This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Relieve Your Child’s Bronchiolitis Symptoms 7 Natural Ways
January 28, 2018

Bronchiolitis is a lung infection most often seen in young children. It can affect people at any age but is most likely to cause serious or noticeable symptoms in infants and toddlers. The infection is common and involves inflammation and congestion in the tiniest airways in the lungs (called the bronchioles). It is usually caused by a virus.
Most people with bronchiolitis get better within a few weeks, but some children may need care in a hospital.
What Is Bronchiolitis?
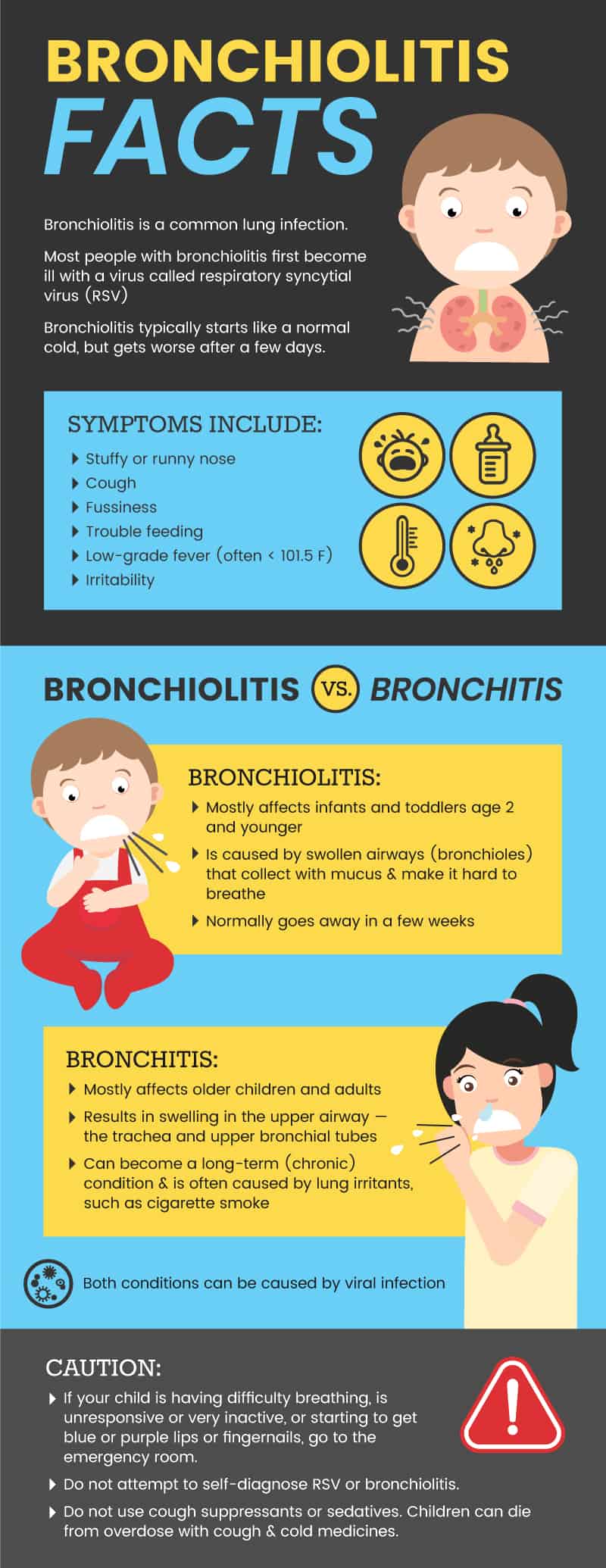
Bronchiolitis is a common lung infection. Most people with bronchiolitis first become ill with a virus called respiratory syncytial virus (RSV). While the virus can make people of any age sick, RSV in babies can cause severe bronchiolitis symptoms that may require hospitalization. (1)
Bronchiolitis typically starts like a normal cold, but gets worse after a few days. It can cause a week or more of wheezing or trouble breathing even in otherwise healthy kids. (2) Children may also get an ear infection that requires antibiotics. (3)
Is bronchiolitis contagious?
Bronchiolitis itself is not contagious. However, the viruses that can cause bronchiolitis are contagious. The viruses are very common and spread easily through coughs, sneezing, talking or touching shared objects. RSV has at least two strains and infects nearly every child by the age of 2. (4) Other viruses, such as the flu and the common cold, can also lead to bronchiolitis if they cause the bronchioles to swell and fill with mucus. (5)
Bronchiolitis vs. bronchitis
There is a difference between bronchiolitis and bronchitis, even though the conditions have similar names. They have similar effects on the actual airways, but in different parts of the lungs and in people at different ages.
