This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Spinal Stenosis Symptoms, Causes & Treatments
June 27, 2016
Chronic back pain is a major problem for millions of adults. It’s now estimated that around 75 percent of all people will experience a period of persistent back pain at some time in their lives, and 1 percent to 2 percent will suffer from serious compression of a nerve root — and another 3 percent to 5 percent have herniated discs. (1) Contributing to this back pain is spinal stenosis.
The spine is a row of 26 small bones in your back that allow you to stand up straight, walk, lift and bend over. Spinal stenosis is often attributed to “wear and tear” caused by aging — considered to be part of the degenerative cascade that causes bone weakening and cartilage loss. However, there are also specific risk factors that make certain people more likely to develop stenosis, including having high levels of inflammation, tumors or injuries that affect the spine, and a history of other inflammatory medical conditions.
While older people are most likely to suffer from spinal stenosis, middle-aged adults can develop this condition too. And a small percentage of younger people are also born with inherited, narrowed spinal canals that limit their mobility. The good news is there are ways you can help manage spinal stenosis. So what exactly is this condition, along with the causes and symptoms, along with how to treat it? Let’s find out.
What Is Spinal Stenosis?
Spinal stenosis is a disorder that’s caused by narrowing of the spinal canal, which is the passage of nerves that runs down the center of the back. Because stenosis is triggered from accumulating increased pressure that’s placed on the spinal cord and the nerves within the back, it commonly causes back pain, sciatica and other nerve problems.
Most people develop symptoms of spinal stenosis that manifest in their lower backs (lumbar region) and their necks, but others experience no noticeable symptoms at all. It’s also possible to suffer from problems related to bladder or bowel control due to spinal stenosis, caused by nerve damage that’s connected to the lower body.
While conventional treatments for stenosis include taking medications to lower inflammation or pain — and sometimes in severe cases spinal surgery — natural treatments including exercise, stretching, physical therapy and warming/icing the painful area can also be highly effective.
What Causes Spinal Stenosis?
The word “stenosis” means the abnormal narrowing of a body channel. With spinal stenosis, the narrowing happens in the bone channel occupied by the spinal nerves. Older people (usually 50 and older) with weakened joints/ligaments in the back, cartilage loss and degeneration develop stenosis most often. (2) Some research shows that the prevalence of “degenerative” lumbar stenosis in older adults can be up to 13 percent of the population. (3)
