This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Staph Infection Symptoms, Causes & Natural Treatments
December 5, 2022
Staph infections account for a large percentage of all hospital visits related to infections each year. The name of the bacteria responsible for causing many a staph infection is staphylococcus, which is actually very common and lives on the skin of approximately 30 percent of even the healthy human population. That means there’s a good chance that staph bacteria is living on your skin from virtually your head to toes, possibly even residing within your mouth and nostrils.
Staph bacteria don’t normally have the chance to proliferate, however, or cause negative reactions, thanks to protection from the immune system.
When they do occur, staph infections can take many forms, ranging in symptoms and severity depending on what part of the body they affect and the strength of someone’s overall immune system. The National Institute of Health has found that most staph germs are spread through skin-to-skin contact, and yes, they’re usually contagious in nature.
One finding that scares many experts who study bacterial infections is that more and more antibiotic-resistant staph bacteria are now being discovered. This means that certain blood-borne infections caused by resistant staph can’t be treated with a normal course of antibiotics or other medications and therefore pose serious risks due to this antibiotic resistance.
According to the Centers for Disease Control and Prevention, methicillin-resistant Staphylococcus aureus (MRSA) is the most common form of resistant staph bacteria that’s immune to many antibiotics. As you can see, because antibiotics are not always a reliable treatment option for infections, preventing infections from developing in the first place by increasing immunity, avoiding contaminated products and practicing good hygiene is your best form of protection against staph infection.
What Is a Staph Infection?
Staph infections are bacterial infections that can result in problems ranging from minor skin reactions all the way to serious, life-threatening heart complications. Experiencing skin rashes or symptoms of food poisoning — such as blistering, vomiting and dizziness — are two of the most common ways that a staph infection presents itself.
These staph infections result from staph bacteria making their way into the pores through punctured skin or to the gastrointestinal tract from contaminated food.
Staph infections caused by Staphylococcus bacteria only become a problem when they spread to deeper parts of the body where they normally aren’t found and then proliferate to high levels. Sometimes bacteria can reach the bloodstream, where they travel to connective tissue, joints, bones and vital organs, like the lungs or heart.
Because there are various body parts they can affect and conditions that can be caused by staph infections, symptoms and signs are different from person to person. While people staying in the hospital or recovering from surgery are usually the most susceptible to developing staph infections, those who seem otherwise healthy are still at risk.
The skin is one of the most frequent body parts to show signs staph of infection in patients who are overall healthy.
Wondering if staph infections are contagious? It’s been found that some staph bacteria can be spread from person to person or carried on contaminated foods, linens and surfaces. This includes the resistant bacteria called MRSA.
MRSA has been shown to be transmitted through bed linens, bed rails, bathroom fixtures, hospital and kitchen equipment, and surgical/medical tools — plus found on sick patients’ and doctors’ hands, in their homes and on their clothing.
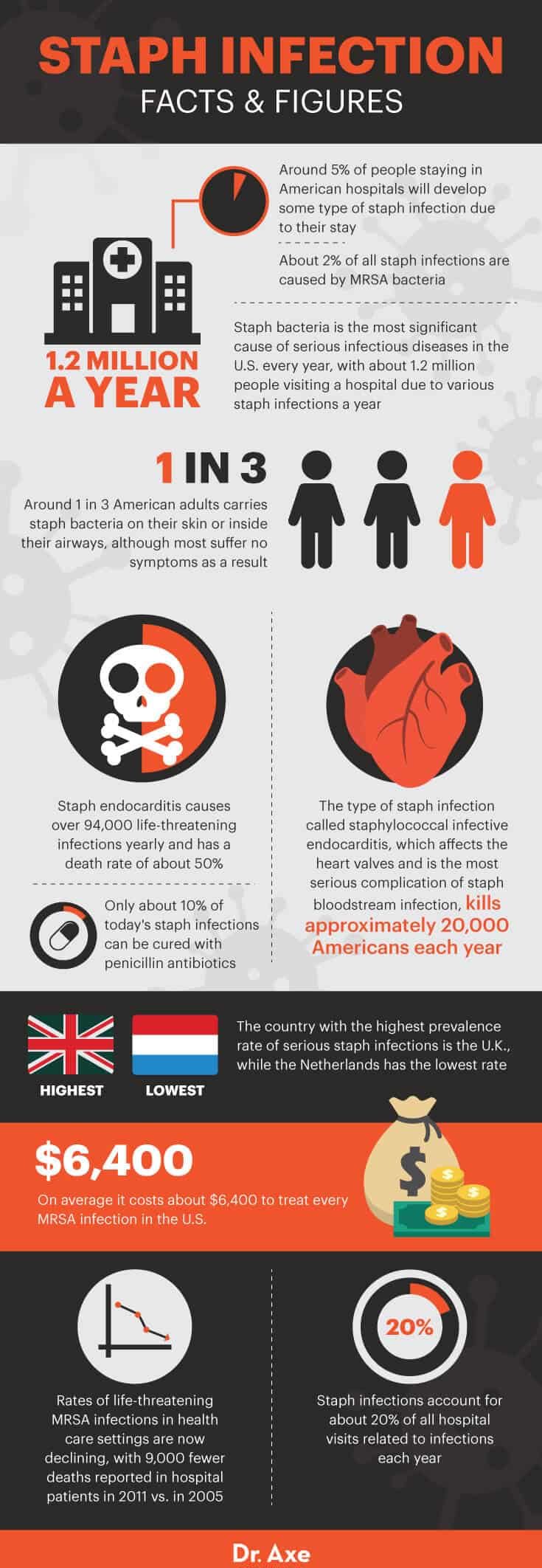
Here are more facts and figures on this condition:
