This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Ehlers-Danlos Syndrome (+ 7 Natural Ways to Manage Symptoms)
February 23, 2018

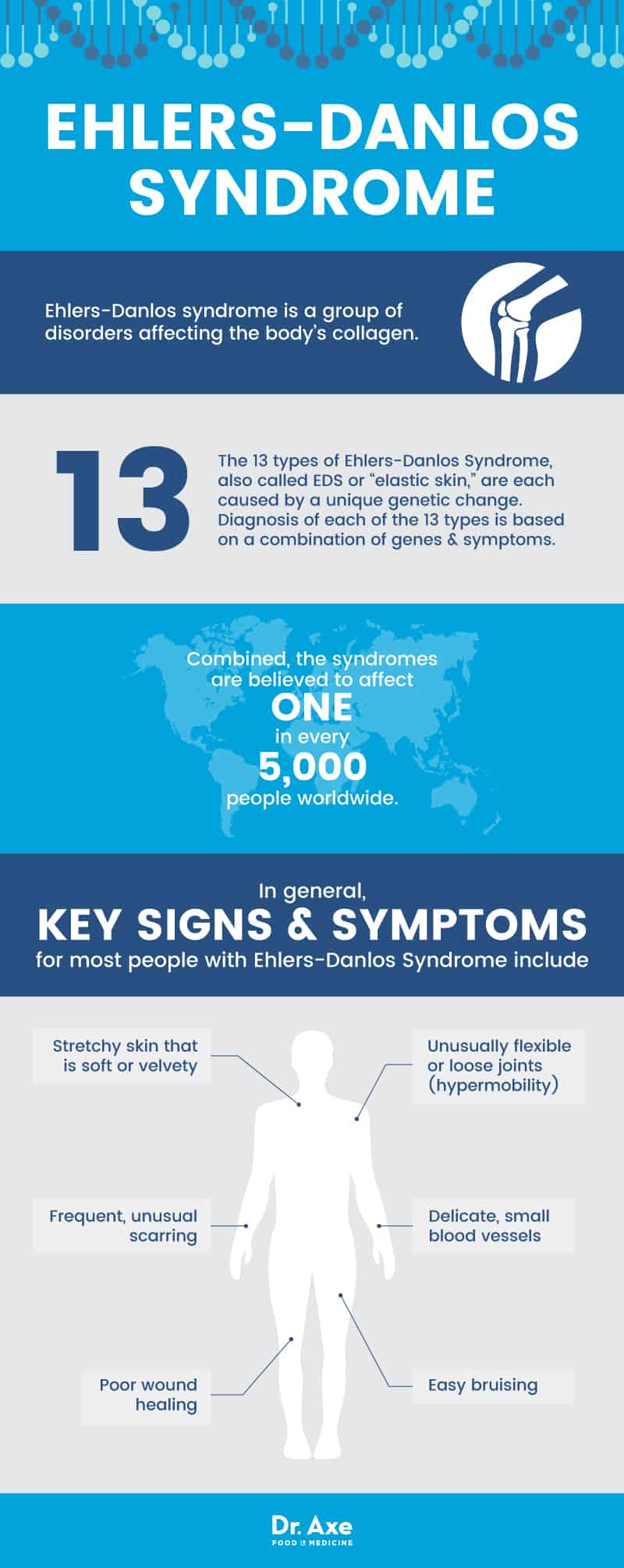
Ehlers-Danlos syndrome is a group of genetic disorders that cause loose joints and skin. The condition can also affect tissue, organs, bones and blood vessels. There are 13 types of Ehlers-Danlos syndrome, and the condition can greatly range in severity from person to person even among the same subtype. Once a formal diagnosis is known, many people can benefit from both conventional treatments and natural prevention and management strategies.
What Is Ehlers-Danlos Syndrome?
Ehlers-Danlos syndrome is a group of disorders affecting the body’s collagen. Collagen is an important building block for the body’s connective tissue, including the bones. It also helps support cartilage and skin to give the body strength and flexibility.