Some common disorders that can contribute to stenosis or occur at the same time include osteoarthritis/degenerative joint disease, rheumatoid arthritis, sciatic nerve pain, spinal injuries or tumors, and genetic diseases that affect the bones of the back (such as Paget’s disease). (4)
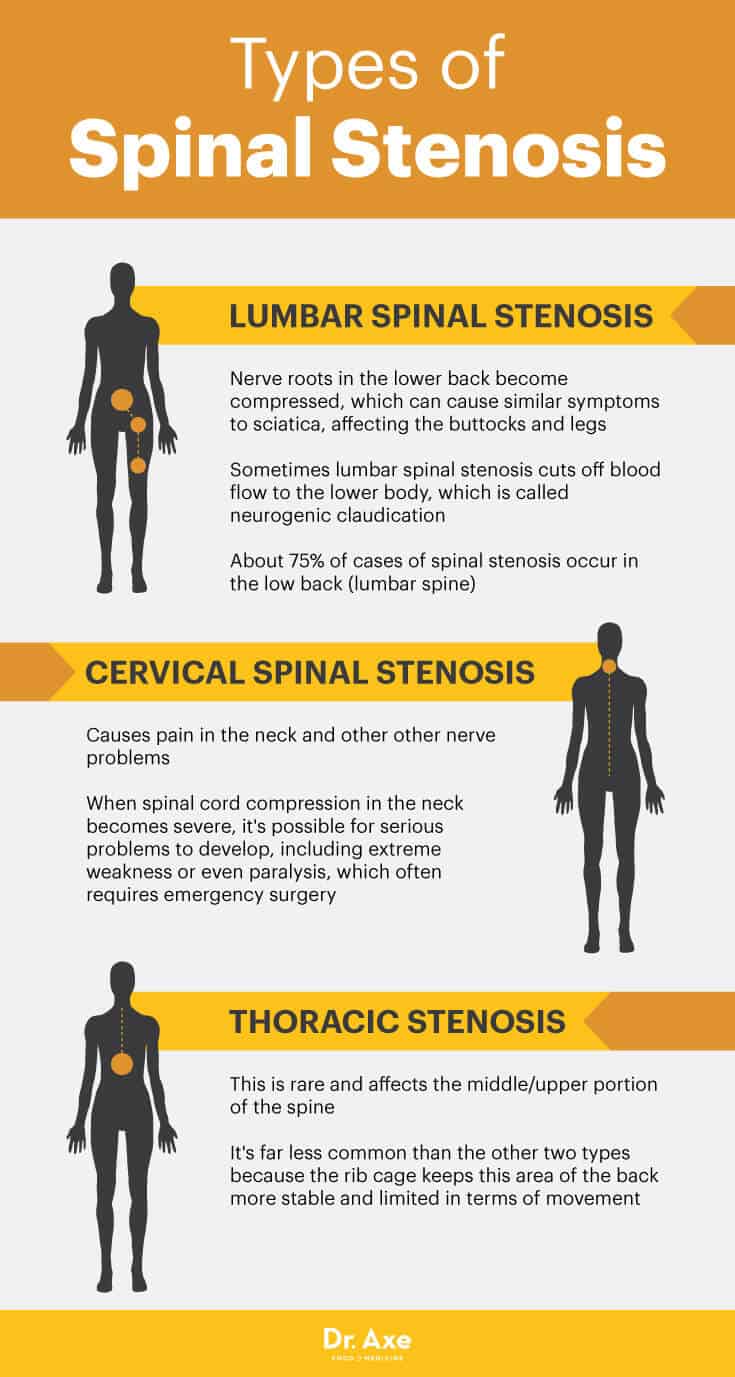
Stenosis can affect different parts of the spine. When the lower back develops stenosis, it’s called lumbar stenosis, while stenosis in the neck is called cervical stenosis. (5)
- Lumbar Spinal Stenosis: Nerve roots in the lower back become compressed, which can cause similar symptoms to sciatica, affecting the buttocks and legs. Sometimes lumbar spinal stenosis cuts off blood flow to the lower body, which is called neurogenic claudication. About 75 percent of cases of spinal stenosis occur in the low back (lumbar spine).
- Cervical Spinal Stenosis: Causes pain in the neck and other other nerve problems. When spinal cord compression in the neck becomes severe, it’s possible for serious problems to develop, including extreme weakness or even paralysis, which often requires emergency surgery.
- Thoracic Stenosis: This is rare and affects the middle/upper portion of the spine. It’s far less common than the other two types because the rib cage keeps this area of the back more stable and limited in terms of movement.
Symptoms of Spinal Stenosis
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the most common symptoms of spinal stenosis include: (6)
- back pain, especially in the lower back
- neck pain, such as a stiff neck
- tingling “pins and needles” sensations, numbness, and throbbing in the lower body; it’s possible for symptoms to spread throughout the lower body when a nerve root becomes affected
- muscle weakness or pain around the top of the legs, knees and hips (along the sciatic nerve)
- impaired bladder or bowel control
- pain when exercising or lifting heavy objects, usually immediately
- loss of balance and easily falling
- pain when standing for long periods of time, coughing, sneezing, bending, stretching or just after getting up in the morning
- in severe cases, extreme weakness and paralysis
Some people go years without knowing that they’re experiencing early signs of spinal stenosis. While a small percentage don’t have any pain or symptoms of nerve degeneration, the majority notice symptoms come on gradually. Symptoms commonly start out as minor radiating pain in the lower back or neck, throbbing, muscle weakness, and sometimes numbness. These are all signs of worsening compression of the nerves on the spinal cord. Pain can be dull at times or sharp and intense at others. As inflammation and degeneration worsen, nerve roots can become affected, which can cause the most severe, radiating pain.
