This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Peritonitis Causes & Symptoms + How to Get Your Health Back
January 9, 2018

Peritonitis is a serious infection or inflammatory response that can either be confined to the peritoneum (abdomen) or widespread. What can cause peritonitis? A number of things can trigger peritonitis. Peritonitis is usually caused by infection from bacteria or fungi that enter through a leakage or a hole in the digestive system, such as the intestines or bowels. The condition is most likely to affect people with weakened immune systems due to having other health conditions, although it can also affect people with no previous history of risk factors.
Can peritonitis be life-threatening? Yes, it can. This is why antibiotics are typically required during treatment, sometimes along with surgery. While antibiotics can be lifesaving, natural remedies like a healthy diet, rest and use of supplements can also help with prevention and supporting recovery by boosting overall health.
What Is Peritonitis?
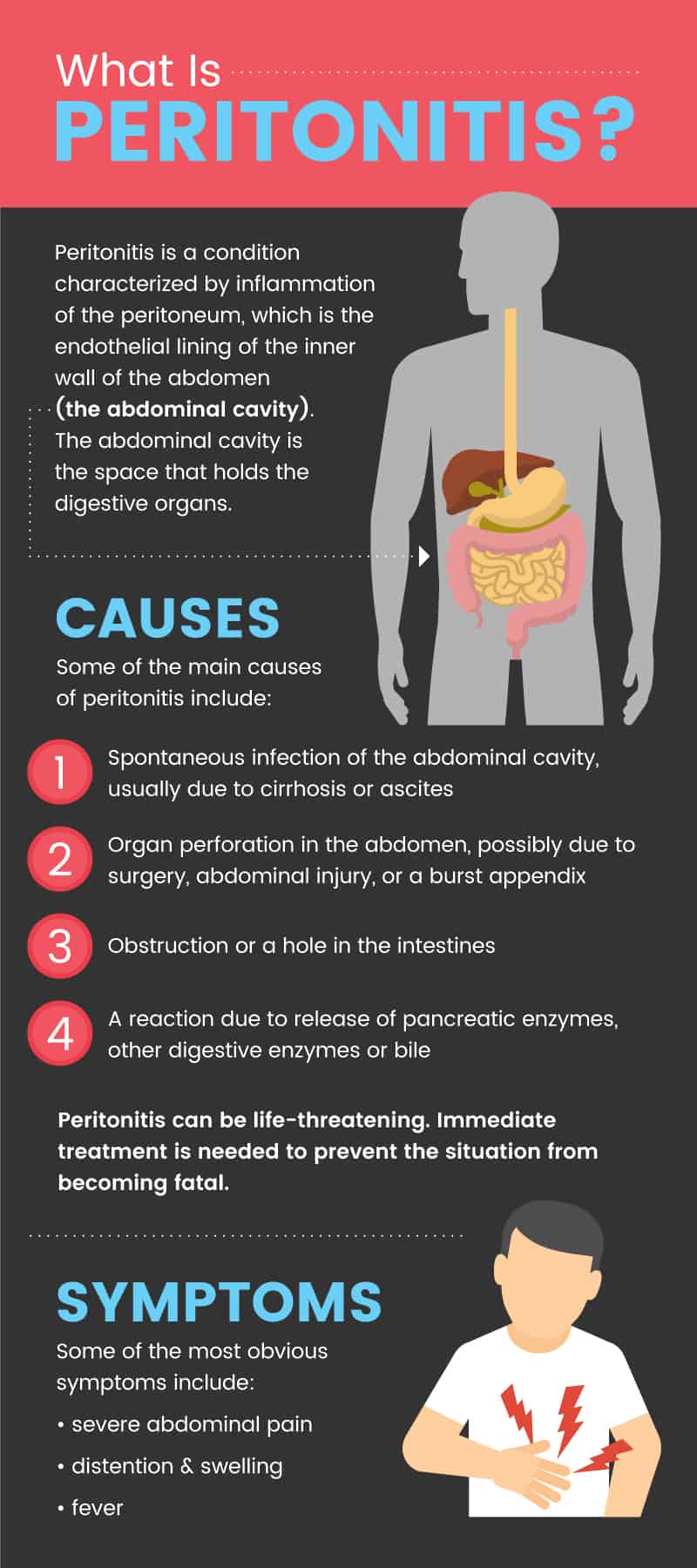
Peritonitis is a condition characterized by inflammation of the peritoneum, which is the endothelial lining of the inner wall of the abdomen (the abdominal cavity). (1)
The abdominal cavity is the space that holds the digestive organs. It is bordered by the abdominal wall, which is made of layers of skin, fat, muscle and connective tissue. The peritoneum covers the inside of the abdominal cavity as well as most of the abdominal organs, such as the liver, stomach and spleen. (2) As a serosal membrane, the peritoneum normally responds to stimuli, such as pathogens found inside the body, by causing an inflammatory response. When this response becomes greatly increased peritonitis occurs, causing symptoms like pain, swelling and abdominal distention.