The 13 types of Ehlers-Danlos Syndrome, also called EDS or “elastic skin,” are each caused by a unique genetic change. EDS was originally split into 11 categories and was then simplified into six categories, based on symptoms, in 1997. Once new genetic differences were revealed, the syndromes were reclassified in 2017 into the current 13 types. Diagnosis of each of the 13 types is based on a combination of genes and symptoms.
Combined, the syndromes are believed to affect one in every 5,000 people worldwide. However, prevalence of Ehlers-Danlos syndromes varies from subtype to subtype. For example, some of the rarer forms have only been found in a few people or families—ever!—while others, such as hypermobile EDS, affect one in every 5,000 to 20,000 people. (1)
EDS is not curable, but it is treatable. In addition, many people can take preventive steps to keep their health as good as possible. The Ehlers-Danlos Society recommends that anyone who suspects they may have EDS or hypermobility see a genetic specialist for a formal diagnosis. This is because geneticists may be better at identifying the exact type of EDS you have, or may be able to tell if your symptoms are caused by a different connective tissue disorder instead. (2)
Is there a blood test for Ehlers-Danlos Syndrome?
In most cases, Ehlers-Danlos Syndrome can be diagnosed via a combination of a physical examination, medical history of you and your family, and a blood test to check for EDS genes. Even if no known EDS genes are found in a genetic blood test, you can still be diagnosed with it based on your clinical signs and symptoms. In fact, one of the most common types of EDS, called hypermobile Ehlers-Danlos Syndrome or hEDS, has a genetic cause but no specific identified gene yet. This type is diagnosed using family history, signs and symptoms alone. (3)
Is Ehlers-Danlos Syndrome considered a disability?
EDS is not specifically listed as a covered disability by the U.S. Social Security Administration. However, there are general categories for physical and sensory limitations that may allow some people with EDS to qualify for disability payments. For example, if your symptoms include severe chronic joint pain, limits on your mobility, or constant risk to your heart and major blood vessels, you may qualify for benefits. According to multiple websites devoted to helping people understand disability benefits, the primary factor in whether people with EDS get approval appears to be how limited they are in terms of ability to perform work because of their EDS symptoms, not the diagnosis of EDS alone. (4, 5, 6)
Is Ehlers-Danlos Syndrome life threatening?
In most cases, people with EDS have average life expectancy. This can be reached most easily when people take care to avoid injury and protect their health.
However, certain subtypes of EDS can be very severe and life-threatening. For example, vascular EDS can result in sudden death due to problems with the aorta. Kyphoscoliotic EDS can eventually cause curvature of the spine over time that makes it difficult to breathe. In addition, other types of EDS can be life-threatening if people have very fragile blood vessels or complications such as ruptured organs or serious injuries. (7, 8)
Signs & Symptoms
In general, key signs and symptoms for most people with Ehlers-Danlos Syndrome include: (9)
- Unusually flexible or loose joints (hypermobility)
- Delicate, small blood vessels
- Easy bruising
- Stretchy skin that is soft or velvety
- Frequent, unusual scarring
- Poor wound healing
According to the National Organization for Rare Disorders (NORD), symptoms specific to the 13 types of Ehlers-Danlos Syndrome include: (10)
- Arthrochalasia
- Mobility limitations due to major risk of dislocating multiple joints at the same time
- Low muscle tone and dislocation of the hips at birth
- Brittle cornea
- Eye problems such as increased risk of a ruptured cornea after a minor injury, degeneration of the cornea, and having a cornea stick out (protrusion)
- Bluish tinge to the white parts of the eye
- Cardiac-valvular
- Minor common symptoms of EDS, but severe heart defects that require surgery
- Classical
- Stretchy skin and loose joints, fragile blood vessels and thin, paper-like, discolored scars
- People with classical EDS may also have small lumps under the skin and problems with their heart valves. These problems may lead to heart failure and poor circulation over time. It may also cause an emergency heart condition called aortic dissection, which can be life threatening.
