This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Are You at Risk for Antibiotic Resistance?
June 27, 2017
Using hand sanitizers like they’re going out of style (unfortunately, they’re not) and popping antibiotics at the very first sign of an illness. Yes, without knowing it, many people practice antibacterial overkill.
Although the dangers of antibiotics are becoming more known today, many people remain confused or misinformed about when and when not to take prescription antibiotics.
According to the World Health Organization (WHO): (1)
Antimicrobial resistance threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi. It is an increasingly serious threat to global public health that requires action across all government sectors and society. Antimicrobial resistance is present in all parts of the world. New resistance mechanisms are emerging and spreading globally.
What Causes Antibiotic Resistance?
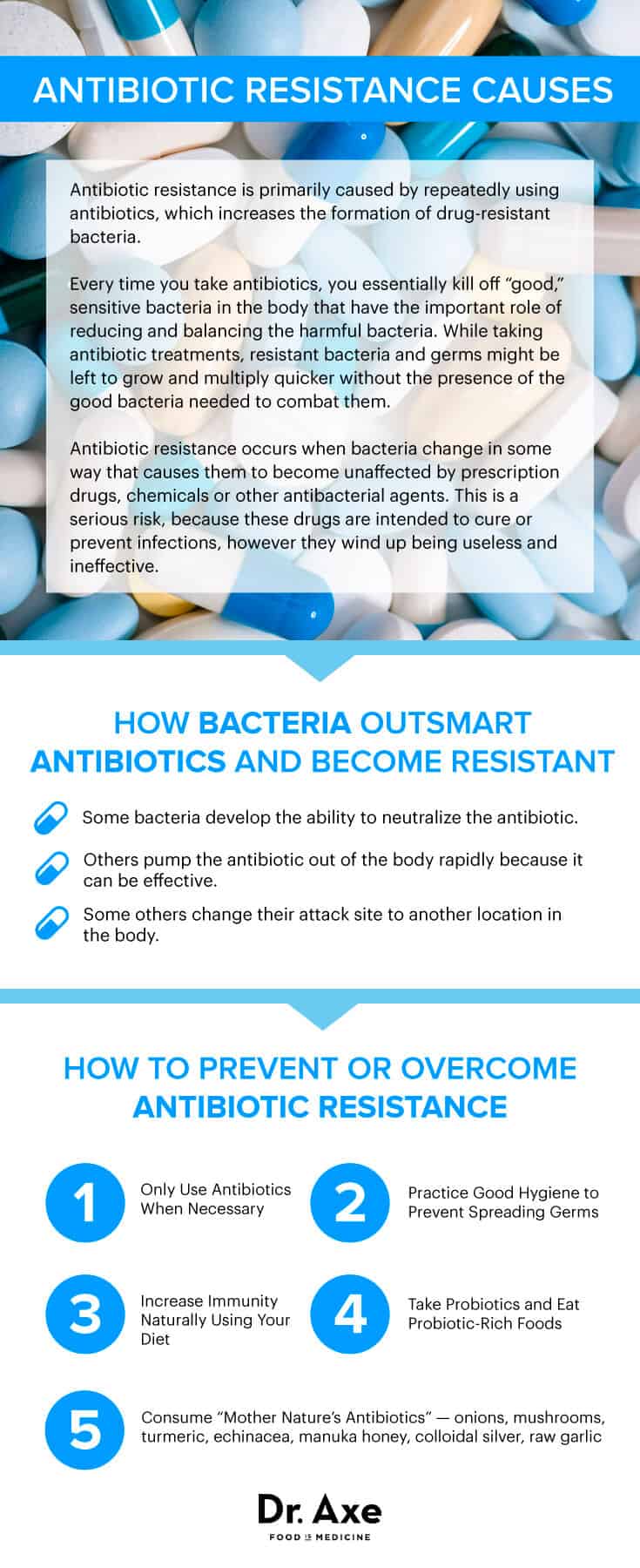
Antibiotic resistance is primarily caused by repeatedly using antibiotics, which increases the formation of drug-resistant bacteria.