There are two types of peritonitis: primary and secondary:
- Primary peritonitis is caused by a spontaneous infection (not related to perforation of the peritoneum). This is the less common type and most likely to affect people with cirrhosis of the liver or ascites, such as due to alcoholism. Infection can be due to genital tract bacteria or blood-borne bacteria proliferating in the peritoneum.
- Secondary peritonitis is due to loss of integrity of the peritoneum (damage to the mucosal barrier). This is the more common type of peritonitis and is usually related to some type of trauma to the abdominal organs.
- Meconium peritonitis is the type that can affect fetuses or newborns shortly after birth. This refers to inflammation and sometimes infection due to perforation of the intestines and meconium, the fecal material that is produced in the intestines before birth.
Signs & Symptoms of Peritonitis
The most common symptoms of peritonitis include: (3)
- Widespread abdominal pain and tenderness. This is due to a buildup of blood, bodily fluids, and/or pus in the abdomen causing swelling (inflammation). Sometimes pain will become very severe and cause the person to curl up into a ball.
- Stomach bloating (abdominal distention).
- Fluid in the abdomen, causing stiffness/rigidity of the abdominal muscles.
- Fatigue.
- Failure to tolerate drinking any fluids due to decreased urination and edema.
- Fever, nausea and vomiting.
- Constipation and failure to pass gas.
- Loss of appetite.
- Low blood pressure.
- Shortness of breath (if pressure expands up to the lungs).
- Swelling in the legs, especially in the ankles or feet.
Peritonitis Causes & Risk Factors
What are the causes of peritonitis? Some of the reasons that peritonitis can develop include:
- Spontaneous infection within the abdominal cavity. This most commonly affects people with liver cirrhosis (severe scarring of the liver) or ascites (the accumulation of protein-containing fluids in the abdomen). Risk factors for these illnesses include alcoholism, obstruction of the hepatic vein, and hepatitis. This is a very serious problem, with research showing that mortality due to peritonitis in patients with cirrhosis/ascites is between 30–90 percent within the first year of diagnosis.
- Organ perforation in the abdomen. This can include a leakage or a hole in the intestines that may be due to conditions like diverticulitis, injury to the abdomen, an ulcer, surgery or a burst appendix. This causes bacteria to enter the gastrointestinal tract, triggering an immune response and infection.
- Obstruction/perforation of the bowels. (4)
- A reaction due to release of pancreatic enzymes, other digestive enzymes or bile.
Below are some of the biggest risk factors for developing peritonitis:
- Having a weakened immune system, due to illnesses like lupus, hepatitis, kidney disease or kidney failure, liver disease, cancer, heart failure, pancreatitis or tuberculosis.