- Classical-like
- The same signs and symptoms as classical EDS, but with a different genetic cause
- Dermatosparaxis
- Physical features such as short height, short fingers, loose facial skin but full eyelids, bluish whites of the eye and a small jaw
- Hernias (when an organ pushes through the tissue that is supposed to hold it in place) and slow wound healing
- Increased risk of bladder or diaphragm rupture
- Hypermobility (hEDS)
- Frequent dislocation of joints, chronic pain, degenerative joint disease, lightheadedness when changing position, bowel disorders, and emotional problems
- Kyphoscoliotic
- Eye problems such as near-sightedness, glaucoma, detached retina, vision loss, and increased risk of a ruptured eyeball
- Spine problems such as scoliosis that gets worse over time and may eventually impact breathing
- Musculocontractural
- Developmental delay, low muscle tone and strength, face or skull structure defects, limited movement of fingers, scoliosis, club foot and eye problems
- Myopathic
- Low muscle tone from birth, plus muscles that do not work correctly
- Scoliosis and hearing loss
- Periodontal
- Gum disease and problems with the teeth and gums that lead to early tooth loss
- Spondylodysplastic
- Skeletal problems such as stunted growth, short height, eyes that stick out and have a bluish tinge, wrinkled palms, weak thumb muscles and tapered fingers
- Vascular
- Detected at birth due to physical deformities such as club foot and hip dislocation
- Facial features such as sunken cheeks, thin nose and lips, prominent eyes
- Increased risk of headaches, seizures, stroke and aneurisms, and post-surgery complications in wound healing
- “Old-looking” hands and varicose veins at a young age
- Increased risk of rupture or bleeding of major organs and blood vessels, such as the uterus, intestines and aorta
Causes & Risk Factors
Ehlers-Danlos syndromes are genetic disorders. This means that they are caused by mutated genes. In many subtypes of EDS, the genes are known and can be found in a blood test. In other types of EDS, however, the genetic cause is not yet known. Regardless, in most cases these gene mutations change the way collagen is made or used in the body.
Some of the genes with mutations that can cause Ehlers-Danlos Syndrome include: (11)
- ADAMTS2
- COL1A1
- COL1A2
- COL3A1
- COL5A1
- COL5A2
- FKBP14
- PLOD1
- TNXB
According to the Genetic and Rare Diseases Information Center, part of the National Institutes of Health (NIH), your risk of having EDS depends on the subtype that runs in the family. Some subtypes have a dominant inheritance pattern, meaning you only need to get the mutated gene from one parent in order to have the syndrome (each child has a 50-50 chance). Other subtypes are recessive, meaning they have to inherit a mutated gene from both parents. In recessive subtypes, each child of two parents with the gene has a one in four chance of having the syndrome. (11)
Other than having a family history of EDS, there are no known risk factors. The disease affects every race and ethnicity and impacts men and women equally. (12)
Conventional Treatment
There is no cure for Ehlers-Danlos Syndrome. Treatments can help symptoms and differ from person to person. Common treatments for people with EDS may include: (13)
- Over-the-counter pain medication as needed
- Prescription pain medication for acute, temporary pain or injuries
- Blood pressure drugs to keep pressure low, for people with fragile blood vessels
- Surgery and stitches to repair damaged joints, ruptured blood vessels or organs
Prevention
There are two ways to approach prevention in Ehlers-Danlos Syndrome: trying to avoid passing it on to your children and trying to prevent symptoms of EDS once it is diagnosed. You can speak with a genetic counselor if you are thinking about having children to learn more about your risk of passing the disorder to your children. (7)
Prevention of symptoms and disease progression are discussed in the next section.
