This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
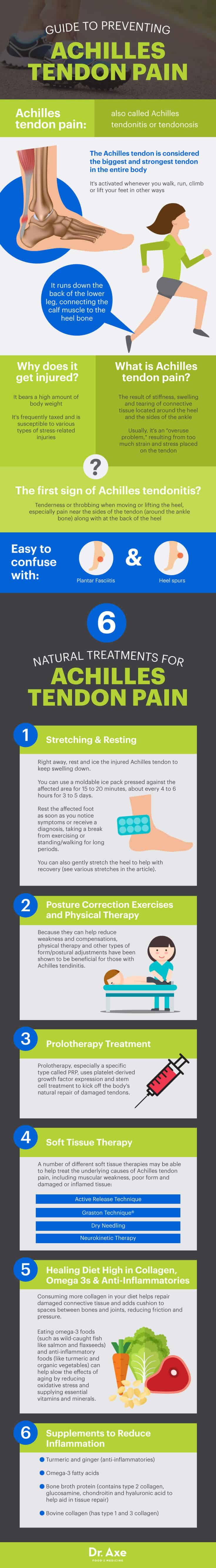
6 Natural Treatments for Achilles Tendon Pain
Reviewed by Ron Torrance, DO, FAOASM
March 26, 2018

Achilles tendon pain, also called Achilles tendonitis or tendonosis, is the result of stiffness, swelling and tearing of connective tissue located around the heel and the sides of the ankle. The first sign of Achilles tendonitis is tenderness or throbbing when moving or lifting the heel, especially pain near the sides of the tendon (around the ankle bone) along with at the back of the heel.
Achilles tendonitis is easy to confuse with other similar conditions, such as plantar fasciitis or heel spurs. Like other common running injuries, the majority of the time Achilles tendon pain is an “overuse problem,” resulting from too much strain and stress placed on the tendon and that causes microtears.
Tendonitis of the Achilles tendon (along with tendonosis) affects runners most often and those who spend lots of time on their feet doing other activities. However, some studies have found that exercise and physical activity isn’t usually the root cause of Achilles pain, rather it seems to provoke inflammation and symptoms that have already been developing. Skipping stretching following exercise, dealing with inflexibility or stiffness, and suffering from weak leg muscles and/or joint degeneration due to aging all seem to be risk factors for Achilles pain.
What Is Achilles Tendon Pain?
The Achilles tendon is considered the biggest and strongest tendon in the entire body, activated whenever you walk, run, climb or lift your feet in other ways. It runs down the back of the lower leg, connecting the calf muscle to the heel bone. Because the Achilles tendon bears a high amount of body weight and is so frequently used, it’s susceptible to various types of stress-related injuries.
Achilles tendon pain will normally develop over time as tiny microtears form within damaged connective tissue at the back of the leg. Tendonitis of the Achilles tendon very commonly gets aggravated from over-exercising, beginning new types of exercises too aggressively, or due to age-related “wear-and-tear” that slowly degenerates tissue.
According to the American College of Foot & Ankle Surgeons, there are two common disorders that occur in the Achilles tendon most often: Achilles tendonitis (also spelled tendinitis) and Achilles tendonosis. (1)
- These conditions sound very similar, but have some important differences — mainly that tendonitis is less serious than tendonosis.
- Achilles tendonitis is an inflammation of the Achilles tendon that usually resolves after some time with treatments, such as rest and stretching.
- Tendonitis of the Achilles tendon can progress if degeneration continues, at which point it’s called Achilles tendonosis. Achilles overuse injuries are also sometimes called tendinopathy, which is characterized by a combination of pain and swelling in the Achilles tendon accompanied by impaired ability to perform strenuous activities.
- Tendonosis is a more complicated condition because it means that the tendon has lost its normal structure, and if left untreated risks chronic degeneration and even rupturing (a full tear). Severe Achilles tendon tears, caused by things like over-exercising or osteoarthritis, can result in rupturing if trauma suddenly impacts the tendon — a common occurrence during athletic competitions, especially in football players.
There are also two types of Achilles tendinitis, depending on the location of inflammation within the tendon: (2)
- Noninsertional Achilles tendinitis: affects the middle portion of the tendon.
- Insertional Achilles tendinitis: affects the lower portion of the heel where the tendon attaches to the heel bone.
