This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Worse Than Gingivitis: Periodontitis Causes & Symptoms (+ 5 Natural Remedies)
August 18, 2018

Periodontitis is an infection or inflammation (swelling) of the bones and ligaments that support your teeth. It happens with gum swelling or infection, also known as gingivitis, goes untreated. The problem spreads from the gums into the support structures of your teeth. It can cause your teeth to loosen and even fall out. The condition is fairly common but its symptoms should not be ignored.
Thankfully, effective treatments are available for periodontitis. There are even many drug-free treatment options for this dental problem. Better still, the condition is preventable. Learn how to protect your teeth and treat periodontitis.
What Is Periodontitis?
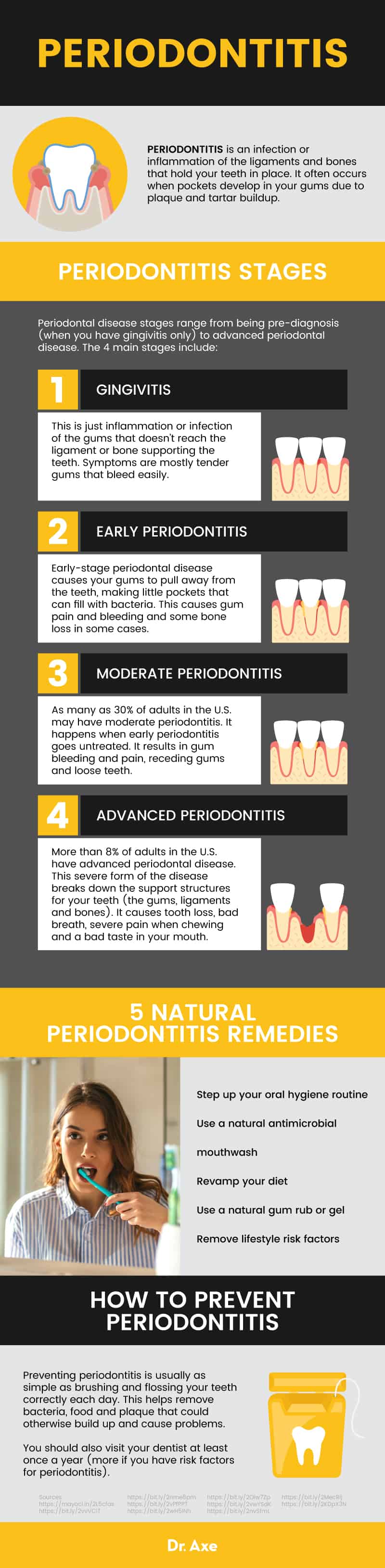
Periodontitis is an infection or inflammation of the ligaments and bones that hold your teeth in place. It often occurs when pockets develop in your gums due to plaque and tartar buildup.
There are multiple types and stages of periodontitis: (1)
- Chronic periodontitis is the most common type. It mostly affects adults and is due to poor oral hygiene and plaque buildup. Problems develop slowly over time. The condition affects almost half of all adults in the U.S. aged 30 or older. (2)
- Aggressive periodontitis can begin in children or young adults and quickly causes problems with bone damage and lost teeth unless it is treated. It runs in families.
- Necrotizing periodontal disease happens when lack of blood supply to the gums and tooth support structures causes tissue death and serious infection. It mostly happens in people with other health problems, such as weak immune systems or malnutrition.
Periodontitis vs. Gingivitis
Periodontitis occurs in some people who have gum disease, also known as gingivitis — inflammation or infection of your gums — when the infection spreads from the gums to the bones and ligaments. Gingivitis is a precursor to periodontitis. Periodontitis can happen when gingivitis goes untreated or advances due to ineffective treatment.