Bronchiolitis mostly affects infants and toddlers age 2 and younger and is caused by swollen airways (bronchioles) that collect with mucus and make it hard to breathe. Bronchitis mostly affects older children and adults. It results in swelling in the upper airway — the trachea and upper bronchial tubes. (6) In addition, bronchiolitis normally goes away in a few weeks, whereas bronchitis can become a long-term (chronic) condition and is often caused by lung irritants, such as cigarette smoke. (7) However, both conditions can be caused by a viral infection.
Signs & Symptoms
Bronchiolitis symptoms in infants may be difficult to identify. Symptoms include: (8, 9)
- Stuffy or runny nose
- Cough
- Fussiness
- Trouble feeding
- Low-grade fever (often < 101.5 degrees F)
- Irritability
In some cases, these are the only symptoms a child may have of bronchiolitis. In other cases, symptoms get worse.
Call a doctor or take your child in for urgent care if you notice any of the following symptoms: (10, 11)
- Sluggishness or extreme inactivity
- Refusing to eat or drink
- Dehydration (not enough wet diapers, or having dark urine)
- Trouble breathing:
- Wheezing
- Nostril flaring
- Whistling noises on the exhale
- Seeing the ribcage go in when the baby breathes in
- Breathing very fast or shallow
- Working very hard to breathe
- Pauses in breathing
- Blue or purple lips or fingertips
- Hypothermia (a temperature that is lower than the normal 98 degrees F)
Bronchiolitis in toddlers and bronchiolitis in adults may cause many of the same symptoms, although sunken ribs during breathing and nasal flaring are most likely to occur only in the very young. (12)
Causes & Risk Factors
Bronchiolitis causes include: (13)
- A virus (most often RSV, but it can also be the common cold or flu)
- Swollen airways that fill with mucus
When the infection causes the airways to swell and fill with mucus, the lungs have trouble getting enough oxygen into the blood. The body then has to work harder to get enough oxygen, which causes trouble breathing, such as wheezing or sucked-in ribs.
Risk factors for bronchiolitis include: (14)
- Age younger than 2 years (and younger than 3 months in particular)
- Preterm birth
- Another heart or lung problem
- A weak immune system
- Exposure to cigarette smoke
- Exposure to lots of other kids or people (in a daycare or crowded home)
- Having older siblings who attend school or daycare
Conventional Treatment
In most cases, bronchiolitis treatment simply involves staying hydrated and resting at home. Most children have mild symptoms and do not require treatment. However, when bronchiolitis becomes severe, conventional treatment may involve: (15, 16)
- Hospitalization
- Oxygen via a mask or machine
- A nebulizer, to deliver inhaled drugs that open up and reduce inflammation in the tiny airways of the lungs
- Intravenous (IV) fluids to help hydrate
- Suctioning mucus from the mouth or nose
- Monitoring breathing and heart rate with a machine
- Making sure your child’s temperature stays in a healthy range
Oxygen is considered the most effective treatment in young children. (17) Because most bronchiolitis is the result of a virus, antibiotics are not usually prescribed. In some cases, certain drugs may be recommended by health care providers for treatment, including: (18, 19)
- Drugs to treat RSV infection, such as ribavirin or palivizumab
- Antibiotics (if the infection was indeed bacterial or if there is also an ear infection)
- Decongestant sprays
- Corticosteroids, such as prednisone
- Alpha or beta agonists to help relax and open the airways, such as albuterol or racemic epinephrine
- Fever reducers, such as acetaminophen or ibuprofen, depending on the child’s age. (If you are considering using medication to reduce your child’s fever at home, talk to a healthcare professional due to serious safety concerns.)
7 Natural Ways to Relieve Bronchiolitis Symptoms
In fighting mild cases of bronchiolitis, the focus is on increasing how much oxygen gets into the body, staying hydrated, and relieving symptoms like congestion and fever. (20)
You can consider these natural ways to relieve bronchiolitis symptoms when your child’s symptoms do not require medical attention:
- Use a humidifier
- Stay hydrated
- Use aromatherapy
- Keep the airways clear
- Relieve the fever
- Consider Traditional Chinese Medicine
- Ask about dietary supplements or at-home natural nebulizer options
1. Use a humidifier
Supplemental humidified oxygen is one of the standard hospital treatments for bronchiolitis. (21) Use of a humidifier is also considered a safe temporary way to improve ease of breathing for your child. (22) However, humidifiers can be associated with respiratory infections and other problems when they are not used properly or are not clean. Follow the instructions for use included with the humidifier and clean it daily during your child’s illness.
