This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Reduce Your Risk of Pelvic Inflammatory Disease (PID)
October 24, 2017
Pelvic inflammatory disease (or PID), a type of bacterial infection that affects some women’s reproductive systems, is capable of causing damage to any part of the female genital tract. One unfortunate complication due to PID that some women experience is infertility (the inability to get pregnant). About 1 in 8 women with a history of PID will have trouble getting pregnant. Others who do become pregnant are at a higher risk for pregnancy-related complications. (1)
What is the most common cause for pelvic inflammatory disease? Experts believe that untreated sexually transmitted diseases, especially gonorrhea and chlamydia, are the number one reason why women develop PID. However some women develop PID even from “normal” common infections such as bacterial vaginosis.
Signs of pelvic inflammatory disease include pelvic pain, painful sex, fever and bleeding between periods. The good news is that like other STDs, pelvic inflammatory disease is usually preventable. Infections that are not sexually transmitted can sometimes cause PID. But there are ways to lower your risk for these types of infections too. Steps you can take to greatly reduce your odds of developing a pelvic infection, and dealing with associated consequences of PID, include practicing sex safe, treating STDs as soon as possible, and increasing your protection against infections by protecting the healthy flora that populate the genital tract.
What Is Pelvic Inflammatory Disease?
The definition of PID is “inflammation of the female reproductive tract (such as the fallopian tubes and ovaries) that occurs especially as a result of a sexually transmitted disease and is a leading cause of infertility in women.” (2)
One of the reasons it’s so important to treat pelvic inflammatory disease as soon as possible is because of its tendency to spread and worsen. PID infection can spread from the vagina to other parts of the genital tract, including the cervix, uterus, fallopian tubes and ovaries. Sometimes symptoms due to PID will not be obvious at all. But other times pain, scarring and permanent damage can develop.
Not only does untreated PID increase the risk for infertility, but in some cases it can also cause other problems like ectopic pregnancies. Ectopic pregnancies occur when one of the ovaries releases an egg that becomes fertilized but cannot travel properly to the uterus/endometrium due to scarring in the fallopian tubes.
Signs & Symptoms of Pelvic Inflammatory Disease
Symptoms of pelvic inflammatory disease vary from person to person. In some cases no symptoms are experienced at all. Other times they might be only mild, and for some women symptoms can be very painful and severe. It’s not uncommon for a woman with PID to be completely unaware of the problem, due to how symptoms are commonly barely noticeable or confused with other health problems. Some women only find out they have PID years down the road once they have difficulty trying to get pregnant.
Some of the most common pelvic inflammatory disease symptoms include: (3)
- Lower abdominal pain, which can be felt on only one side or both sides.
- Tenderness and sensitivity around the genital area.
- Painful sex, sometimes which leads to bleed during or after intercourse.
- Irregular periods.
- Abnormal vaginal discharge, including discharge that appears yellow or green (a sign of infection).
- Burning sensations when urinating.
- Pain during bowel movements.
- Fever symptoms like nausea, chills, loss of appetite, weakness and fatigue.
Complications Caused By Pelvic Inflammatory Disease:
A number of serious complications have been linked to pelvic inflammatory disorder. As mentioned above, PID can also cause infertility (inability to get pregnant) and ectopic pregnancies, which are pregnancies that occur outside the womb (uterus). The longer, or more times, you’ve had PID, the higher risk you have of dealing with infertility. When an ectopic pregnancy occurs, the symptoms can be very similar to those associated with pelvic inflammatory disease, although usually they are more intense. An ectopic pregnancy is a very serious problem that can be life-threatening. So it requires urgent care to prevent bleeding and other complications.
Other complications associated with untreated PID are:
- Scar tissue forming on the inside or outside of the fallopian tubes. Damage can sometimes be irreversible, but usually this only occurs if the disease was left untreated for a long time. Infected fluid may also form abscesses in the fallopian tubes.
- Scar tissue causing a tubal blockage, which prevents an egg from traveling down a woman’s tubes normally.
