This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Interstitial Cystitis: 6 Natural Ways to Help Relieve Bladder Pain
March 14, 2024

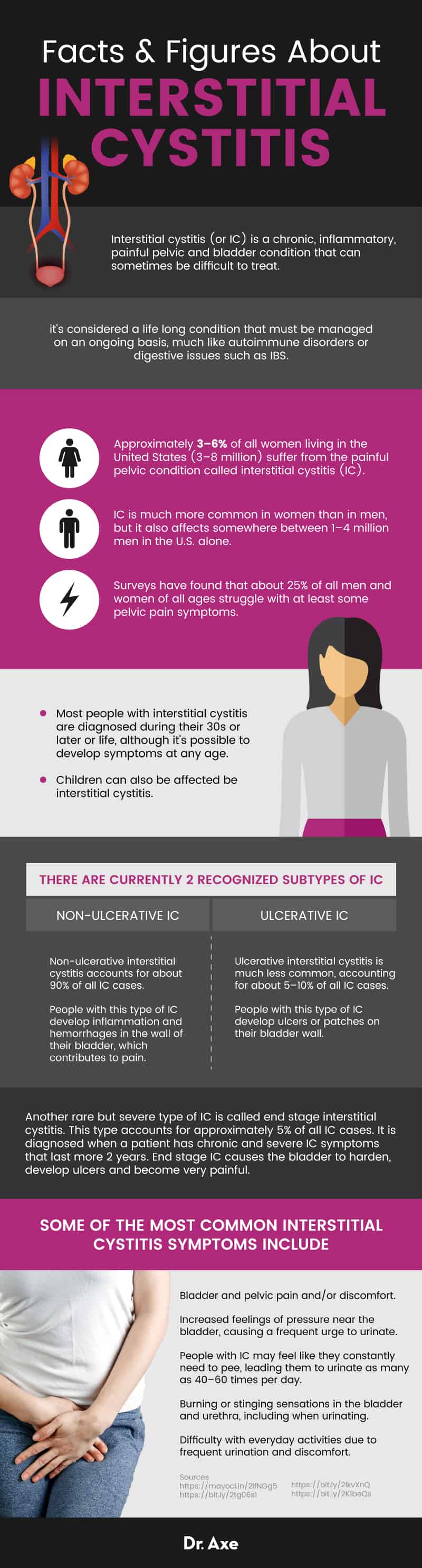
Approximately 3–6 percent of all women (3 to 8 million) living in the United States suffer from the painful pelvic condition called interstitial cystitis (IC). IC is much more common in women than in men, but it also affects somewhere between 1–4 million men in the U.S. alone.
Children can also be affected be interstitial cystitis; in fact, many adult patients with the condition claim that their symptoms have affected them since a young age.
Although IC cannot be completely cured (it’s considered a chronic condition), treatment can help to manage symptoms and reduce pain. What types of interstitial cystitis natural treatments are available? These include acupuncture for improving pain tolerance; exercises like yoga or tai chi to increase blood flow; and a healing diet to reduce inflammation.
Chronic stress and unhealthy habits like smoking can also worsen interstitial cystitis symptoms, so lifestyle changes to address these contributing factors are also important.
What Is Interstitial Cystitis?
Interstitial cystitis (or IC) is a chronic, inflammatory, painful pelvic and bladder condition that can sometimes be difficult to treat. According to the Interstitial Cystitis Association, IC is also referred to by several other names, including painful bladder syndrome (PBS), bladder pain syndrome (BPS) and chronic pelvic pain.
Is interstitial cystitis considered a disability? In some ways, yes. IC is sometimes said to be “debilitating” and can be associated with severe pain and limitations, negatively impacting people’s quality of life. Unfortunately, it’s considered a life long condition that must be managed on an ongoing basis, much like autoimmune disorders or digestive issues such as IBS.
Many people mistake IC for other health conditions, especially urinary tract infections (UTIs). This is because these two conditions share similar symptoms, like bladder and pelvic pain. However, with IC there is no infection present, unlike with UTIs. IC can also be confused with chronic prostatitis in men, which experts believe has led to an under-diagnosis of IC among adult men.
Symptoms
What signs and symptoms would you expect to see with interstitial cystitis and why? IC symptoms can be different for every person who deals with the condition.
What makes IC different from other related conditions is that someone must experience urinary pain that lasts for more than six weeks and that is not associated with health problems like an acute infection or kidney stones. Some people have symptoms nearly all the time, while others experience symptoms that flare up but then go away before returning.