Each of us is made up of trillions of tiny bacteria, some of which are beneficial and essential to our survival, while others are harmful when left unmanaged. Every time you take antibiotics, you essentially kill off “good,” sensitive bacteria in the body that have the important role of reducing and balancing the harmful bacteria. While taking antibiotic treatments, resistant bacteria and germs might be left to grow and multiply quicker without the presence of the good bacteria needed to combat them.
Antibiotic resistance occurs when bacteria change in some way that causes them to become unaffected by prescription drugs, chemicals or other antibacterial agents. This is a serious risk, because these drugs are intended to cure or prevent infections, but they wind up being useless and ineffective.
How do bacteria actually outsmart antibiotics and become “resistant”? There are a few ways this happens: Some bacteria develop the ability to neutralize the antibiotic, others pump the antibiotic out of the body rapidly because it can be effective, and others change their attack site to another location in the body.
Bacteria that were once susceptible to an antibiotic can mutate and essentially change DNA and genetic material to build their defenses. Even if a very small amount of bad bacteria become resistant, they can then multiply and replace all the bacteria that were killed off. All of these methods allow the harmful bacteria to continue to reproduce and cause harm.
Smart use of antibiotics is the key to controlling the spread of resistance. While antibiotics are needed at times to treat serious bacterial infections and certain life-threatening diseases, they’re not the proper, or only, treatment method for things like common viral infections, the common cold, most sore throats and the flu. There are natural steps you can take to beat the cold or flu and sore throat remedies for fast relief, in addition to many more ways to treat afflictions without antibiotics.
Today, millions of unnecessary antibiotics are prescribed every year for these types of conditions when they aren’t fully needed.
Dangers of Antibiotic Resistance
The WHO states that patients with infections caused by drug-resistant bacteria are generally at an increased risk of worse clinical outcomes and even death. These patients usually consume more health care resources than patients infected with the same bacteria who are not resistant to antibiotics.
In 2012, WHO reported a gradual increase in resistance to HIV drugs. Since then, further increases in resistance to first-line treatment drugs were reported, which might require using more expensive and intense drugs in the near future.
We are now seeing antibiotic resistance in some of the most widespread and threatening illnesses there are. In 2013, there were about 480,000 new cases of multidrug-resistant tuberculosis reported and identified in over 100 countries. This type of tuberculosis requires treatment that is much longer and more intense than for nonresistant TB. A high percentage of hospital-acquired infections are now caused by highly resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA).
Around the world, resistance to malaria, HIV, more common bacterial infections like gonorrhea, urinary tract infections, pneumonia, bloodstream infections and more have been reported. And the spreading or emergence of antibiotic resistance throughout from region to region could jeopardize important gains in controlling many types of diseases.
The risks of overly using antibiotics don’t stop there. Using antibiotics frequently has been:
Linked to Higher Increase for Heart Disease
Here’s an eye-opening statistic: The New England Journal of Medicine published an article that found taking Erythromycin, a commonly prescribed antibiotic, increases your risk of dying from a cardiovascular complication by 250 percent! (2)
Correlated with a Higher Cancer Risk
While antibiotics themselves haven’t been shown to cause cancer in humans, studies have found a link between higher antibiotic use and increased cancer risk, particularly with breast cancer. It’s been found that women who take antibiotics more frequently — anywhere between just one and up to 25 times over a 17-year period — appear to have an elevated risk of breast cancer. Researchers believe this is because of the effects of the antibiotics on immune function, inflammation, and metabolism of estrogen and phytochemicals. (3)
Creates a Higher Likelihood for Digestive Problems
“Good bacteria,” known as probiotics, are a large and important part of your immune and digestive systems. They keep the presence of bad bacteria under control and also help you digest your food properly, absorb nutrients, and provide feedback to your brain regarding your appetite, mood and so on.