- Peritoneal dialysis, which is a treatment used to manage kidney failure that uses the lining of your abdomen to filter your blood. (5) Peritoneal dialysis involves having a dialysis solution flow from a bag through a catheter into the abdomen, helping to soak up waste and fluids. Peritonitis infection can sometimes occur if the “exit site” becomes infected or if the catheter becomes contaminated.
- History of ischemic bowel disorders or inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease.
- History of a ruptured appendix (appendicitis).
- Exposure to irritants, such as foreign bodies, bile from a perforated gall bladder or a lacerated liver, or gastric acid from a perforated ulcer.
- History of pelvic inflammatory disease. In this case an infection in the pelvis will spread up to the abdomen. (6)
- Hypertension and obesity, two factors related to metabolic syndrome.
- Taking medications or having hormone imbalances that affect fluid levels.
Peritonitis can also cause complications, which are sometimes life-threatening. The degree of complications depends on the specific type of peritonitis that a patient has, plus the underlying cause of the condition.
- The biggest risk associated with peritonitis is death, which is why vigorous, immediate treatment is needed to prevent the situation from becoming fatal.
- Other complications can include dehydration, acute respiratory distress, sepsis, renal/kidney failure, hypovolemic shock, abscess formation and bowel obstruction.
Peritonitis Diagnosis & Conventional Treatments
To diagnose peritonitis a doctor will usually first perform a physical exam. Patients will usually feel pain, pressure and tenderness when the abdomen is pressed, and the doctor may be able to feel stiffness and other signs of swelling. Blood tests, ultrasound, CT scan and X-rays may also be used to make a diagnosis and rule out other causes of pain.
- Once diagnosed, peritonitis needs to be treated right away since it’s considered an emergency situation. Treatment will usually involve use of antibiotics and sometimes surgery. (7)
- Antibiotics are usually taken in combination for about 5–10 days. One study found that when 90 patients with peritonitis were randomized to a 5- or 10-day course of cefotaxime, similar cure rates of of 90–93 percent were seen in both groups. (8) Antibiotics might be administered through an IV to help with rapid recovery of an infection.
- Surgery may be needed to repair an injury/perforation, to remove a ruptured appendix, or to seal any obstruction in the stomach or intestines.
- Diuretic medications might also be used to reduce fluid retention by helping the kidneys to excrete more urine. IV fluids, oxygen, electrolytes and analgesics might also be needed.
- A tube might need to be inserted into the nose that runs to the stomach in order to help drain secretions and gas/air that accumulate in the digestive tract. This is called a nasogastric tube.
- If the patient has a large amount of fluid accumulated in the abdomen, then a needle may need to be inserted in order to remove fluid and reduce the swelling, The fluid can also be sent for testing to confirm the cause of the condition. When fluid is removed from the abdomen by inserting a needle, the procedure is called therapeutic paracentesis.
5 Natural Ways to Boost Peritonitis Recovery
The following natural treatments for peritonitis are intended for helping with recovery and improving strength after use of antibiotics and/or a necessary stay at the hospital:
1. Get Extra Rest
After dealing with a very serious illness, you’ll need plenty of downtime to rest and recover. Your doctor might put you on bedrest for several days immediately following a peritonitis diagnosis. Once you’re feeling better, you should aim to get at least 8–9 hours of sleep per night, as well as to give yourself breaks throughout the day. If you’re experiencing swelling in your legs or feet, keep them elevated while you lie down and rest.
Don’t engage in any vigorous activities for at least several weeks. Keep any exercise light and restorative until your doctor clears you to do more. Try going for walks and stretching if it feels OK, but don’t do anything to wear yourself out or contribute to fatigue. It’s also normal to feel anxious and uncomfortable while overcoming peritonitis. Some stress relieving activities that might help you feel calmer and get better sleep include: meditation, reading, writing, listening to music and use of aromatherapy (such as with lavender essential oil or chamomile oil).
