thumb. Press against the painful part of your head for up to 15 seconds, then stop. You can do this as needed.
- Rest. Lay still in a dark or dim room. Keep your surroundings quiet and get comfortable on a pillow. Focus on relieving the tension from your head, neck, shoulders, back and down on through the rest of your body. Breathe slowly and deeply to focus on sensations other than your headache.
5. Calm your cough
Because valley fever primarily affects your lungs, most people with symptoms have a cough. You can try these natural remedies to soothe your cough: (16)
- Honey. Add honey to your tea or use a spoonful of honey before bed to ease coughing. (Note: Do not give honey to small children or infants.)
- Ginger. Add a few slices of fresh ginger to boiling water. Once it’s a safe temperature you can drink it as a tea to help calm your cough.
- Try a natural vapor rub. Dr. Axe’s homemade vapor rub includes peppermint and eucalyptus oils to open airways and ease breathing.
- Boost your body’s immune system. You may be able to help your system speed up its own recovery and relieve your symptoms. Many natural herbs and substances have powerful antifungal effects, and a natural extract is the basis of one of the most common antifungal drugs used to treat valley fever. (17) Although many herbs have topical impacts, it is less common to see antifungal supplements in the store. Garlic is a popular option for antimicrobial and antifungal therapy, however. You can consider adding it to your diet or asking your health care provider about it as a supplement. Apple cider vinegar, oregano oil and grapefruit seed extract may be others to ask about. (18)
Prevention
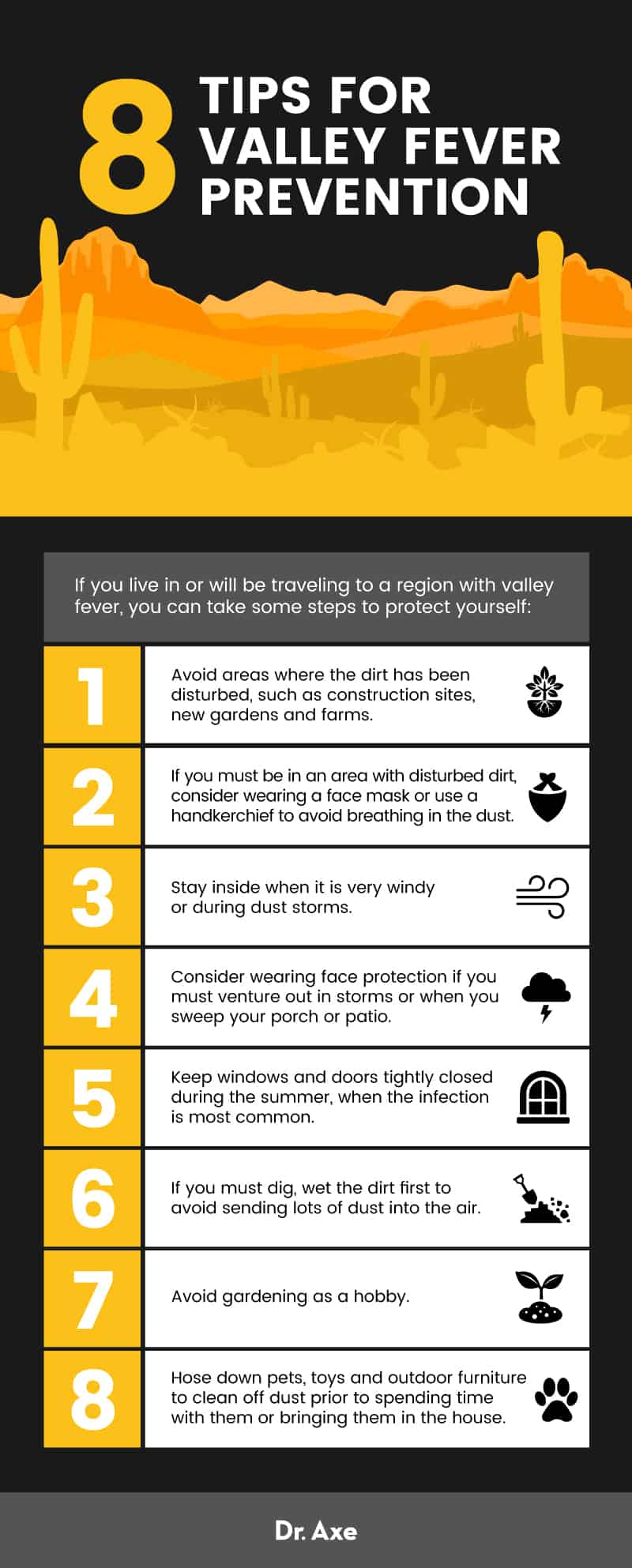
If you live in or will be traveling to a region with valley fever, you can take some steps to protect yourself:
- Avoid areas where the dirt has been disturbed, such as construction sites, new gardens and farms.