The most common interstitial cystitis symptoms include:
- Bladder and pelvic pain and/or discomfort. Pain can sometimes be very severe and spread to the lower back, urethra and genitals. Pain is sometimes described as feeling like piercing, stabbing or dull aches.
- Increased feelings of pressure near the bladder, causing a frequent urge to urinate. “Urinary frequency and urgency” refers to needing to go to the bathroom more often and feeling a stronger than usual desire to urinate all of a sudden. People with IC may feel like they constantly need to pee, leading them to urinate as many as 40–60 times per day.
- Burning or stinging sensations in the bladder and urethra, including when urinating.
- Pain during intercourse. Women may feel pain in their vulva, vagina or the area behind the vagina. Men can develop pain in their scrotum, testicles, penis or the area behind the scrotum.
- Trouble exercising due to pain.
- Trouble sleeping due to getting up to pee.
- Difficulty with everyday activities due to frequent urination and discomfort.
- Increased emotional stress, anxiety and/or depression.
Causes
IC is an inflammatory condition of the bladder that experts believe is caused by dysfunction of protein membranes found in the bladder lining. There’s evidence that damage to the bladder wall can allow particles in the urine (maybe causing cloudy urine), such as potassium, to leak into the bladder lining causing an inflammatory response. Normally the lining of the bladder should be able to repair itself, but in people with IC this process doesn’t seem to happen.
Studies suggest that proteins, including the type called antiproliferative factor (APF), may interfere with normal activity of bladder cells, causing ongoing damage and irritation. The immune system may start to attack the bladder (an autoimmune response) and nerve signaling in the bladder may also become impaired. When someone with IC’s bladder fills up with urine after being filtered by the kidneys, the stretching sensation causes lots of pressure and discomfort that can sometimes be intolerable.
Based on its underlying causes, is interstitial cystitis a disease? IC is not necessarily a disease, but more of a condition that encompasses a number of uncomfortable symptoms. There are currently two recognized subtypes of IC: non-ulcerative IC and ulcerative IC.
- Non-ulcerative interstitial cystitis accounts for the vast majority, about 90 percent, of all IC cases. People with this type of IC develop inflammation and hemorrhages in the wall of their bladder, which contributes to pain.
- Ulcerative interstitial cystitis is much less common, accounting for about 5 percent to 10 percent of all IC cases. People with this type of IC develop ulcers or patches on their bladder wall.
- Another rare but severe type of IC is called end stage interstitial cystitis. This type accounts for approximately 5 percent of all IC cases. It is diagnosed when a patient has chronic and severe IC symptoms that last more two years. End stage IC causes the bladder to harden, develop ulcers and become very painful.
It’s still not entirely known what causes the all cases of IC. But a number of factors have been identified that seem to contribute to the development of the condition. These include:
- Any health condition or event that damages the bladder or bladder lining. For example, “bladder trauma” may be caused by bladder infections, pelvic infections or pelvic surgery.
- Bladder overdistention, caused by holding urination in for long periods of time.
- Pelvic floor muscle dysfunction
- Autoimmune disorders
- Pelvic inflammatory disease, which can be linked to bacterial infections including sexually transmitted infections like chlamydia.
- Primary neurogenic inflammation (hypersensitivity or inflammation of pelvic nerves)
- Spinal cord trauma
Risk Factors
The IC Association states that “Interstitial cystitis (IC) can affect anyone. Women, men, and children of any age or race can develop IC.” Surveys have found that about 25 percent of all men and women of all ages struggle with at least some pelvic pain symptoms. No differences have been found in prevalence rates based on race and ethnicity.
Most people with interstitial cystitis are diagnosed during their 30s or later or life, although it’s possible to develop symptoms at any age. Lifestyle habits including eating a poor diet, smoking and being very stressed all seem to make IC symptoms worse. Women commonly find that their symptoms get worse just prior to or during menstruation. And there’s some evidence that certain antidepressants, sinus medicines and pain relievers may trigger IC symptoms.
Children and adults who have IC are more likely to have other health conditions too, including fibromyalgia, vulvodynia, allergies, reflux, gastrointestinal problems, enuresis (bedwetting) or incontinence.
Conventional Treatment
How do you test for interstitial cystitis? An interstitial cystitis diagnosis can be determined with tests that include a physical exam, urinalysis and urine culture test, ultrasound and imaging tests.