- Staph bacteria is the most significant cause of serious infectious diseases in the United States every year. Every year about 1.2 million people visit a hospital due to various staph infections.
- Around one in three American adults carries staph bacteria on the skin or inside the airways, although most suffer no symptoms as a result.
- The type of staph infection called staphylococcal infective endocarditis, which affects the heart valves and is the most serious complication of staph bloodstream infection, kills approximately 20,000 Americans each year.
- About 2 percent of all staph infections are caused by MRSA bacteria.
- On average, it costs about $6,400 to treat every MRSA infection in the U.S.
Staph Infection Symptoms
Some of the most common staph infection symptoms that affect the skin can include:
- Developing an abscess that causes redness, swelling and pain. This can be in the form of a visible boil, infected hair follicle (which looks like an ingrown hair) or a bump that look like a cystic acne pimple. Many who develop a staph infection of the skin form of a visible swollen pocket that contains pus and feels tender when touched.
- Forming a painful rash. Several types of rashes can be caused by staph infections. One is called impetigo, which is a skin rash that’s contagious and causes large blisters to form. Blisters can sometimes form crust coatings or open up and release fluid. Another is called cellulitis, which is caused from an infection deeper beneath the skin’s surface. Cellulitis occurs most often on the legs or feet and can cause patches of visible ulcers that eventually ooze open.
- In infants or babies, a type of staph infection called staphylococcal scalded skin syndrome can cause a rash or blisters that open up and expose raw skin. Some also develop symptoms of a fever at the same time.
Bacteremia develops when staph bacteria reach the bloodstream. This can cause staph infection symptoms that affect digestion and the vital organs, including:
- Symptoms of food poisoning, such as nausea and vomiting, diarrhea, dehydration, and dizziness
- Low blood pressure and feeling shaky
- Symptoms of a fever, such as having the chills, loss of appetite, shakiness, upset stomach or weakness
- High fevers can result from staph infections called toxic shock syndrome, which can cause toxicity, rashes, confusion, muscle pains and digestive upset
- Septic arthritis symptoms can also form, and this type of infection causes swelling and pain in the joints, especially the knees. Septic arthritis can also cause pain and inflammation in the spine, feet, ankles, hips, wrists, hands, elbows and shoulders.
- One of the most serious conditions caused by a staph infection is endocarditis, which affects the endocardium (the inner lining of the heart). It’s been found that between 10 percent to 20 percent of people who undergo surgery to implant an artificial heart valve develop endocarditis within 60 days. This can affect blood flow and sometimes cause symptoms like damage to the lungs, congestive heart failure or kidney problems.

Causes
Although many of us carry staph bacteria on our bodies, the skin and immune system usually protect us from infection by acting like natural barriers and regulators of bacterium. However, when you consume contaminated food, undergo surgery or get cut, for example, it’s possible for staph bacteria to enter into the body, make their way through the bloodstream and reproduce to high levels.
Staph bacteria can proliferate inside closed-off parts of the body, forming abscesses, allowing pus to accumulate, along with redness, heat, swelling and usually some pain. Staph bacteria are especially harmful when they enter parts of the body that are normally blocked from their presence, cut off from air flow and have poor circulation.