7 Natural Ways to Manage Ehlers-Danlos Syndrome Symptoms
People with Ehlers-Danlos Syndrome can often reduce their risk of serious complications by following some preventive lifestyle tips. Please note that you should speak with your doctor prior to changing your treatment plan, as not all natural management strategies are appropriate for people with all types of EDS. Tips for naturally managing EDS and preventing some symptoms include: (10, 13)
- Avoid physical stress
- Consider dietary supplements
- Get low-impact exercise and physical therapy
- Use assistive devices
- Avoid injury and invasive procedures
- Baby your skin
- Get help coping
-
Avoid physical stress
Strenuous physical activity can lead to injury, dislocated joints, increased blood pressure and bruising. It can also cause or worsen joint pain. You can help limit the physical stress on your body by:
- Asking for less-demanding tasks at work
- Avoiding repetitive motions
- Requesting help with strenuous housework
- Avoiding contact or high-impact sports, such as football, hockey, gymnastics and sprinting
- Avoiding lifting weights or heavy items
- Taking it easy on your jaw by not chewing gum, ice, or hard candy
- Not playing wind or brass instruments
-
Consider dietary supplements
Before you consider dietary supplements, speak with your doctor to find out if they may interfere with any medications you may be taking.
- Many symptoms of Ehlers-Danlos Syndrome resemble those of nutrient deficiencies. Because of this fact and increasing evidence that symptoms of genetic conditions can sometimes be influenced by nutrition, researchers are investigating some of the following supplements for their use in EDS symptom management: (14)
- Calcium
- Carnitine
- Coenzyme Q10
- Glucosamine
- Magnesium
- Methyl sulphonyl methane
- Pycnogenol
- Silica
- Vitamin C
- Vitamin K
- In particular, vitamin C may be recommended to help speed wound healing and reduce bruising. In some cases, it may be prescribed at high doses to help reduce bleeding time, improve healing and even increase muscle strength in certain subtypes, such as kyphoscoliosis-type EDS. (15)
- Provided they do not interfere with any medications you may be taking, you may also wish to consider diet, herbs, supplements and topical therapies to:
- Lower blood pressure
- Relieve pain
- Ease bone and joint pain
- Speed bruise healing
- Speed wound healing
- Relieve arthritis symptoms
- Improve bone density
-
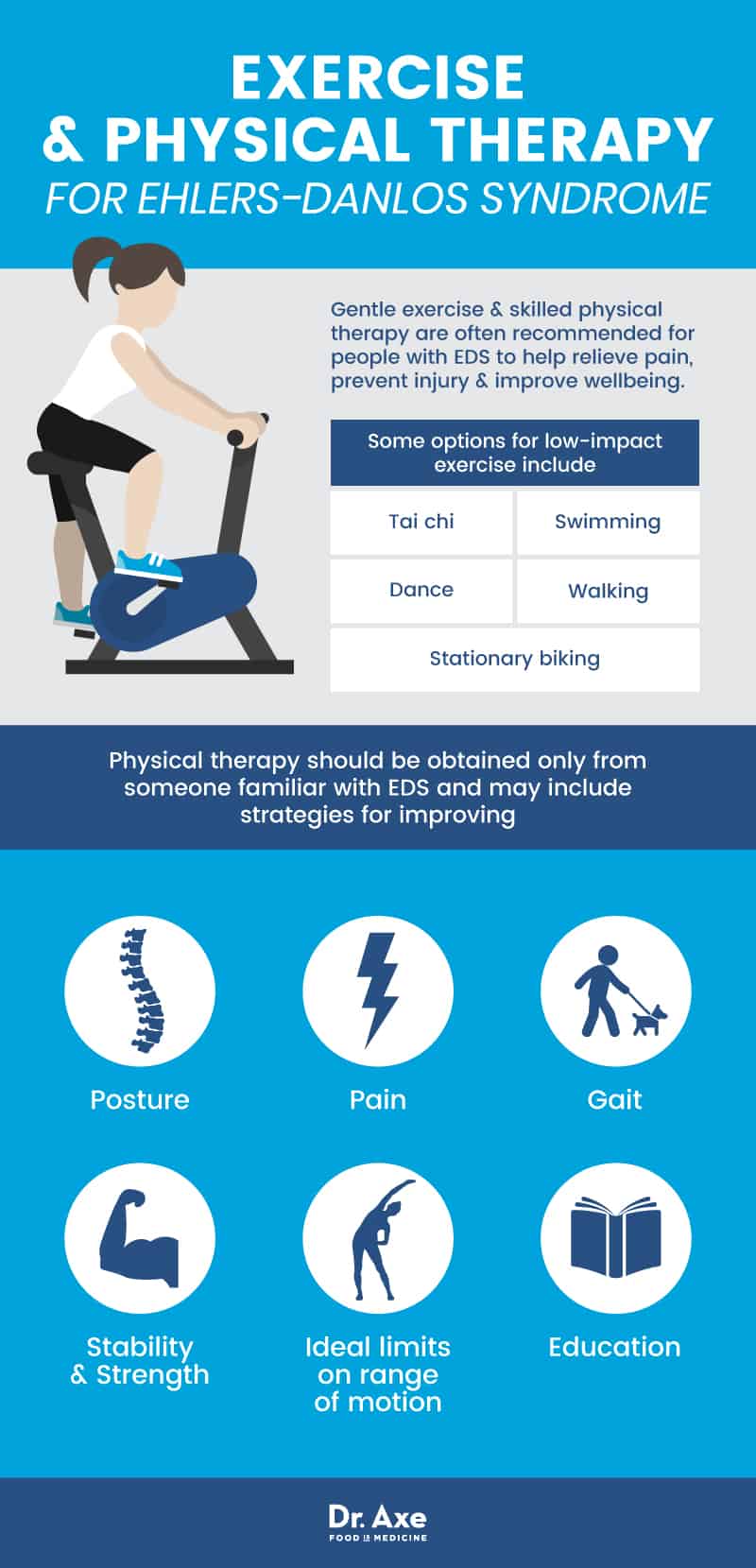
Get low-impact exercise and physical therapy
Low-impact exercise and physical therapy are often recommended for people with Ehlers-Danlos Syndrome. However, there is little research showing any particular benefit in terms of symptoms. This may be due to the fact that many people withdraw from sports and physical activities due to fear, injury or discomfort, plus many physical therapists are not familiar with EDS and its management. (16)
Some studies have found that people’s symptoms tend to improve when they do exercise and receive therapy, but that the difference is not usually significant compared to people who did not take part. (17)
Despite the lack of research, gentle exercise and skilled physical therapy are often recommended for people with EDS to help relieve pain, prevent injury and improve wellbeing.