Symptoms
One of the most important jobs of the Achilles tendon is helping to raise and lower the heel off the ground, an essential movement for walking and most types of exercise. This is why Achilles tendonitis symptoms are one of the most common sports, exercise or running-related injuries. Achilles tendonitis symptoms usually begin gradually and get worse with activity if ignored and left untreated. (3)
Symptoms of Achilles tendon injuries usually include: (4)
- Pain along the back of your foot, pain above your heel or pain at the sides of the ankle bone.
- Throbbing when moving the heel or ankle, especially when lifting the heel and standing on the toes. Some experience severe pain the day after exercising.
- Developing stiffness, swelling, inflamed tissue, thickening and tenderness near the heel.
- Limited range of motion in the ankle or heel.
- Sometimes hearing unusual noises when moving the tendon, such as snapping or popping sounds.
How might you know that it’s your Achilles tendon causing you pain? You can test if you have Achilles tendonitis by pinching the back and side of the affected foot, near the heel or ankle bone. Sharp pains, limited range of motion when moving the foot and signs of swelling are all indications that the Achilles tendon is inflamed. Another simple test is raising the heel off the ground about 2–3 inches to check for unusual signs of tenderness. If this simple heel-lifting motion causes problems, it’s time to ice, stretch, rest and visit a doctor.
Causes and Risk Factors
As a type of tendonitis, Achilles pain involves inflammation of the soft tissue surrounding muscles and bones. A tendon is a flexible band of fibrous tissue that connects muscles to bone. Tendons work by allowing the pulling movement of muscle to lift a bone in order to cause movement. When the same motion occurs over and over again the tendon can become overly-stretched and strained. Tendonitis also occurs more often with age since tendons become less flexible, weaker and, therefore, more susceptible to injury.
Causes for Achilles heel pain usually include one or a combination of the following. (5)
- A sudden increase in exercise, especially without enough stretching and resting: Middle-aged “weekend warriors,” those who work out vigorously on the weekends but not much during the work week, seem to be very susceptible to Achilles tendon pain.
- Overuse, as in too much repetitive activity involving the Achilles tendon: This can include running, climbing stairs, hiking or walking with unsupportive shoes.
- In athletes, overtraining and not resting enough between workouts: Overtraining puts too much stress on the tendon and doesn’t leave enough time for the body to repair the injured tissue follow exercise. The types of vigorous sports and exercises that are associated with Achilles injuries usually involve quick acceleration, jumping and tackling. Athletes who play football, tennis, rugby and basketball are all at risk for Achilles tendonitis.
- Skipping stretching, which can lead to tight or weak calf muscles: This causes added pressure to be placed on the Achilles tendon due to muscular compensations, poor form and postural problems.
- Having rigid, inflexible leg muscles and/or joints: This can be due to arthritis, a sedentary lifestyle or aging.
- Having any condition that causes joint deterioration and inflammation: This may include an autoimmune disease, frequent infections, gout, thyroid disease or diabetes.
Conventional Treatment
Because inflammation and overuse are commonly tied to Achilles pain, Achilles tendonitis treatment normally includes a combination of:
- Rest (usually including stopping exercise for a period of time). Be sure to avoid “maximum loading” exercises for at least two weeks after injury or substantial pain (jumping, fast runs, heavy strength training).
- Icing the affected area, especially after trauma or sudden injury.
- Compression and elevation (to reduce swelling). Wearing a night splint has been shown to be an effective intervention for Achilles tendinopathy, especially when worn long-term and combined with eccentric exercises and stretching. (6)
- The use of anti-inflammatory medications or sometimes corticosteroids. Over-the-counter pain killers that are commonly recommended first to reduce pain include aspirin, naproxen or ibuprofen. If these don’t do enough corticosteroids might be used on the tendon, but these can be risky for treating Achilles injuries since they sometimes increase the odds of rupturing due to weakness and pressure.
- In severe cases, sometimes surgery is needed. Surgery is usually only recommended after trying all other options for at least six months. Arthroscopic or open surgery are sometimes used to repair severely damage tissue, treat injuries due to trauma, or relieve pressure and chronic pain. It’s been found that about 70–90 percent of patients who require surgery for moderate Achilles injuries return to physical activity after about 6–7 months. (7)
Natural Treatments
1. Stretching and Resting
Right away, rest and ice the affected Achilles tendon to keep swelling down. Ice is most effective when used right away, so don’t wait! You can use a moldable ice pack pressed against the affected area (with a thin cloth between the ice pack and the Achilles, or use an ice pack in a sleeve) for 15 to 20 minutes, about every 4 to 6 hours for 3 to 5 days. Rest the affected foot as soon as you notice symptoms or receive a diagnosis, taking a break from exercising or standing/walking for long periods.