2. Eat A High Antioxidant, Low Salt Diet
Dietary intervention alone won’t help you to overcome peritonitis, so you will still need help from your doctor even if you plan to improve your diet. However, while you’re recovering, a healthy diet can prevent complications like dehydration or worsened inflammation. Here are dietary steps to help you recover from peritonitis:
- Avoid foods high in sodium, which can make fluid retention worse. This includes most packaged foods, fast food, fried foods, canned or frozen foods, soups, bottled dressings, processed meat and condiments. Speak to your doctor about how much to limit your salt intake and how long you will need to follow a salt-reduced diet. (9) It’s common for patients to need to decrease their dietary sodium intake to around 2,000 milligrams per day or less.
- Eat a variety of fruits and vegetables in order to get plenty of antioxidants. (10) Some high-antioxidant foods include fresh fruits like berries, leafy green veggies, carrots, tomatoes, squash, bell peppers, asparagus, sea vegetables, cocoa, acai, green tea and other veggies.
- Consume foods high in B-vitamins. These include quality animal proteins like meat or fish, eggs, almonds, beans/legumes, leafy green veggies, and whole grains
- Ask your doctor if it will be helpful to increase intake of high potassium foods, such as bananas, avocados, potatoes and greens. This may help with regulating blood pressure and fluid levels.
- Consume probiotic foods like fermented dairy (yogurt or kefir) or cultured veggies to help restore “good bacteria” in your gut. After taking antibiotics this can be helpful for digestion and improving recovery.
- Limit intake of inflammatory foods like added sugar, refined grains, refined vegetable oils, and packaged foods made with sodium, additives and preservatives.
- Avoid caffeine, alcohol, and tobacco. Once you’re feeling better, ask your doctor if it is safe to add moderate amounts of alcohol or caffeine back in.
3. Eliminate Excess Fluid Intake
Consuming too much fluid can make abdominal swelling, edema and distention worse. Immediately after peritonitis is diagnosed you may need to limit the amount of water and fluids you consume, but while you are recovering you should aim to drink six to eight glasses of filtered water daily to prevent dehydration. If you notice fluid retention getting worse, or you feel dizzy or have other signs of dehydration, talk to your doctor. If you do need to limit fluid intake for a while and are dealing with symptoms like dry mouth, then you can try sucking on mints or gum, brushing your teeth, gargling water and using lip balm to help.
4. Limit Inflammation With Supplements & Herbs
- Check with your doctor first before taking any supplements to make sure they will not interact with any medications you’re using.
- If cleared by your doctor, take a quality multivitamin to prevent nutrient deficiencies, especially if you are eating less due to discomfort. Your multivitamin should provide vitamins A, C, E, B-complex vitamins, magnesium, calcium, zinc and selenium.
- Take a probiotic supplement to help replenish good bacteria in your gut after taking antibiotics.
- Consider seeing a specialist in homeopathy who can recommend herbs to take. Herbs that may be helpful include adaptogen herbs like ashwagandha.