- Long-term pelvic/abdominal pain that can make sex painful and unenjoyable.
- Higher risk for pregnancy and birth-related complications.
Because PID is most commonly caused by an untreated sexually transmitted disease (STD), it’s important to be aware of the symptoms of STDs like gonorrhea and chlamydia. Chlamydia is a common type of STD that affects both men and women and is transmitted through vaginal, anal or oral sex. Research shows that most people who have these types of STDs are not aware of it. And many are under the age of 25 and may be too embarrassed to seek help. (4) It’s common for chlamydia to not cause any noticeable symptoms. But this doesn’t protect the reproductive system from scarring and more serious infections.
STDS that can cause PID have similar signs and symptoms to PID itself. When someone does have noticeable symptoms they can include: (5)
- Abnormal vaginal discharge, which sometimes has a fishy vaginal odor.
- Burning sensations when urinating or having bowel movements.
- Discharge from the penis, along with burning sensations.
- Pain and swelling in one or both testicles.
- In some cases rectal pain, bleeding and discharge.
Pelvic Inflammatory Disease Causes & Risk Factors
Pelvic inflammatory disease most commonly affects women of reproductive age who are under the age of 35. Untreated sexually transmitted diseases, especially gonorrhea and chlamydia, are by far the most common cause of PID. But many different types of bacteria can contribute to PID, some of which may proliferate inside a woman’s reproductive system following intercourse (even if no STD was transmitted) or after pregnancy, childbirth, miscarriage, or an abortion.
Some of the bacteria that have been found to cause pelvic inflammatory disease include: (6)
- Chlamydia trachomatis — Currently considered the most significant pathogen associated with PID, since about 8–10 of women with C. trachomatis infection will develop PID if not treated. Chlamydia has also been detected in up to 60 percent of women with infertility/reproductive problems including salpingitis or endometritis.
- Neisseria gonorrheae
- Mycoplasma genitalium
- And bacterial vaginosis-associated microorganisms, especially anaerobes.
Although it’s rare, even “ordinary” bacterial infections like vaginosis can progress to PID. Bacterial vaginosis (or BV) is a common type of vaginal infection caused by an overgrowth of normal microbes (bacteria) inside the vagina that affects almost 30 percent of the female population between the ages of 15–49 in the U.S. (and other industrialized nations). (7)
Risk factors that are associated with a higher chance of developing pelvic inflammatory disease include:
- Being a woman between the ages of 25–35.
- Having unprotected sex.
- A history of PID and other types of vaginal bacterial infections.
- Having more than one sexual partner, which increases the risk for all types of STDs. This is especially risky when you have a sex partner who has many other sex partners.
- Frequently douching, which can alter the delicate balance of flora (protective bacteria) found inside the vagina.
- Using an intrauterine device (IUD) as a method of birth control, especially within the first three weeks after the IUD is inserted.
- Having a history of vaginosis, frequent UTIs, or other types of vaginal infections due to things like pregnancy, childbirth, miscarriage or an abortion.
- Smoking and illicit drug use.
Conventional Treatments for Pelvic Inflammatory Disease
Studies indicate that in the United States alone there are at least an estimated 1.2 million medical visits each year related to PID. (8) Pelvic inflammatory disease commonly is treated with one or more prescription antibiotics, which help to clear the infection. Antibiotics that are used to treat mild-to-moderate cases of PID can include:
- Extended spectrum cephalosporin, commonly in conjunction with doxycycline or azithromycin.
- Cefotetan.
- Clindamycin.
- Gentamicin, followed by doxycycline.
- Ampicillin/Sulbactam.
- Other broad-spectrum antibiotics that fight off polymicrobial flora associated with vaginosis (called aerobes and anaerobes).
- Most women being treated for PID won’t require a hospital stay or any time of intensive care; however, women who are at a greater risk for complications sometimes will. If a woman is pregnant, does not get better after taking medications, has a high level of inflammation in the fallopian tubes, or becomes very ill, then she may need to stay in the hospital in order to be monitored and and receive intravenous antibiotics.