Conventional treatment options for IC can include a combination of: medications, physical therapy, biofeedback training, bladder training (which involves gradually waiting longer to use the bathroom and stretching out the time between urinating), alternative treatments to control stress, lifestyle changes, and bladder surgery, when needed.
Examples of interstitial cystitis medications that are used to manage symptoms include:
- Amitriptyline
- Pentosan polysulfate
- Hydroxyzine
- Cimetidine
- Gabapentin, used to help reduce side-effects
- Prescription pain killers including opioid analgesics or codeine, or over-the-counter (OTC) pain medications such as aetaminophen, aspirin and ibuprofen.
Because IC is not caused by an infection, antibiotics haven’t been shown to be helpful. Antibiotics should only be used if it’s determined that an infection, such as a UTI, is the root cause of your symptoms.
When is surgery for interstitial cystitis recommended? Surgery is typically a last resort option if other treatments don’t do enough to manage symptoms.
Surgery for IC can involve inserting a small amount of liquid medication (medications used are Heparin, Lignocaine and sodium bicarbonate) into the bladder with a catheter while the patient is under anesthesia. The procedure helps to stretch the bladder lining and positively impact the nerves located in the bladder.
This type of procedure is called badder instillation (or a bladder wash or bath). While it can help to decrease pain, it is usually only a temporary solution. Surgery may need to be repeated every six months or yearly in order to keep painful symptoms from returning. Rarely other surgeries will be needed, including to remove or enlarge the bladder.
How to Manage Interstitial Cystitis Symptoms
1. Avoid These Foods
It’s important to eat an interstitial cystitis diet. Eating inflammatory foods can exacerbate IC symptoms, which is why a healthy diet should be a key part of every interstitial cystitis treatment plan.
One survey found that 85 percent of patients with IC experienced an aggravation of symptoms after eating certain foods or beverages. For example, one study reported that coffee, tea, spicy foods, alcohol and carbonated beverages negatively affected more than 52 percent of IC patients.
Every person with IC reacts to dietary changes a bit differently; some find that changing their diet makes a big difference in terms of reducing symptoms, while others don’t notice much improvement with dietary changes.
If you’re struggling with interstitial cystitis symptoms, it’s recommended that you avoid these foods and drinks which can cause IC “flares”:
- Pizza and other heavy foods made with lots of cheese or dairy
- Sweetened drinks including lemonade, soda and most commercial juices including cranberry or orange juice
- Carbonated and caffeinated beverages such as coffee, teas and sodas
- Processed foods made with refined grains (cereals, breads, wraps, cookies, cakes, etc.)
- Spicy or acidic foods, including tomatoes, hot peppers and citrus fruits
- Common allergens, which can include conventional dairy products, grains containing gluten, peanuts, and shellfish. There hasn’t been a clear relationship established between lactose intolerance or gluten intolerance and IC; however, many people with IC find their symptoms get better when avoiding these foods.
- Foods high in sodium/salt, added sugar or those that contain artificial sweeteners
- Processed foods that contain saturated fat sourced from conventionally raised animals (like beef and cheese)
- Alcohol
2. Eat These Foods
Aim to eat a balanced diet that includes a variety of whole, unprocessed foods that are well-tolerated. Foods to eat that support recovery from interstitial cystitis include:
- Foods high in antioxidants, including leafy green veggies, berries, broccoli, Brussels sprouts, carrots, beets, tomatoes, bell peppers, green tea, cocoa, sea vegetables, etc.
- High-fiber foods, like avocados, berries, apples, pears, coconut flakes, figs, artichokes, winter or acorn squash, sweet potatoes, beans and legumes, seeds and nuts like almonds, walnuts, flax seeds and chia seeds
- Fresh herbs and spices like turmeric, ginger, basil, parsley or oregano, plus raw garlic and raw honey
- Organic, grass-fed or pasture-raised meats
- Wild-caught fish like salmon, mackerel, sardines or herring
- 100 percent whole grains like quinoa, brown rice, buckwheat and rolled oats
- Bone broth or protein powder made from bone broth/collagen
You should drink enough water each day to prevent dehydration; however, you don’t want to drink more than you need because this will contribute to urinary frequency.
Another advantage of eating a healthy, high-fiber diet like the one described above is that it helps prevent constipation and facilitates having regular bowel movements each day. People with IC have reported that having regular bowel movements helps manage their symptoms because it decreases pressure and bloating in the abdomen.