Conventional Treatment for Spinal Stenosis
Pain in the middle or lower back is not always caused by stenosis. Other disorders that can cause similar pain, throbbing and numbness include herniated/bulging disc, sciatica, infections, fibromyalgia, osteoporosis and arthritis. To rule out other problems that might be responsible for a patient’s pain, doctors usually perform a physical examination, sometimes take X-rays or perform an MRI, and also discuss symptoms with the patient. It’s common for doctors to discuss the following with a patient: the patient’s symptoms, times of day when pain is worse, activities that make the pain feel better or more intense, when and how symptoms started, and whether other symptoms are also present.
Back pain is often caused by strains, pulls or minor injuries that usually heal within four to six weeks. However, if a doctor makes a diagnosis of spinal stenosis, leaving the spine alone to heal is usually not enough to solve the issue. The conventional way to treat spinal stenosis often includes:
- Over-the-counter or prescription anti-inflammatory drugs (NSAIDs)
- Other forms of painkillers, such as acetaminophen (considered to be slightly better than NSAIDs for long-term use)
- Muscle-relaxing drugs and/or drugs used to lower muscle spasms (these are often not recommended for older adults because they can cause side effects and interact with other medications)
- Short-term course of narcotic medications is sometimes used for severe episodes of nerve-related pain
- In severe cases, spinal surgery is used as a last-resort option
Natural Treatments for Spinal Stenosis
1. Exercise Regularly
Experts believe that one of the best ways to prevent back pain and spinal compression is to exercise and stretch regularly, ideally in ways that use the whole body, including the back. It might seem counterintuitive, but staying sedentary (such as avoiding exercising, stretching or even bed rest) doesn’t usually relieve back problems, so sustaining light activity is recommended if at all possible. According to the Spine Health website, the key to exercising with stenosis is to “start slowly, and build strength and tolerance over time.” (7)
A combination of aerobic activities and bodyweight exercises (or other gentle forms of resistance/strength training) helps lower overall inflammation, improves strength of muscles and keeps the joints limber. Regular exercise is also important for maintaining bone density and a healthy bodyweight, which takes pressure off the spine by decreasing risks for obesity and osteoporosis.
When you regularly perform full-body workouts — including specific exercises that train the core along muscles in the buttocks, thighs, upper back and lower back — you’re able to take some of the pressure and compression off of the spine. This helps stabilize the spine and decrease strains or pressure placed on the spinal discs, plus protect the joints and ligaments that hold the spine together. Exercise is most effective when it’s consistent and practiced before there’s even a problem, which means it’s important for young and middle-aged adults to take care of themselves.
- As a general rule if you feel strong pain while exercising, back off and get your doctor’s advice before continuing.
- Try to exercise so your muscles feel warm and slightly fatigued but not throbbing or very painful.
- Exercises that can help keep the back strong and prevent problems include swimming, brisk walking, cycling, water aerobics, resistance training using the core and back, and HIIT workouts for those who can complete more vigorous workouts. Some people find that movement is easier when slightly supported or bent over, such as holding the wheels of a bicycle or using handbars on an elliptical machine.
- Exercises that can help strengthen the back and core include squats, abdominal moves that bring the knees to the chest, pelvic tilts and full-body moves like burpees.
2. Stretch to Maintain Flexibility
Stretching the spine is a natural way to relax stiff muscles, beneficial for staying limber and helpful in preventing injuries or stiffness. It’s important to stretch after workouts and also to ease in to exercise with a warm-up period. Focus on breathing deeply while stretching, which can serve as a great way to relieve stress.