At home, it is also commonly recommended that you avoid potential irritants in the air, such as: (23)
- chemicals
- smoke
- fumes
- dust
- allergens
- cold air
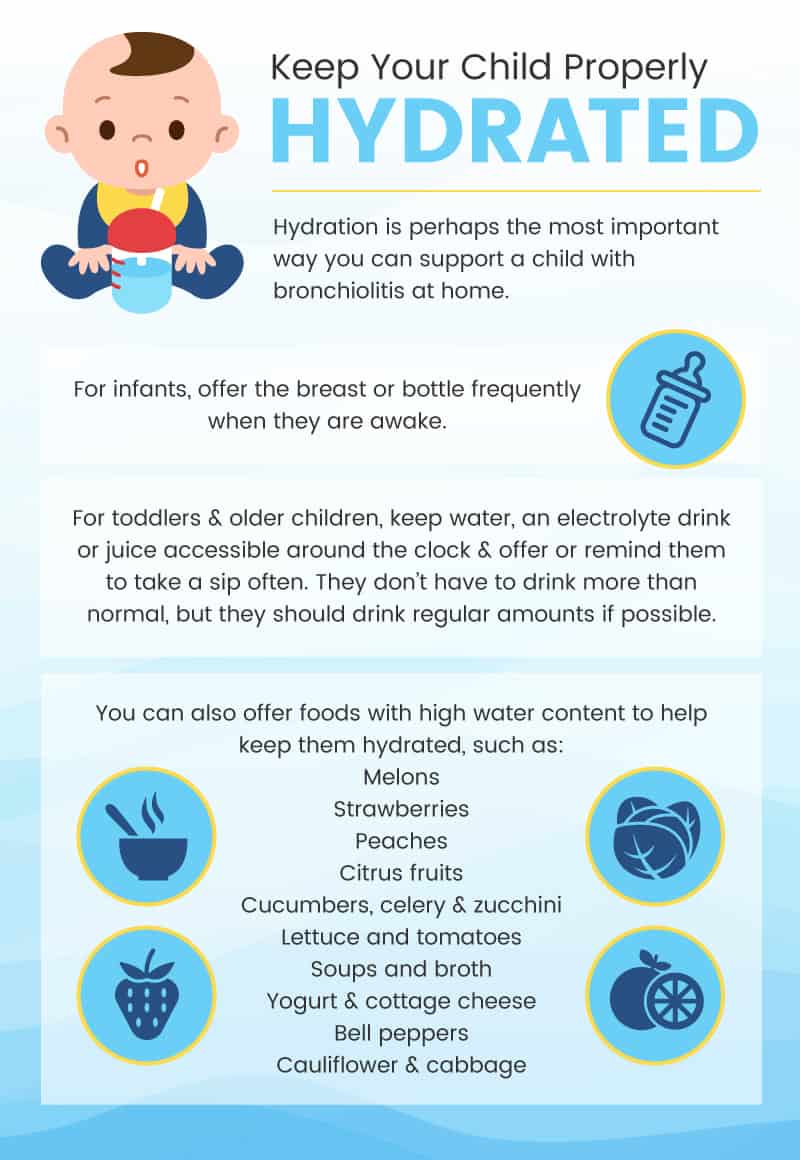
2. Stay hydrated
Hydration is perhaps the most important way you can support a child with bronchiolitis at home. (24) For infants, offer the breast or bottle frequently when they are awake. For toddlers and older children, keep water, an electrolyte drink or juice accessible around the clock and offer or remind them to take a sip often. They don’t have to drink more than normal, but they should drink regular amounts if possible. (25) If you are worried that your child is not eating or drinking enough, call a health care professional. Doctors may recommend an over-the-counter (OTC) electrolyte drink made specifically for children or may tell you to bring your child into the hospital for IV fluids.