As staph bacteria continue to reproduce inside the affected area, the immune system responds by raising inflammation in order to attack the infection. Inflammation caused from a patient’s own immune system is part of what leads to destructive staph infection symptoms.
Toxins released from staph bacteria can cause an excessive immune response that attacks the body’s own healthy tissue. For example, with endocarditis infections, inflammation causes capillary leakage, low blood pressure, shock, fever, destruction of the heart valves and sometimes strokes.
Risk factors for developing a staph infection include:
- Staying in a hospital or nursing home where bacteria can spread from patient to patient. People in the hospital are mostly likely to get an MRSA infection, especially if they already have a run-down immune system due to having another health problem or taking antibiotics.
- Being sick with another infection, autoimmune disorder or condition that causes low immunity.
- Spending lots of time in public settings where you might be around other sick children or adults, including daycare centers, schools or universities.
- Undergoing surgery, especially to implant an artificial device, joint, stent or pacemaker. Bacteria can sometimes accumulate around these foreign objects in the body or enter the bloodstream through surgical incisions.
- Having wounds, stitches, incisions or cuts that are left uncleaned and untreated.
- Using expired or contaminated tampons and feminine products or not changing them often enough.
- Consuming foods that are more likely to be contaminated with bacteria that cause food poisoning. These foods include pork products, old vegetables or fruits that have been left out, and unrefrigerated meat or dairy products.
- Not washing your hands regularly after using public bathrooms, going to a health facility/gym, or sharing equipment that can carry sweat, blood or other fluids along with bacteria.
- Having low immune function due to a poor diet, nutrient deficiencies, allergies and an unhealthy lifestyle.
Treatment and Prevention
Diagnosis of staph infection or poisoning in an individual is usually based on observing signs and symptoms. Sometimes blood, stool or urine tests are also used to confirm diagnoses.
The conventional way of treating staph infections is usually:
- Opening up the affected area up in order to reduce inflammation and drain out excess blood or dead cells (which form pus)
- Prescribing antibiotics
In many cases, abscesses caused from staph infections can be closed off from drainage and therefore cause pain and swelling. This can happen when cellular debris and pus are left behind by the immune system but have nowhere to go (much like an infected pimple that’s beneath the surface of the skin and doesn’t form a noticeable white head). In this case, doctors might open up the abscess, blister, ulcer, etc., in order to relieve fluid from the infection.
Antibiotics, such as cephalosporins, nafcillin, sulfa drugs or vancomycin, are commonly used to fight staph bacteria, however some strains of bacteria have now become resistant to these medications. MRSA is the most widespread type of staph that is antibiotic-resistant and causes serious infections in thousands of patients each year.
Although researchers continue to explore ways to treat MRSA infections with new types of antibiotics, some patients don’t respond and wind up needing surgery to remove MRSA abscesses.
There are natural treatment options as well to help with symptoms and prevention, including:
1. Strengthen Your Immune System
Avoid inflammatory and allergenic foods that disturb gut health and lower immune function, including packaged, processed foods; potential food allergens like conventional dairy, gluten, shrimp and peanuts; refined fats or fried foods; and added sugar.
Consider taking herbs and supplements to boost immune function, such as zinc; antioxidants like vitamin C, echinacea and vitamin D; and antiviral herbs for immunity like calendula, elderberry and astragalus. In addition, fill up on healing foods like fresh fruits and veggies, probiotic foods, bone broth, and healthy fats like coconut, nuts and seeds.
2. Practice Good Hygiene and Hand-Washing
Regularly wash all fabrics and linens (especially when they’re shared) using a natural antibacterial detergent. Ideally look for detergents containing essential oils that have antibacterial/antimicrobial properties, or make a homemade laundry soap yourself.
Be sure to wash all dirty clothes containing bodily fluids, towels and bedding, particularly after they come into contact with someone who has an infection.
Clean and disinfect all working surfaces thoroughly and regularly, including those in bathrooms and kitchens. Public surfaces that are used or touched daily carry the biggest risk for spreading staph bacteria, including doorknobs, phones, or surfaces in public restrooms and locker rooms.
Frequently disinfect shared items in your home or workplace using natural cleaning products, especially those regularly used with someone’s hands, such as phones, doorknobs, keys, cabinet handles and keyboards. Run any shared utensils and kitchen or cooking equipment through a dishwasher after use.