When you’re low in good bacteria, due to taking antibiotics that work to reduce all types of bacteria within your gut, you can’t digest the foods you eat as well, and it’s common to experience symptoms like constipation, bloating, food sensitivities and more. You might also be at a higher risk for nutrient deficiencies because you can’t absorb phytonutrients, vitamins and minerals as well.
Increases Risk for Allergies
Some studies now point to the fact that use of antibiotics in children increases their risk for allergies, asthma and eczema. Children commonly face colds, ear, respiratory and sinus infections and are quickly given antibiotics to reduce symptoms, yet this has its consequences.
A 2009 study published in the Journal of Allergy and Clinical Immunology found that when antibiotics were used in the first year of a child’s life, there was an increased risk of asthma and eczema by the age of just 6 or 7. (4) The Centers for Disease Control and Prevention (CDC) report that 90 percent of upper respiratory infections are viral, and yet still more than 40 percent of the antibiotic prescriptions written each year are prescribed for such infections — even though we know antibiotics have no effects on viruses. (5)
Children are also at a high risk for developing food allergies, gut-related problems and digestive issues, especially if they don’t eat a nutrient-rich diet and weren’t breastfed. Research shows that many allergic reactions are actually caused by an unhealthy level of intestinal flora and built-up toxicity from poor digestion and a poor diet.
The immune response is influenced by the mucous membranes of the digestive lining, and children can develop something known as “gut and psychology syndrome” (GAPS). While this is certainly possible in adults too, children need to eat a proper GAPS diet and avoid toxins or unnecessary antibiotics even more so than adults since their immune systems and central nervous systems are still developing.
Increases Cost of Health Care and Jeopardizes Current Treatments
Antibacterial resistance increases the costs of health care because it forces medical professionals to use more complicated, long-term and risky treatments to handle illnesses that would otherwise be easy to combat. When bacterial infections become resistant to first-line drugs, more expensive therapies must be used for a longer duration of time.
This usually means extended hospital stays, increased health care costs, and an economic burden placed on governments, families and societies. At the same time, we are all put at a higher risk because antimicrobial resistances of all kinds (meaning resistance to not only bacteria, but other forms of medicine, too) means that prevention and treatment of many common infections — as well as surgeries, blood transfusions, organ transplants, cancer chemotherapy and more — become riskier.
5 Tips for Preventing Antibiotic Resistance
The invention of antibiotics in our medical system over 70 years ago has been one of the most significant and life-saving things to happen, but as you can see, the problem is that today antibiotics are widely overused. While they have helped thousands of people over the years and are necessary treatments for certain bacterial infections like pneumonia and serious wounds, they’re not useful for treating viral infections, coughs, or preventing the common cold or flu.
The bottom line is that every time you’ve taken prescription antibiotics in the past, you’ve not only killed bad bacteria causing your illness, but you’ve also killed off the good bacteria as well. To naturally help rebuild your gut environment where the majority of bacteria live, helping you to boost your immune system, there are several actions you can take.
1. Only Use Antibiotics When Necessary
If you’re sick and visiting your doctor, talk about different treatment options and ask whether an antibiotic is completely needed. There might be natural methods that are just as effective as an antibiotic, so don’t assume you need one or pressure your health care provider to prescribe.
- Don’t take an antibiotic for asthma symptoms, seasonal allergy symptoms, or viral infections like a cold, stomach virus or the flu. Keep antibiotic use to when it’s absolutely necessary and only to treat bacterial infections in order to prevent antibiotic resistance.
- Never share antibiotics and don’t save antibiotics to use at a later time to take when you’re sick again. Always throw away any pills that are left over after your treatment is over.
- Follow antibiotic prescription directions very carefully — don’t skip doses, double up on doses or stop without finishing the cycle.
2. Practice Good Hygiene to Prevent Spreading Germs
An essential part of preventing the spread of bacteria-causing illnesses or infections is a clean household and work environment. Make sure to wash your hands thoroughly, clean your kitchen and bathroom surfaces well, and avoid going to work when you’re sick.