If your child is more interested in food than drink, you can also offer foods with high water content to help keep them hydrated. Hydrating foods include: (26)
- Melons such as watermelon and cantaloupe
- Strawberries
- Peaches
- Citrus fruits
- Cucumbers, celery and zucchini
- Lettuce and tomatoes
- Soups and broth
- Yogurt and cottage cheese
- Bell peppers
- Cauliflower and cabbage
3. Use aromatherapy
Although the jury is still out on exactly how helpful essential oil-based aromatherapy is for improving breathing in bronchiolitis, it is possible it may temporarily relieve symptoms. The one with the most bronchiolitis-specific research is probably eucalyptus oil.
- In one study, symptom relief occurred 20 minutes after using a spray with a combination of essential oils was greater than when a placebo spray was used. (27) The spray didn’t impact how long symptoms such as sore throat, hoarseness or cough lasted or how bad they were overall, but it did temporarily provide relief. The study used a combination of Eucalyptus citriodora, Eucalyptus globulus, peppermint, oregano and rosemary.
- A study in rats found that Eucalyptus globulus oil helped fight chronic bronchitis by relieving inflammation and fighting airway mucus. (28) Another study, also in rats, found similar results in the bronchioles. (29) A third study in rats found that eucalyptus oil fought bronchiolitis and helped reduce inflammation and mucus production. (30) Although those researchers believe eucalyptus oil should be considered for drug development, it is not yet used as one in traditional medicine.
- Note! Commercial vapor rub products may be dangerous for infants and young toddlers. (31) Do not apply it to very young children. For older children and adults, do not apply it near the mouth or nose. A study found that the ingredients in one popular brand, Vicks VapoRub, can cause irritation in the airways. This can cause more mucus production and trouble breathing. (32) This may be due to camphor, which can be toxic even in small doses to young children. (33)
- You can make your own vapor rub that leaves out potentially harmful ingredients. Instead of menthol and camphor, you can use peppermint and eucalyptus.
In general, there is no strong evidence that aromatherapy helps kids with bronchiolitis. However, parents who wish to use aromatherapy can likely do so knowing it is not likely to do any harm. (34)
4. Keep the airways clear
If your child is congested, you may wish to clear their nose or mouth of mucus. This can make it easier for them to draw air in and can impact how much oxygen they get into their blood. (35)
Home suction tools include suction bulbs and other over-the-counter options, such as “snot suckers” like the Nose Frida. If your baby’s mouth is full of mucus you can carefully use suction bulbs to clear their mouth a bit as well. (36)
Saline drops for your child’s nose can also be used to help clear their nose of mucus so they can breathe clearly. (37) For infants, saline drops should be used before using nose suction, so that the mucus breaks down and is easier to suction out. Older kids can use saline nose drops before blowing their nose so that they get more out.
5. Relieve the fever
If your child has a fever associated with their RSV or bronchiolitis, talk to his or her doctor about the best way to treat it. (38) In some cases, very young babies can easily become hypothermic — the opposite of a fever, when their temperature drops too low. This means you must be very careful when trying to bring down a fever. However, there are several ways to relieve a fever naturally that may be safe for infants and toddlers as well as older kids and adults. Simple tips include avoiding over-bundling with clothes or blankets and taking a lukewarm bath.
6. Consider Traditional Chinese Medicine (TCM)
Traditional Chinese herbal therapies are still widely used in China for the treatment of bronchiolitis and RSV. Although they are not widely accepted as formal treatments in the U.S., it is possible that a professional TCM practitioner could provide an herbal therapy that may relieve symptoms or fight underlying RSV.
- About 75 percent of 286 parents whose children had bronchiolitis were satisfied with and preferred TCM to conventional drugs. (39)
- In a review of complementary and alternative therapies for infant bronchiolitis, four studies of Chinese herbal medicine were included and showed some benefit for clinical outcomes. (40)
- A study in mice found that a TCM herbal treatment, called modified dingchuan decoction, which is often used for coughs and other respiratory problems, may fight RSV and reduce inflammation. (41)
- Studies using human respiratory tract cells found that Peuraria lobata Ohwi (found in both Ge-Gen-Tang and Sheng-Ma-Ge-Gen-Tang) fights RSV infection. (42)
7. Ask about dietary supplements or at-home natural nebulizer options
Although many dietary supplements may not be practical (or safe) to give to infants, you can ask your child’s doctor about child-safe options that may help them fight infections and reduce swelling in the airways. In some cases, it may be possible to give these natural dietary elements through a nebulizer.
A review of research on complementary and alternative medicines for infant bronchiolitis found studies with promising results for the following: (43)
- Vitamin D. Research supports the idea that vitamin D plays an important part in our immune system’s ability to fight viral infections.