Symptoms
Symptoms of periodontitis overlap with many gingivitis symptoms and include: (1, 3)
- Gums that are swollen or puffy
- Gums that are red or purple and shiny
- Bleeding gums when you brush or eat
- Teeth that appear long
- Receding gums or gums that have pulled away from the teeth
- Tender or painful gums
- New gaps developing between teeth or a change in the way they fit together when you bite
- A change in how partial dentures fit
- Sensitive teeth
- Loose teeth or teeth that have fallen out
- Pus in your gums or between your teeth
- Bad breath
- Pain when chewing or brushing
Periodontitis Stages
Periodontal disease stages range from being pre-diagnosis (when you have gingivitis only) to advanced periodontal disease. The four main stages include: (2, 5)
- Gingivitis — this is just inflammation or infection of the gums that doesn’t reach the ligament or bone supporting the teeth. Symptoms are mostly tender gums that bleed easily.
- Early periodontitis — Early-stage periodontal disease causes your gums to pull away from the teeth, making little pockets that can fill with bacteria. This causes gum pain and bleeding and some bone loss in some cases.
- Moderate periodontitis — As many as 30 percent of adults in the U.S. may have moderate periodontitis. It happens when early periodontitis goes untreated. It results in gum bleeding and pain, receding gums and loose teeth.
- Advanced periodontitis — More than 8 percent of adults in the U.S. have advanced periodontal disease. This severe form of the disease breaks down the support structures for your teeth (the gums, ligaments and bones). It causes tooth loss, bad breath, severe pain when chewing and a bad taste in your mouth.
Related: What Is the Oral Microbiome? How to Balance It to Improve Overall Health
Causes
Periodontitis causes include gum and bone infection and inflammation. When gingivitis isn’t treated properly, it can cause full-blown periodontal disease. This happens because bacteria stay on the teeth and form plaque. If the plaque is not cleaned off, it hardens to what is called tartar or calculus. This causes swollen, irritated gums to develop pockets of space, allowing the film of hardened bacteria to spread from the teeth to underneath the gums. This makes it harder to clean, and the condition progresses to periodontitis if the trapped tartar is not cleared away by a dentist.
Risk factors for periodontitis include: (1, 4)
- Poor oral hygiene
- Gingivitis
- Older age
- Not having regular dentist visits
- Being male
- Living in poverty
- Having less than a high school education (if you are an adult)
- Smoking or chewing tobacco
- Drug or alcohol abuse
- Obesity
- Diabetes, Crohn’s disease, rheumatoid arthritis, leukemia, HIV/AIDS and certain other diseases
- Treatment with drugs that lower your immune function or that cause dry mouth
- Hormone fluctuations caused by pregnancy, birth control or menopause
- Poor nutrition or vitamin C deficiency
- Genetics
- Crooked teeth
- Stress
- Fillings that are loose or defective
Conventional Treatment
Provided gingivitis has not turned into periodontitis yet, you can treat the gum inflammation and infection using proper mouth and teeth cleaning. With regular visits to the dentist (at least once per year) for professional cleanings and at-home brushing and mouth rinses, plus flossing, gingivitis can be reversed without medication.
If the disease has progressed to periodontitis, early stages can often be treated with deep cleaning of the surfaces below the gums, at the root of the teeth. The dentist scrapes away the tartar and helps clear out bacteria trapped in the gum pockets. This is called scaling and may be done with a dental tool, ultrasonic device or a laser. (6)
For more periodontitis treatments at more advanced stages of disease, you may have scaling done as well as root planing. This involves smoothing the root surfaces to help avoid future tartar buildup. You will likely also be given antibiotic medication directly under the gums or as a medicated mouth rinse to treat infection. You may also need an oral antibiotic pill. In cases of severe damage or loose or missing teeth, you may need corrective surgery.
Surgical periodontitis options
Surgical treatments include: (6)
- Pocket reduction or flap surgery. The periodontist (a dentist who specializes in periodontal health issues) makes cuts in the gums to better clean the roots of the teeth and plane the bone. This helps the tissue heal and makes the gums easier to clean after the gums are stitched back together.