Use natural antibacterial agents at home, including essential oils, to keep germs and bacteria away without the use of chemicals or drugs. Natural antibiotic oils are found in essential oils including oregano oil, lemon oil and helichrysum essential oil. Many of these oils also work as alternatives for natural allergy relief.
Using natural methods is a safer bet because a link between commercial antibacterial chemicals used in personal or household cleaning products and bacterial resistance has been shown in some studies.
3. Increase Immunity Naturally Using Your Diet
While it might seem hard to do at first or completely, removing the vast majority of grains, starches and sugar from your diet helps heal your gut and replenish good, protective bacteria. Grains, even whole grains, contain antinutrients and proteins like phytate, lectin and gluten that are difficult to digest.
These cause intestinal inflammation, and if you’ve already taken antibiotics several times in your life, you can’t afford to make matters worse in your gut microbiome. Consuming too much sugar in any form — even from grains or high levels of starches — feeds harmful bacteria and allows them to multiply more easily. Since these foods break down into simple sugars in the digestive tract, the bacteria can use them for fuel, which overloads your immune system and leaves you susceptible to bacterial infections and viruses.
You can try sprouted grain bread or these sandwich alternatives in place of most grains; also, begin to use natural sweeteners instead of sugar.
4. Take Probiotics and Eat Probiotic-Rich Foods
Probiotics have been studied for various health benefits, with one of their primary roles being to help reduce harmful and resistant bacteria within the gut while also increasing good bacteria. Their role in preventing drug-resistant infections is still being researched by the CDC, but it’s already been well-established that probiotics can help increase gut health and immune function in humans.
Probiotics are the “friendly” bacterial flora living inside of our digestive tracts that help us break down our foods and absorb immune-boosting nutrients that feed our brain and organs. In fact, these bacteria (or what are also really types of yeasts and molds) make up a whopping 70 percent to 85 percent of our immune system! This is why a healthier gut environment correlates with less illnesses, including the flu, asthma, head colds and UTIs.
Take a high-quality probiotic supplement regularly, especially if you’ve been on antibiotics. You can also easily eat probiotic-rich foods frequently that help balance your intestinal flora. To naturally build back the probiotics in your gut, I recommend you consume some of these top probiotic foods regularly: apple cider vinegar, cultured dairy products (amasai, kefir, goat milk yogurt or cultured probiotic yogurt made from raw cow’s milk), fermented vegetables (sauerkraut, kimchi, kvass) and probiotic beverages (kombucha, terrain herbals and coconut kefir).
Luckily, these healing foods are becoming easier to find in major grocery stores as knowledge about the many benefits of probiotics for gut health gain attention in the mainstream media.
5. Consume “Mother Nature’s Antibiotics”
Luckily for us, there are plenty of foods found in nature that have the ability to reduce harmful bacteria in our bodies, lower inflammation and increase the presence of protective bacteria. Aside from eating probiotic-rich foods, also make sure to get enough gut-building, allergy-fighting foods with “prebiotics.” These include things like onions, asparagus, raw chicory root, raw Jerusalem artichokes and dandelion greens. Also try to consume natural antibacterial foods:
-
- onions
- mushrooms
- turmeric (which contains curcumin)
- echinacea
- Manuka honey
- colloidal silver
- raw garlic
Raw garlic is one of the most beneficial and versatile antibacterials to reverse disease. It contains the compound called allison, which is antifungal, antibiotic and antiviral. Use raw garlic in recipes and consider taking up to one raw clove per day.
Oregano oil benefits are superior to prescription antibiotics as well. It’s a natural antiviral, antibacterial, antifungal, antiparasitic, antioxidant and anti-inflammatory food. Take 500 milligrams or five drops of 100 percent pure essential oil daily.
Finally, as a natural antiviral, colloidal silver benefits your immune system and alkalizes the body. Take one to two tablespoons daily for the best results.