Stretches to help prevent and reduce back or sciatic pain include: (8)
- sitting leg stretches
- knee to chest stretches on the floor
- back stretches done while laying on the stomach and lifting the chest or legs
- quadricep stretches, which can be done by standing, bending one knee and pulling the foot behind you
- hip and hip flexor stretches done with your back on the floor by bending the legs, crossing one ankle over the other knee and possibly pulling on the back of the thighs to deepen the stretch
3. Maintain Good Posture and Consider Chiropractic Care
Proper posture when standing, sitting or exercising helps protect the spine and reduces stress on the back in general. Slouching can cause strains around the spine, so try to find a chair that can be adjusted so your back is straight, heels are on the floor, knees are just slightly bent and chin is parallel to the floor. If you spend a lot of time in a chair and notice that your lower back is not supported, you can place a pillow behind your back for extra support.
An effective way to address poor posture and back pain is to visit a chiropractor. Chiropractors are trained in manipulating the spine, helping improve posture and reducing nerve pain or damage. A chiropractor can perform targeted chiropractic adjustments to help realign the spinal discs, prevent further compression or protrusion into the spinal canal, and lower pain of the back, neck and sciatic nerve.
4. Try Physical Therapy
As long as movement and activity are cleared by a doctor, visiting a physical therapist (PT) can help improve healing and speed up recovery. A PT can help you safely start to practice specific posture-improving exercises that strengthen your upper legs, core and back. Sometimes special machinery or equipment is used to perform abdominal exercises that help take pressure off the spine.
PTs can also teach patients how to improve their posture and recommend tips for using more supportive shoes, chairs, mattresses, pads, pillows, etc. After some time, it’s usually possible for patients to safely transition to exercising on their own.
5. Dull Pain Naturally
- Application of heat or ice can help naturally dull pain and control inflammation. Icing the swollen area during the first 72 hours of pain following a triggering episode can help curb swelling. Try using ice packs twice daily for about 15 minutes at a time.
- As long as the painful area is not inflamed or red, you can try using a heating pad on low or medium for 15 to 20 minutes several times per day, laying down with the pad placed on your back or wrapping it around your lower back while you sit down.
- Taking a hot shower or bath is another convenient, effective way to dull pain. Add Epsom salt to a hot bath, along with soothing essential oils, such as peppermint or lavender oil, to further penetrate and relax the inflamed area.
- Massaging painful areas helps relax muscles, loosen up tight tissue, increase blood flow and even increase the production of endorphins, which ease pain. However, before beginning massage therapy treatments, it’s a good idea to get clearance from your doctor if you’re unsure about the severity of your condition.
6. Eat an Anti-Inflammatory Diet
Losing excess weight can reduce load-bearing stress on the lumbar spine and reduce or prevent stenosis. (9) A healthy diet also helps maintain muscle mass and protects you from experiencing very high levels of inflammation or complications that can make stenosis worse. High levels of inflammation weaken your bones, muscles and joints, which makes it more likely that you’ll deal with spinal problems as you age.
- Lower your intake of things like sugar, processed meats, chemically sprayed crops, refined grain products, alcohol and packaged snacks.
- Consume plenty of anti-inflammatory foods like leafy green veggies, healthy fats including extra virgin olive oil and coconut oil, “clean and lean proteins” (cage-free eggs, grass-fed meat, wild-caught fish), and fermented foods that contain probiotics.
- Suppelments to help reduce pain include turmeric, omega-3 fish oils, glucosamine, MSM and proteolytic enzymes.
- Other important factors for reducing inflammation include avoiding smoking/recreational drugs, lowering stress and sleeping well.