3. Manage Stress with Relaxation Techniques
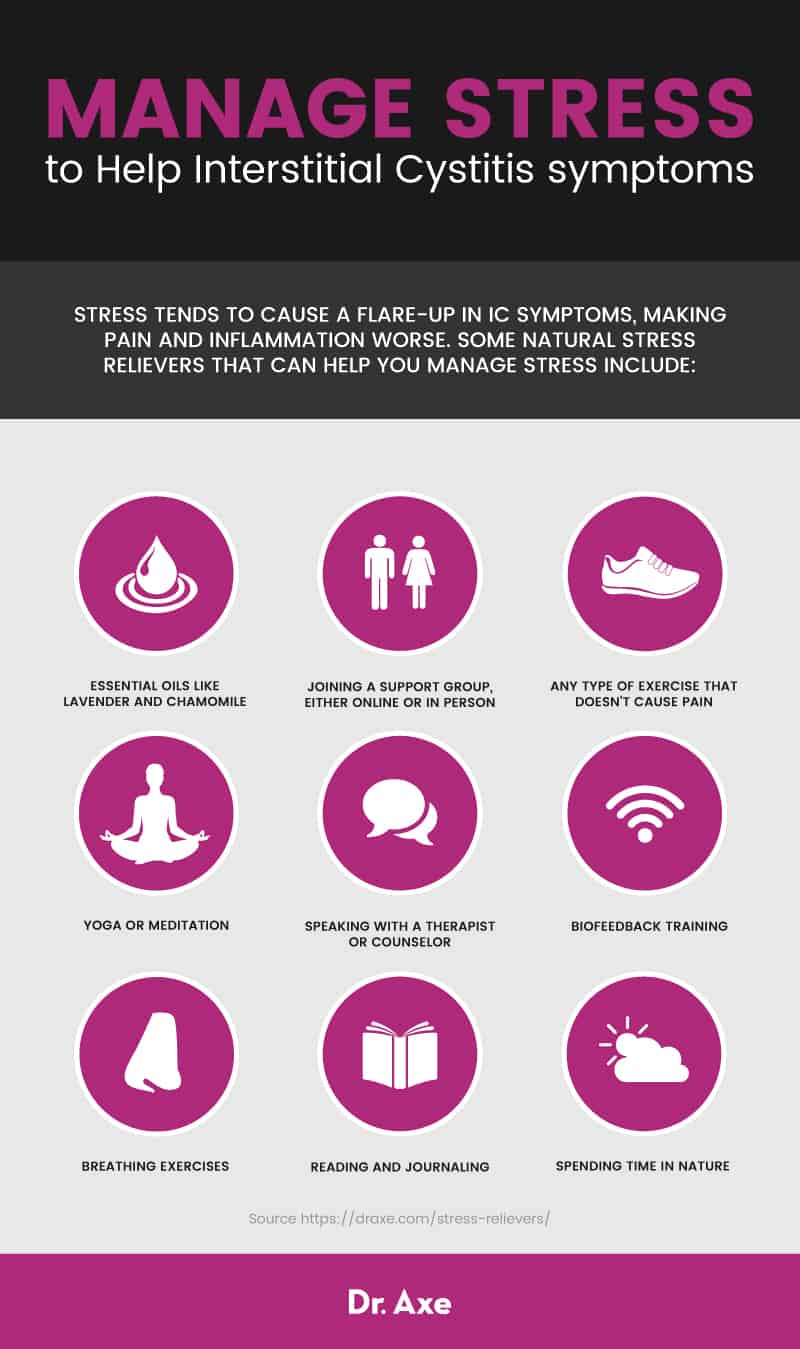
Stress tends to cause a flare-up in interstitial cystitis symptoms, making pain and inflammation worse. Some natural stress relievers that can help you manage stress include:
- Yoga
- Meditation
- Breathing exercises
- Biofeedback training
- Using essential oils like lavender and chamomile
- Spending time in nature
- Reading and journaling
- Any type of exercise that doesn’t cause pain
- Speaking with a therapist or counselor
- Joining a support group, either online or in person
4. Acupuncture & Mind-Body Approaches to Cope With Pain
Complementary and alternative medicine (CAM) approaches are now being widely used to help patients cope with chronic pain, terminal illnesses and other health challenges. CAM treatments include:
- Dietary modification
- Herbs and supplements
- Bladder training
- Biofeedback
- Yoga
- Massage therapy
- Physical therapy
- Qigong
- Traditional Chinese Medicine
- Acupuncture
While more randomized, controlled trials are still needed to confirm how these approaches can help people with IC, a study published in the journal Translational Andrology and Urology states that “Clinical evidence has shown that each therapy can certainly benefit a portion of IC/BPS patients.”