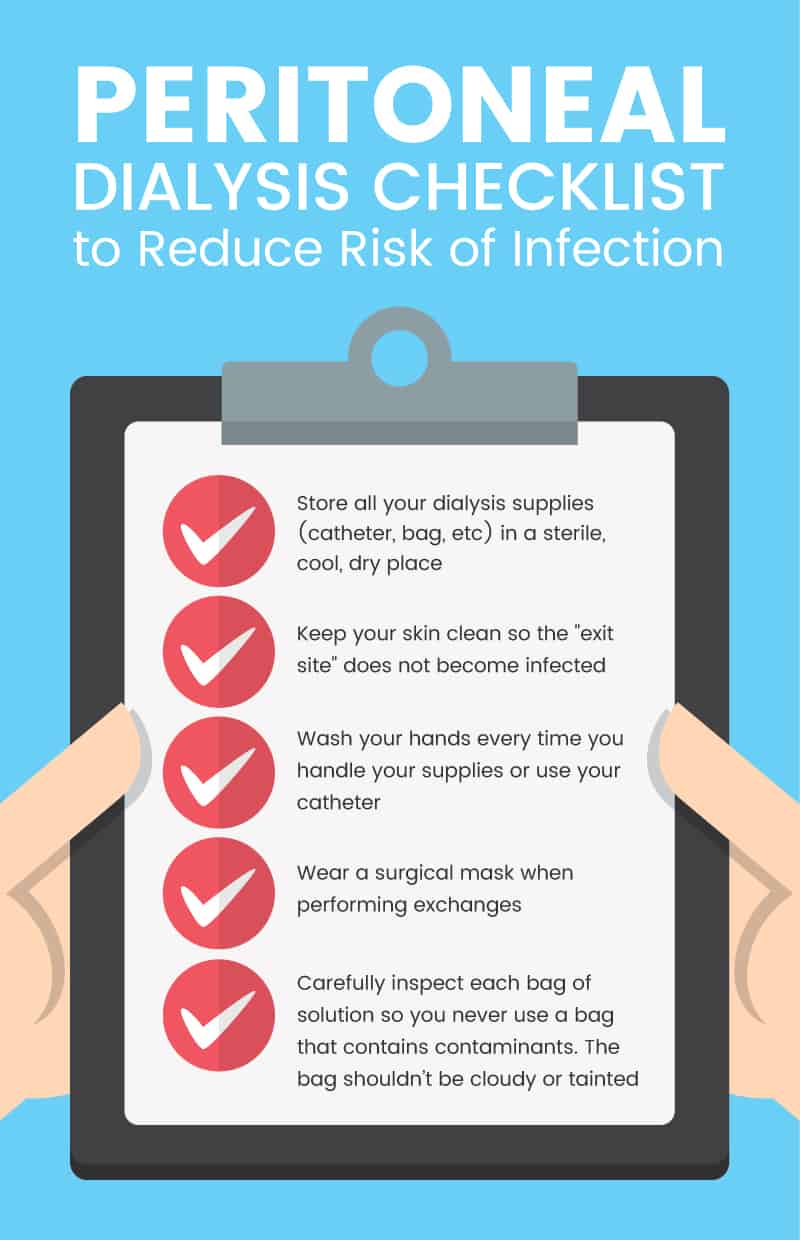
5. Prevent Infection & Contamination if Performing Peritoneal Dialysis
If you use peritoneal dialysis to manage kidney failure, there are certain steps you can take to reduce your risk for infection: (11)
- Store all your dialysis supplies (catheter, bag, etc) in a sterile, cool, dry place.
- Keep your skin clean so the “exit site” does not become infected.
- Wash your hands every time you handle your supplies or use your catheter.
- Always carefully inspect each bag of solution so you never use a bag that contains contaminants. The bag should not appear cloudy or tainted.
- Wear a surgical mask when performing exchanges.
Precautions Regarding Peritonitis Treatments
Peritonitis is a medical emergency that must be treated immediately. If you experience any symptoms of peritonitis (severe abdominal pain, distention and swelling, fever, etc.) always go to the emergency room or visit your doctor right away. Rapid treatment is critical for preventing serious complications, including permanent scarring and death.
Key Points on Peritonitis
- Peritonitis is a life-threatening condition characterized by inflammation of the peritoneum, which is the endothelial lining of the inner wall of the abdomen.
- Causes of peritonitis can include: spontaneous infection, obstruction of the intestines or bowels, diverticulitis, pancreatitis, appendicitis, liver disease or infection due to peritoneal dialysis.
- Peritonitis is treated with antibiotics, sometimes surgery, and sometimes diuretics or use of intravenous fluids.
5 Natural Ways to Improve Peritonitis Recovery:
- Rest.
- Limit fluids
- Lower anxiety and pain
- Prevent dehydration
- Eat a low salt diet.
- Manage peritoneal dialysis carefully to avoid contamination.