Spinal Stenosis vs. Arthritis in the Back
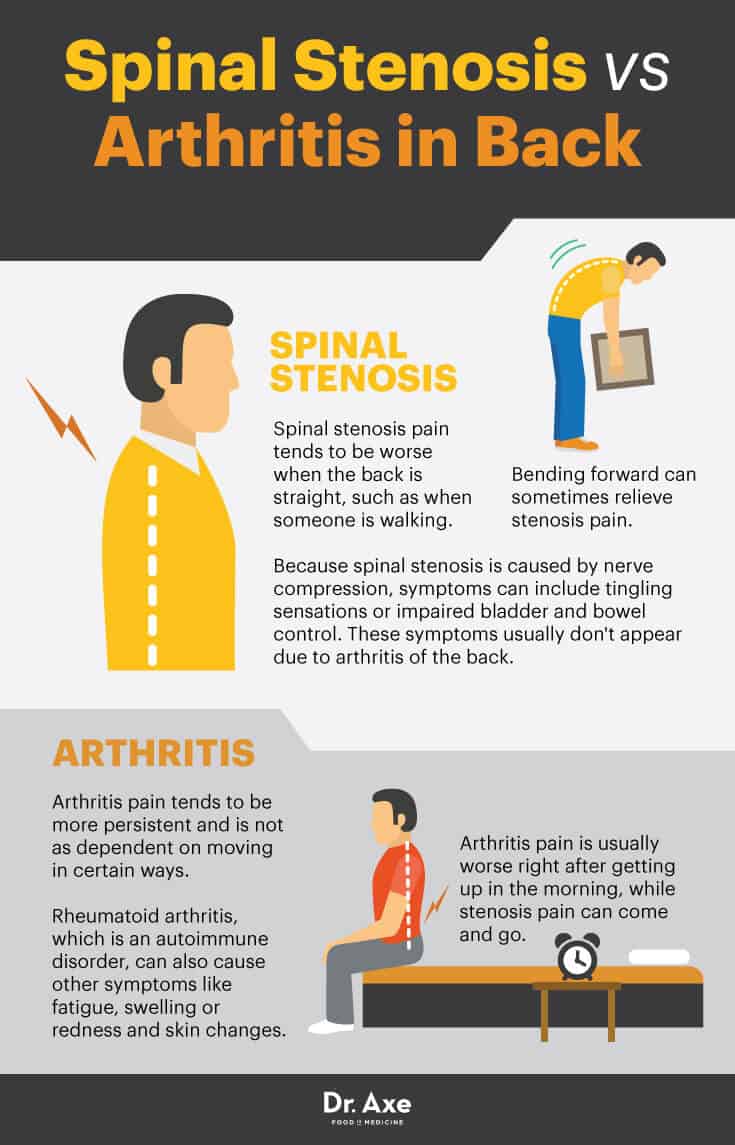
- How can you tell the difference between arthritic back pain and stenosis back pain? According to the Arthritis Foundation, spinal stenosis pain tends to be worse when the back is straight, such as when someone is walking. Bending forward can sometimes relieve stenosis pain. (10)
- Arthritis pain is usually worse right after getting up in the morning, while stenosis pain can come and go.
- Arthritis pain tends to be more persistent and is not as dependent on moving in certain ways. Rheumatoid arthritis, which is an autoimmune disorder, can also cause other symptoms like fatigue, swelling, or redness and skin changes.
- Because spinal stenosis is caused by nerve compression, symptoms can include tingling sensations or impaired bladder and bowel control. These symptoms usually don’t appear due to arthritis of the back.
Precautions About Treating Spinal Stenosis
If you experience severe pain for several days in a row, high levels of tingling or numbness, or cannot stand up and walk, always visit your doctor right away. Sometimes the recommendations above won’t be enough to reduce stenosis, and other treatments are needed.
Although surgery should be considered only in very severe circumstances, it might be necessary if your symptoms get in the way of everyday activities, stop you from walking, cause persistent problems with bowel or bladder function, and start to spread to the rest of your nervous system. (11) Visiting a rheumatologist (a doctor who treats arthritis and related disorders) and neurologist (a doctor who treat diseases of the nervous system) can help you consider your options if your case becomes very serious.
Final Thoughts on Spinal Stenosis
- Spinal stenosis causes the spinal canal to become compressed and narrowed in one or more parts of the back/neck, often causing pain and other impairments.
- Risk factors for spinal stenosis include older age, a history of medical conditions that affect the nerves/spine, sedentary lifestyle, spinal injury and family history.
- Natural treatments for spinal stenosis include exercise, stretching, physical therapy, and controlling inflammation through a healthy diet and lifestyle.