- In rare and severe cases, surgery might be needed to remove scarring, damaged tissue or abscesses that may rupture within the genital tract.
PID is considered a type of sexually transmitted disease, which means that male or female sexual partners of women with PID should also visit a doctor for treatment. It’s important that both partners finish their treatment protocol before having any kind of sex. This way they don’t wind up re-infecting each other. Both partners will need to be treated whether they have symptoms or not.
Sometimes symptoms of an infection will go away before the infection is totally cleared. But you and your partner should still take the full dose of medications prescribed to you regardless of whether you’re feeling better or not.
Be aware that while PID is usually treatable, it can still return at a later time. In fact if you have had PID before, you have a higher chance of developing it a second time. Becoming infected with an STD again can cause the infection to re-spread. This is why safe sex is important for prevention long-term.
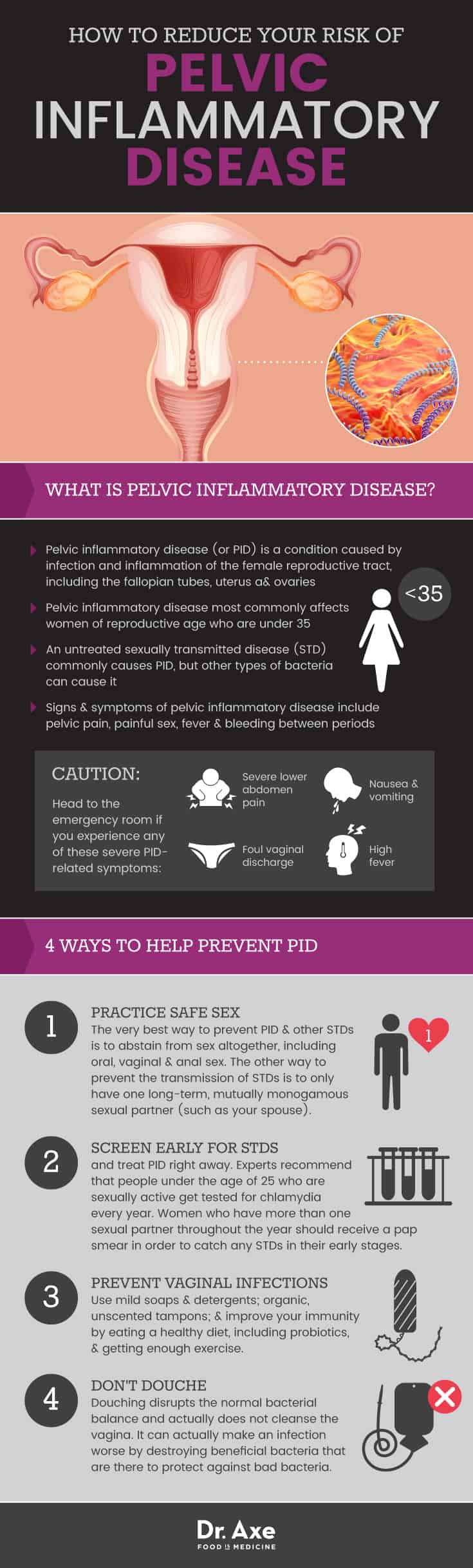
4 Natural Ways to Help Prevent Pelvic Inflammatory Disease
- Practice safe sex.
- Screen early for STDs and treat PID right away.
- Prevent vaginal infections by using mild hygiene products, probiotics and boosting your immunity.
- Don’t douche.
1. Practice Safe Sex
The very best way to prevent PID and other STDs is to abstain from sex altogether, including oral, vaginal and anal sex. The other way to prevent the transmission of STDs is to only have one long-term, mutually monogamous sexual partner (such as your spouse). If you do choose to have sex with multiple partners, then be sure to wear a condom every time. Even if you are in a monogamous relationship, if you and your partner are being treated for PID, then abstain from sex until you’re both fully recovered.