- Gum grafts (soft tissue grafts). Receding gums may leave too much of your teeth exposed. Tissue from the roof of your mouth or a donor can be attached to your gumline to shore it up and help avoid further gum recession. It can also improve the look of your gums.
- Bone grafts. If the bone holding your teeth in place has been damaged, small bone pieces of your own or from man-made bone or donor bone can be put in to help hold your teeth in place. The added bone can also work as a support structure for your own body to regrow bone.
- Guided tissue regrowth. Other options for regrowing bone and tissue include using a special fabric barrier between your bone and tooth to guide the regeneration of bone and tissue. Alternatively, tissue-stimulating gel proteins or collagen matrices can be applied to the tooth root to help it grow back healthy tissue and bone.
Natural Remedies
Many periodontitis treatments for early periodontal disease do not involve drugs. If you wish to supplement conventional treatment for periodontitis, consider these other natural options:
-
Step up your oral hygiene routine
Regardless of whether you’re getting care from a periodontics professional, it’s critical to keep your mouth as clean as possible. You can fight the disease and boost the impact of professional treatments this way.
- Brush at least twice each day. If you can, brush after each time you eat or have a sweetened drink.
- According to the American Dental Hygienists’ Association, you should use a soft toothbrush and hold it at a 45-degree angle to your teeth up at the gum line. (7)
- Gently brush back and forth and roll it downward periodically. Brush two or three teeth at a time.
- Brush all tooth surfaces and gently brush the gumline if you can.
- Tip the brush straight up and use up-and-down strokes to brush behind the front teeth.
- Brush your tongue from back to front.
- Replace the toothbrush at least every three months.
- Consider a probiotic toothpaste, as some early research suggests probiotic mouth products may also fight plaque effectively.
- Floss at the end of the day to remove food particles and bacteria.
- Don’t skip brushing or flossing — even if you’re tired or busy.
- If your gums are too sensitive for flossing, ask your dentist about oil pulling.
- This is a floss-free alternative for removing food and bacteria from your mouth that you may prefer. It may help fight plaque and reduce symptoms of gingivitis within a week of daily use. It’s plaque-fighting effects continue to improve for at least a month with daily use. (8)
- Coconut oil is commonly used for this process, which involves putting a tablespoon or so of the oil into the mouth and swishing it around until it is thin and milky-white. Then spit it out without swallowing.
- Sunflower oil or sesame oil have also been effective in research studies of oil pulling.
-
Use a natural antimicrobial mouthwash
Herbal mouth rinses can have potent antibacterial and antimicrobial effects. In several studies, they have reduced the symptoms and signs of periodontitis and gingivitis. In many cases, they perform just as well as conventional mouthwashes recommended to people with periodontitis. (9, 10, 11)
Consider creating your own mouthwash using one of the following recipes:
- Dr. Axe’s homemade mouthwash
- Hydrogen peroxide (3 percent), in equal proportions to water, plus a bit of honey and a few drops of essential peppermint oil (12)
- Salt water (yes, just stir some sea salt into lukewarm water)
- Essential oil mouthwash, combining a cup of warm water with a few drops of lemongrass essential oil or tea tree oil, both of which can fight plaque and gum symptoms (13)
- Undiluted aloe vera juice (13)
-
Revamp your diet
Diets high in carbohydrates can promote the growth of bacteria in the mouth. However, there is no formal recommendation for a diet to fight periodontitis once it is established. Research suggests the ideal periodontitis diet probably involves an overall balance but includes: (14, 15)
- Low amounts of refined sugars
- High fiber, fruits and vegetables
- Fish oils
- Plenty of antioxidants from foods and drinks
- Antioxidant-rich foods include broccoli, leafy greens, beans, kiwi, dark chocolate, avocados, artichokes and more
In addition, follow any dietary recommendations you have for other health conditions, such as diabetes. Poorly controlled chronic conditions can increase your risk for oral health problems. If you suspect you have a deficiency in certain vitamins, this can be treated using a supplement after speaking with a health care professional or dietitian. Certain vitamin deficiencies, including a diet too low in vitamin C, can put you at risk for bone loss, tooth decay, gum irritation and other oral health problems.