Food workers should always wash their hands thoroughly to prevent foodborne illnesses from spreading.
Avoid sharing personal items, such as towels or razors, that can carry bodily fluids.
If you go to a gym or exercise facility, make sure to clean equipment after use, and shower once you leave. Try using a towel when putting your bare skin on any surface, such as a protective layer between you and mats or the gym floor. Wash your hands after lifting weights, touching machines or using the bathroom.
Employees who are sick or suffering from infections should avoid going to work, and children who are sick should stay home from school. In public settings where shared equipment is used, such as tools, computers, phones, uniforms, helmets and protective gear, all equipment should be regularly disinfected.
3. Clean and Protect All Open Cuts
Be sure to keep any cuts, incisions or wounds clean and covered using band-aids, bandages or another dressings. Use a natural antibacterial wash over skin when showering, and make sure to protect openings in the skin when in high-risk settings like hospitals or nursing homes.
Be sure to let your doctor know right away if a cut shows signs of infection, including redness, swelling and oozing, since this can help prevent the infection from worsening.
4. Properly Store and Handle Food
Staphylococcal food poisoning is caused from staph bacteria entering the gastrointestinal tract after eating foods that are contaminated with toxins left behind from staph microbes. Staphylococcus aureus is most likely to affect food workers who can come into contact with staph bacteria when touching contaminated products or who pick up bacteria from employees or when working on dirty surfaces.
In most patients, symptoms like severe nausea and vomiting begin quickly after staph enters the digestive system, usually within two to eight hours. To prevent staph food poisoning from spreading, employees in restaurants, grocery stores, butchers, etc., should always thoroughly wash their hands after touching food or after going to the bathroom, stay home when they’re sick, and refrigerate food properly.
Foods that have a higher risk for spreading staph bacteria include raw foods prepared with someone’s bare hands, unpasteurized milk and cheese products (especially when they sit out for long periods), salty pork products, processed meats, puddings or custards, and any food that’s prepared using contaminated equipment.
Will cooking food remove staph bacteria? Unfortunately, the CDC reports that toxins created in food by staph bacteria cannot usually be killed from cooking or heating food. This is why it’s still possible to get food poisoning from any type of prepared meal.
Fortunately, food poisoning symptoms should go away within one to two days in most cases.
Food poisoning staph symptoms don’t respond to taking antibiotics, so unless you’re becoming very weak or dizzy, you don’t usually need to visit a doctor office.
In the case of food poisoning symptoms, to prevent symptoms of dehydration due to vomiting or diarrhea, try to consume fluids (such as coconut water or freshly made fruit/veggie juice for electrolytes), stay in a cool environment and get plenty of rest. If staph food poisoning affects infants, children or the elderly, it’s recommended you head to the doctor right away.
5. Treat Skin Rashes and Blisters
To help reduce pain from blisters or lower skin swelling due to a staph rash:
- Press a warm compress against the rash once or twice daily using a fresh, clean washcloth or towel. You can also take warm showers (but not too hot) or baths to reduce swelling and tenderness.
- Elevate painful or swollen areas to prevent too much fluid accumulation.
- Very gently stretch stiff areas to keep them from getting even more stiff.
- Wear loose, breathable clothing.
- Avoid other skin irritants as much as possible while you heal, including scented body soaps, detergents, shampoos, perfumes and lotions.
- Speak to your doctor about applying a soothing essential oil, such as lavender, to the skin, combined with a carrier oil, such as coconut oil, several times daily.
Precautions
Because these infections can be serious and contagious, always consult with your doctor if you suspect you might have signs of have a staph infection. This is especially important in infants or children, the elderly, following surgery, or if you have another health condition that affects your immune system.
Seek professional help if symptoms worsen and don’t go away within one week, or if they appear suddenly and cause very high fevers or swelling.
Conclusion
- Staph infections are caused by a common bacteria called Staphylococcus. Some staph bacteria, including MRSA, are resistant to antibiotic treatments and therefore the biggest risk to public health.
- Symptoms of a staph infection can affect the skin, GI tract, heart, blood vessels, joints, lungs and bones. Some of the most common staph infection signs are food poisoning, skin rashes, forming blisters that ooze open, joint pain and fevers.
- Prevention and natural treatments for staph infections include boosting immunity with a healthy diet, washing your hands, cleaning and disinfecting your home/work environment regularly, reducing fevers naturally, and treating skin pain with heat and essential oils.