- If you must be in an area with disturbed dirt, consider wearing a face mask or use a handkerchief to avoid breathing in the dust.
- Stay inside when it is very windy or during dust storms.
- Consider wearing face protection if you must venture out in storms or when you sweep your porch or patio.
- Keep windows and doors tightly closed during the summer, when the infection is most common.
- If you must dig, wet the dirt first to avoid sending lots of dust into the air.
- Avoid gardening as a hobby.
- Hose down pets, toys and outdoor furniture to clean off dust prior to spending time with them or bringing them in the house.
Precautions
- Complications from valley fever, such as meningitis, can be deadly. If you believe you have valley fever, if you have flu-like symptoms that last longer than expected, or if your symptoms suddenly get worse, seek medical attention. A formal diagnosis can help make sure you get the care or medical advice you need for proper healing.
- In some cases, people experience long-term effects of valley fever in the form of nerve damage or chronic infection. These complications are rare and should be managed under the guidance of a health care professional.
- People with valley fever that has spread to other parts of the body — such as the heart, brain, liver, skin or bones — have a high death rate. If you feel you need treatment or that you are getting worse, seek medical attention right away.
- Do not start or stop taking any medicines, herbal remedies, supplements or other treatments without consulting a health care professional first. Some remedies may interact with medications and health conditions and result in dangerous health problems.
- Valley fever in dogs is quite common and can be costly. If you have a dog or other pet and live in or are visiting a region with valley fever, try to keep your pet from licking dirt or digging in dirt. Walk on paved surfaces instead of dirt trails.
Final Thoughts
- Valley fever, also known as coccidioidomycosis, is an infection caused by breathing in a fungus. The fungus is found in soil in certain areas of the U.S. Southwest as well as parts of Central and South America. The infection affects people and animals and is not contagious, meaning you can’t “catch” it from other people.
- Many people exposed to the fungus don’t develop symptoms. The first symptoms of valley fever for those who do, however, usually resemble the flu. Expect a fever, headache, cough, painful red rash and muscle or joint aches about five–21 days after exposure.
- People experiencing symptoms that do not get better after a week or two, or anyone with a severe worsening of their symptoms, should get medical attention. Ask for a valley fever test if you live in or have recently visited an area with valley fever.
- Most people recover with no medical treatment within a few weeks or months. Others may develop a serious infection in the lungs, an infection that spreads to other parts of the body (called disseminated coccidioidomycosis) or a chronic infection that can last for a year or more. Still others develop serious complications, such as meningitis, that can be life-threatening.
- People can often recover at home by managing symptoms and keeping themselves comfortable. Depending on your risk factors or symptoms, however, you may need an antifungal drug or hospitalization. Always discuss the best care plan for you with your health care provider. Do not attempt to diagnose or manage the condition on your own.
There are many natural ways people can help ease their valley fever symptoms. You can try natural approaches to:
- Soothe a rash
- Manage your fever
- Relieve aching muscles and joints
- Address a headache
- Calm your cough
Read Next: Bee Sting Treatment: 7 Home Remedies