- Some options for low-impact exercise include:
- Physical therapy should be obtained only from someone familiar with EDS and may include strategies for improving: (18)
- Posture
- Pain
- Gait
- Stability
- Strength
- Ideal limits on range of motion
- Education
-
Use assistive devices
Depending on your symptoms and the types of problems you are at risk for based on your EDS diagnosis, you may need or want to use assistive devices. Some tools, as well as occupational therapy, may be very useful in helping minimize strain, pain and fatigue. Ideas for helpful devices and tools for people with EDS include: (16, 19)
- Canes, scooters or wheelchairs
- Splints or braces to limit risks to joints
- Step stools to reduce reaching overhead
- Heat and ice packs
- Low-pressure mattress
- Jar and can opener tools
- Utensils with large, soft grips
- Carts and trolleys
- Roller backpacks, briefcases or suitcases
- Long-handled cleaning tools
- Ergonomic desk tools, such as wrist supports and foot rests
- Cushions
- Compression garments
- Medic-alert bracelets
-
Avoid injury and invasive procedures
For people with most forms of EDS, injury, invasive procedures such as surgery, and traumatic physical experiences such as childbirth can be dangerous. Consider these tips to avoid some of the possible complications that come with stress on your joints, tissue, bones and blood vessels: (10, 15, 19)
- Visit an obstetrician who is specially trained in high-risk pregnancies if you are going to have a baby
- Use knee and elbow pads and a helmet during sports
- As children with EDS learn to walk, teach them on soft, padded surfaces
- Work with a physician to recommend non-invasive disease screening whenever possible, and to carefully weigh the risks and benefits of invasive screenings (such as colonoscopies)
- Prevent disease progression by getting regular vision, blood pressure, bone density, heart disease, and other screenings based on your particular risks
- Avoid elective surgeries
- Ask about less-invasive options (such as robotic or laparoscopic) for medically necessary but non-emergency surgeries
- Use skin glue and adhesive strips instead of stitches when possible
-
Baby your skin
EDS carries many risks for the health and strength of your skin. You can help prevent skin breakage, protect it from damage and potentially speed wound healing by doing the following: (20, 21)
- Use sunscreen daily
- Wear protective bandages on exposed skin (for people with frequent skin problems)
- Avoid soap, body wash and body lotions with harsh chemicals that may dry out the skin or cause allergic reactions
- Massage your skin with coconut oil to retain moisture and fight bacteria
- Reduce the appearance or promote the healing of scars using coconut oil, shea butter, and other natural topical treatments if your doctor says they are safe for you
-
Get help coping
Many people with EDS have more than just physical symptoms. The syndromes can be very challenging emotionally and socially, and are associated with depression, anxiety, fear, trouble sleeping, guilt, social avoidance, stigma, eating disorders, alcohol and tobacco misuse, neurodevelopmental disorders and other difficult experiences. (16, 18)