-
Use a natural gum rub or gel
Many natural remedies may help fight the bacteria and inflammation that lead to gingivitis and periodontitis. If you are interested in applying a paste or gel to the gums to potentially fight plaque, you can consider this list of natural gingivitis therapies studied in at least preliminary human research trials:
- Clove rub
- Turmeric gel
- Aloe vera gel (or juice rinse)
- Neem gel
- Black cumin gel
-
Remove lifestyle risk factors
The way you live your life can impact your physical well-being. Avoid these top lifestyle-related aggravators of oral health problems. Doing so could potentially help boost your body’s ability to fight oral disease.
- Don’t smoke. Quit smoking if you already do. Smoking is one of the key avoidable risk factors for gum disease and tooth loss. Quitting can make it easier for you to heal. (16)
- Reduce stress. Chronic stress in particular can aggravate periodontitis. (17) It may contribute to the destruction of the ligaments and bone. (18) Get stress under control by exercising, talking with a support person or therapist, making time for activities or hobbies you enjoy, exploring your spirituality, using aromatherapy, listening to relaxing music, or looking for the sources of stress in your life and thinking of ways to address them.
- Manage your comorbid conditions. For example, people with diabetes suffer from a two-way street of potential health problems. Diabetes can make gum disease worse and gum disease can worsen diabetes. (19) Several other general health conditions can have similar back-and-forth relationships with periodontitis. Get your overall health under control by following the advice of a health professional as well as managing your oral health aggressively.
How to Prevent Periodontitis
Preventing periodontitis is usually as simple as brushing and flossing your teeth correctly each day. This helps remove bacteria, food and plaque that could otherwise build up and cause problems.
You should also visit your dentist at least once a year (more if you have risk factors for periodontitis). Your dentist can help show you the best ways to brush and can provide an extra level of plaque and tartar removal. Keeping buildup from continuing or spreading helps prevent periodontitis, even if you already have gingivitis.
Precautions
- In severe cases, periodontitis bacteria can spread into the blood and cause problems in the lungs and heart. The infection can also lead to a periodontal abscess. Do not delay treatment for periodontitis or gingivitis if you suspect you have the condition.
- Speak with your dentist and physician about any natural remedies you plan to use for periodontitis. Some herbs, supplements and home remedies can interact with medication or cause problems for people with certain health conditions.
- If you have severe pain, bleeding gums, very bad breath or other periodontitis symptoms, seek care promptly from a dentist for professional diagnosis. Do not attempt periodontitis treatment at home unless you have already been checked by a dentist. Many health problems can be connected to poor dental health.
- Do not swallow mouthwash, oil, rubs, gels, toothpaste or anything else used for oral hygiene unless your dentist tells you to do so.
Conclusion
- Periodontitis is inflammation or infection of the support structures of your teeth. It develops when inflamed or infected gums (gingivitis) go untreated and the infection spreads to the ligaments or bone that hold your teeth in place.
- The condition is very common and is preventable with good oral hygiene, regular dental visits and by taking care of your overall health.
- When treated, most cases of periodontitis improve within a few weeks. If left untreated, the condition can cause tooth loss, pain and severe infection.
- Treatment usually involves deep cleaning under the gums by a periodontics specialist. In some cases, root planing (scraping and reshaping of the tooth roots and bone) may be done to keep the harmful plaque from coming back as easily. Severe cases may require surgery.
5 Natural Remedies to Help Fight the Plaque Causing Infection, Bad Breath and the Overall Health Situation Leading to Periodontitis
- Stepping up your oral hygiene routine
- Using a natural antimicrobial mouthwash
- Revamping your diet
- Using a natural gum rub or gel
- Removing lifestyle risk factors