CAM treatments are already popular among people with IC. According to one survey based on 1,982 IC/BPS patients, approximately 84 percent had tried CAM treatments and 55 percent were recommended to use CAM by their physicians. Studies have found that acupuncture can be helpful for dealing with chronic pain, stress and emotional problems like anxiety or depression. Certain studies have also shown that acupuncture can help modulate bladder storage and emptying functions.
“Manipulative, body-based approaches.” such as massage and chiropractic care, may help to promote a relaxation response and release tense muscles that make pain worse. And physical practices like yoga, qi gong and tai chi can help improve physical function, suppress pain, boost immunity, relieve anxiety and enhance quality of life.
5. Reduce Inflammation By Quitting Smoking & Other Unhealthy Habits
Quitting smoking, maintaining a healthy weight, getting enough sleep, avoiding exposure to toxins, and regularly exercising are all great ways to control inflammation.
Research suggests that people who drink high amounts of alcohol and smoke or use tobacco products are more likely to suffer from serious bladder, pelvic and colon-related conditions than those who do not smoke or drink heavily. This is even true of bladder and colorectal cancers. Keep your alcohol consumption in check by having no more than two drinks a day if you’re a man, or one drink a day if you’re a woman. For help quitting smoking, you can talk to a counselor or join an online program that specializes in smoking cessation. You can get started by calling the national quitline at 1-800-QUITNOW or by visiting www.Smokefree.gov.
If you’re able to stay physically active without experiencing lots of pain, exercising will offer protection against inflammation and support your overall health. Gentle, low-impact types of exercises like walking, using an elliptical machine, swimming and stretching are recommended most for those with IC. Exercise may be able to improve your tolerance to pain, boost circulation, support your immune system, and also can help you control your weight. Staying active is also a great way to improve feelings of well-being and lower stress, depression, insomnia or anxiety while you’re working on recovering.
Taking certain supplements can also help reduce inflammation and support your immune system, including vitamin D, probiotics, magnesium and omega-3 fish oil supplements.
6. Pelvic Floor Physical Therapy
Consider visiting a physical therapist who can help you to stretch and strengthen your pelvic floor muscles. A 2012 study published in the Journal of Urology showed that 59 percent of women with IC who received 10 myofascial physical therapy treatment sessions experienced significant improvements in pain, urgency and frequency scores. Myofascial physical therapy worked better when compared to therapeutic massage in women with symptomatic interstitial cystitis/painful bladder syndrome.
PT can reduce muscle spasms and may also help with bladder and bowel control. By slowly training your pelvic floor muscles and bladder, you’ll likely find that your bathroom habits start to feel more normal and in your control.
Ask your healthcare professional for a recommendation for a physical therapist who specializes in pelvic floor issues. Additionally, your PT can teach you how to carefully stretch your tight pelvic floor muscles and keep them relaxed so pain and feelings of urgency are reduced.
Precautions
Just because you’re experiencing pelvic pain and needing to urinate more frequently doesn’t mean you have IC. You’ll first need to rule out other conditions that may be causing your symptoms, like urinary tract infections, bladder cancer, sexually transmitted diseases, kidney stones and endometriosis.
If you’ve been experiencing pelvic or bladder pain for more than several weeks, visit your doctor (or the emergency room if pain becomes severe). Always talk with your doctor about any contributing risk factors that apply to you, such as a history of STDs, pelvic inflammatory disease, bladder infections, UTIs or autoimmune disorders.
Final Thoughts
- Interstitial cystitis (or IC) is a chronic, inflammatory, painful pelvic and bladder condition.
- IC symptoms include: pain and discomfort in the pelvic region and bladder, increased urge to urinate, pain during intercourse, pain that spreads to the genitals and back, physical limitations due to discomfort, and emotional problems including anxiety, distress, depression and trouble sleeping.
- IC is caused by inflammation and damage to the bladder lining. This can be due to autoimmune responses, infection, and changes in nerve signaling near the bladder.
- Risk factors for developing IC include: being a woman, being in your 30s or older, history of autoimmune diseases, history of STDs and/or pelvic inflammatory disease, having had pelvic surgery, eating a poor diet, being very stressed, and smoking.
- The best natural treatments for interstitial cystitis include dietary changes, managing stress, acupuncture, lifestyle changes and physical therapy.