2. Screen Early for STDs & Treat PID Right Away
Experts recommend that people under the age of 25 who are sexually active get tested for chlamydia every year. Women who have more than one sexual partner throughout the year should visit a gynecologist for a pap smear in order to catch any STDs in their early stages. If you are diagnosed with an STD or PID, then getting treated right away lowers your risk for developing long-term complications. In other words, the longer you wait to get tested and treated for STDs, the more likely it is that you develop permanent damage to your reproductive system.
Pregnant and nursing women need to be especially cautious about being treated early. STDs, and even vaginosis, can lead to complications in a developing fetus. If you’re breast-feeding, talk to your doctor as well, since this will have an impact on the medication/treatments that are safe for you to use to clear the infection.
3. Prevent Vaginosis & Other Common Infections
Vaginosis usually will not lead to complications like PID, but it is possible. Keep in mind that if you’ve had vaginosis in the past, it’s common for the infection to reoccur within three to 12 months. Some of the ways you can help prevent infections from developing or recurring include:
- Using mild soap and detergent — Washing the vagina with commercial (usually alkaline) soaps can cause skin irritation, imbalances in pH and microflora, and increased vaginal discharge. Try to avoid using any feminine deodorant sprays, perfumed or dyed products near your vagina (such as lubricants or scented tampons/pads), especially on the inside or if you already have any type of irritation. Try not to wash your underwear in any strong detergents with perfumes and other chemicals that can rub off onto your skin. A safer option, especially if you’re sensitive, is to use an unscented glycerin or castile soap, and to not over-wash or internally cleanse your vagina, which is naturally self-cleaning.
- Upgrade your tampons — If you’re using tampons during your period, then stick with unscented, ideally organic, tampons or pads that don’t contain any harsh chemicals, dyes or perfumes. Avoid bacterial overgrowth by changing tampons at least three times daily (at least every 6–8 hours).
- Boost your overall immunity — Having a strong immune system won’t protect you from acquiring an STD. But it may help to prevent recurring infections like vaginosis and decrease risk for complications. Some of the ways you can protect against infections include: eating a healthy diet; taking probiotics and eating probiotic foods (probiotics including lactobacillus increase the number of “good bacteria” in the vagina and re-establish a balanced microflora); addressing allergies, nutrient deficiencies, diabetes and digestive problems; exercising, sleeping enough and avoiding medications that may contribute to infections.
4. Don’t Douche
Because douching disrupts the normal bacterial balance inside the vagina, it’s a risk factor for developing infections. (9) Some women might think that douching will help to get rid of an infection that’s already forming, or help reduce symptoms caused by an STD. But this is not true. Douching does not actually help to cleanse the vagina. And it can actually make an infection worse by removing beneficial bacteria that are there to protect against harmful bacteria.
Precautions When Treating Pelvic Inflammatory Disease
If you experience any of the signs and symptoms of an STD mentioned above (abdominal pains, painful sex, burning when peeing, irregular periods, etc.) then head to your doctor for an examination as soon as you can. Your partner should also be examined by a doctor, or you should let any recent partners know about your diagnosis. You should head to the emergency room if you experience any of these severe PID-related symptoms: severe pain in your lower abdomen, nausea and vomiting, high fever (temps above 101 F or 38.3 C) and foul vaginal discharge.
Key Points
- Pelvic inflammatory disease (or PID) is a condition caused by infection and inflammation of the female reproductive tract, including the fallopian tubes, uterus and ovaries.
- An untreated sexually transmitted disease (STD) commonly causes PID, but other types of bacteria can cause it.
- Symptoms of PID, when they do occur, include abdominal pain, painful sex, pain when urinating, irregular periods and infertility.
- Head to the emergency room if you experience any of these severe PID-related symptoms: severe pain in your lower abdomen, nausea and vomiting, high fever (temps above 101 F or 38.3 C) and foul vaginal discharge.
4 Ways to Help Prevent Pelvic Inflammatory Disease
- Practice safe sex.
- Screen early for STDs and treat PID right away.
- Prevent vaginal infections by using hygiene products, probiotics and boosting your immunity.
- Don’t douche.