- In a study of infants with serious bronchiolitis, many had a genetic mutation that may make it harder for their bodies to use vitamin D to fight infection. (44) The researchers suggested that higher levels of vitamin D in their systems may make it easier for the children with this mutation to get the amount they need to help control inflammation and fight the virus.
- Other research also suggests that vitamin D deficiencies can be treated to reduce the risk for serious respiratory infections in young children. (45, 46)
- Vitamin D drops are available over the counter for infants and toddlers.
- N-acetylcysteine. This is an amino acid cysteine taken by mouth that is believed to help give cells an important antioxidant. (47)
- A study of N-acetylcysteine given through a nebulizer found that it helped kids feel better faster and get sent home from the hospital earlier than children given salbutamol. (48)
- N-acetylcysteine is available over the counter in pill form, which may not work for young kids. Talk with a healthcare professional about possible ways to get N-acetylcysteine safely as a supplement or nebulizer treatment for your child if you are interested.
- Magnesium. Research indicates the body may lose magnesium in the urine during illness; magnesium levels in the blood are lower and levels in the urine are higher in children at the start of illness, with the reverse by the end. (49) Several randomized trials have started to look at nebulized magnesium sulfate as an option for treating bronchiolitis.
- One study found that it was not helpful (and may be harmful) when given into the vein (via IV at the hospital). (50)
- Another study found that when magnesium sulfate was combined with salbutamol in nebulizers, it improved symptoms more than just magnesium sulfate alone. (51)
- Magnesium sulfate given via a micro air pump was also found to be helpful in another study (compared to given into the vein). (52)
- Ask your child’s doctor about a possible magnesium sulfate supplement or nebulizer if you are interested, but do not try this treatment without the guidance of a health professional. (53)
Prevention
RSV infections occur in nearly everyone by the age of 2. The best way to prevent it is to take steps to avoid any type of contagious infection: wash your hands, limit contact with people who are sick, clean surfaces like toys and doorknobs, cover your nose and mouth when coughing or sneezing, and don’t share cups or utensils. (54) You can also follow these steps:
- Do not smoke in the home or around your child. (55)
- Breast-feed your baby to help protect him or her from RSV. (56)
- When you or another adult in the house have a cough or fever, take extra precautions and consider wearing a face mask. (57)
- Since the flu virus can also cause bronchiolitis, the Mayo Clinic recommends everyone over the age of 6 months get a flu shot every year. (58)
- Consider a vitamin D supplement of 400 IU/day for kids under the age of 1, and 600 IU/day for children over the age of 1. (59)
Children who are born prematurely or who have other risk factors, such as a heart or lung condition or a problem with their immune system, may be offered a medication (palivizumab) to help reduce their risk of getting RSV. (60)
Precautions
- If your child is having difficulty breathing, is unresponsive or very inactive, or starting to get blue or purple lips or fingernails, go to the emergency room.
- Bronchiolitis can sometimes be very serious in young children. When in doubt, consult a health care professional or seek urgent or emergency care.
- Do not attempt to self-diagnose RSV or bronchiolitis. Its symptoms can be easily confused with pneumonia and other respiratory illnesses.
- Do not use cough suppressants or sedatives. (61) Children can die from overdose with cough and cold medicines. Sedatives can make it even harder for your child to get enough oxygen. Coughing is also important to help your child clear mucus from their lungs.
- Do not use products with camphor or menthol, such as many over-the-counter vapor rubs.
- For over-the-counter pain and fever relief, follow the product’s weight-based instructions. If your child is too small or young to be listed on the package instructions, call a doctor to ask about a safe dose.
- If you are using at-home herbal remedies for your child, proceed with caution. Young children may require smaller doses of remedies or may have negative reactions to herbs, supplements, carrier oils, and other products used for at-home care.
Bronchiolitis Key Points
- Bronchiolitis is a very common childhood illness that usually resolves on its own within a week.
- Common symptoms include coughing, congestion, wheezing and a low-grade fever.
- The problem is most common in babies and toddlers and is usually caused by a virus called RSV.
- Most children do not require treatment other than rest and hydration. Some may require pain or fever relief.
- Take your child to an urgent care center or emergency room if they have trouble breathing.
Natural ways to treat mild bronchiolitis at home include:
- Use a humidifier.
- Stay hydrated.
- Use aromatherapy.
- Keep the airways clear.
- Relieve the fever.
- Consider Traditional Chinese Medicine.
- Ask about dietary supplements or at-home natural nebulizer options.