You may wish to try some of the following to improve your emotional, social and mental health support:
- Try cognitive behavioral therapy. A study combining cognitive behavioral therapy with physical therapy in 12 women with EDS found significant improvements in muscle strength, endurance, perceived ability to perform daily activities, fear of exercise, perceived pain and participation in daily life. (22)
- Build a support system. Reach out to family, friends, religious advisors, teachers or employers and others who can offer assistance, accommodations and encouragement. (13)
- Get high-quality rest. Fight fatigue and the mood problems that come with it by getting enough sleep. Many people with EDS have disordered breathing during sleep, as well as significant daytime fatigue. (23, 24) Tips to improve sleep include getting into a routine, not smoking or drinking alcohol, avoiding screen time for an hour before bed, and keeping the room dark and cool.
- Talk with others who understand EDS. Check out groups such as the Ehlers-Danlos Society and local or online social groups to find people who understand your experiences. (25)
Precautions
- EDS can be a serious medical condition. It can also resemble many other connective tissue disorders. To make sure you have a proper diagnosis for your symptoms, you should visit a physician or geneticist.
- Do not attempt to treat EDS at home unless you have a formal diagnosis and care plan from a physician.
- Some types of EDS cause problems with the aorta and other major blood vessels that can cause sudden death if you do not receive immediate emergency care and surgery. If you ever feel searing, burning pain in your abdomen or chest, seek care immediately. Wear a medical alert bracelet that names your specific EDS diagnosis so that first responders better understand how to assess and treat you.
- Do not start or stop taking medications or supplements without first discussing the plan with your doctor. This is because many natural herbs and supplements can interact with prescription medications and cause unintended side effects.
Ehlers-Danlos Syndrome Key Points
- Ehlers-Danlos Syndrome is a group of genetic disorders that affects the body’s connective tissue. Its key characteristics are stretchy skin and flexible joints.
- Many people with EDS experience other symptoms, such as chronic pain, fatigue, easy bruising, poor wound healing and abnormal scarring.
- There are 13 subtypes of EDS, ranging from mild to life threatening. In most cases, life expectancy is normal or close to normal provided people are careful to avoid injury. However, certain subtypes of the disease can result in sudden death due to a ruptured aorta.
- There is no cure for EDS. Instead, the symptoms are treated as needed using anything from over-the-counter pain medications and physical therapy to surgery.
7 Natural Management Strategies
People with Ehlers-Danlos syndromes can often manage their symptoms by taking preventive measures. They may also benefit from these natural management strategies:
- Avoid physical stress
- Consider dietary supplements
- Get low-impact exercise and physical therapy
- Use assistive devices
- Avoid injury and invasive procedures
- Baby your skin
- Get help coping