You can also gently stretch the heel to help with recovery. The key is to avoid stretching too aggressively (especially in the beginning), since this can make pain worse in some cases. If you notice sharp pain when stretching, wait until this subsides to begin. Hold static Achilles tendon stretches for about 10–30 seconds at a time, ideally repeating several times daily. Although slightly uncomfortable at first, with time, stretching should lead to less pain overall. Many stretches are also performed with slow repetitions, which you can increase as pain continues to go away.
Several stretches to help resolve Achilles tendon pain are below:
- Wrap a strap or another band (such as a theraband used by some physical therapists) under your affected foot for resistance, placing it under the toes and then tilting the heel back gently. Pump the heel slowly and carefully to loosen up the tendon, repeating about 10–15 times. Do three sets of 10–15 repetitions daily, unless you notice soreness and increased pain.
- Stand at the edge of a stair with just the front half of your foot on the stair. Lift your heels off the ground then slowly lower your heels to the lowest point possible. Repeat 5–15 times, several times daily.
- Improve the flexibility of the ankle joints and varying your exercise moves to include all different ranges of motion. Roll the ankles in small circles in the air while laying down, or lift the toes against a wall while gently pumping the heel.
- Stretch and strengthen the calves to reduce stiffness and weakness. Sit on the edge of a couch with your feet flat on the floor. With one leg, keeping your heel on the floor, lift and point the toes toward the ceiling so that you feel a stretch in your calf muscle. Hold for 30 seconds, then do the same with the other leg, three times per leg.
- When you have strong calf muscles, you reduce the risk of Achilles injury by reducing the stress placed in that area during activity. Calf exercises include performing calf raises done while either standing, sitting, with one foot at a time, or even using stairs.
2. Posture Correction Exercises and Physical Therapy
Because they can help reduce weakness and compensations, physical therapy and other types of form/postural adjustments have been shown to be beneficial for those with Achilles tendinitis (especially noninsertional tendinitis). A physical therapist or another trained practitioner can help show you how to correctly perform eccentric exercises and stretches targeting the Achilles, along with improving posture and range of motion in other ways to prevent future injury.
For those recovering from surgery or severe injury, physical therapy is an important part of healing correctly and usually needs to be sustained for about 6–12 months.
3. Prolotherapy Treatment
Prolotherapy, especially a specific type called PRP, uses platelet-derived growth factor expression and stem cell treatment to kick off the body’s natural repair of damaged tendons. A 2010 Journal of the American Medical Association study compared two forms of prolotherapy (saline and PRP) for treating tendon injuries and found they had similar effects. Both treatments helped treat chronic Achilles tendinopathy, although some speculate that PRP might be best suited for this kind of injury. (8)
4. Healing Diet High in Collagen, Omega 3s and Anti-Inflammatories
Collagen is the most abundant natural protein found in the whole body, giving connective tissue its durability and strength. Consuming more collagen in your diet helps repair damaged connective tissue and adds cushion to spaces between bones and joints, reducing friction and pressure. Consuming more collagen from sources like bone broth may help increase connective tissue (tendon or joint) strength and prevent age-related injury.
I also recommend eating omega-3 foods (such as wild-caught fish like salmon, grass-fed beef, chia seeds and flaxseeds), organic vegetables, organic fruits and herbs like turmeric, garlic and ginger. These anti-inflammatory foods can help slow the effects of aging by reducing oxidative stress and supplying essential vitamins and minerals. A healthy diet may help you recover better, experience less complications and get you back on your feet faster.
5. Soft Tissue Therapy
A number of different soft tissue therapies may be able to help treat the underlying causes of Achilles tendon pain, including muscular weakness, poor form and damaged or inflamed tissue. Consider visiting a trained practitioner in one of the following manipulative therapies, which have been shown to help eliminate joint or muscular pains and help people overcome injuries:
6. Supplements to Reduce Inflammation
To reduce inflammation associated with aging, stress and trauma, I recommend taking the following supplements:
- Turmeric and ginger (anti-inflammatories)
- Omega-3 fatty acids
- bone broth (contains type 2 collagen, glucosamine, chondroitin and hyaluronic acid to help aid in tissue repair)
- Bovine collagen (has type 1 and 3 collagen)
- Antioxidant-boosting compounds, including resveratrol, green tea, medicinal mushrooms like cordyceps, and berry extracts, such as acai or goji. These have anti-aging effects and have numerous benefits beyond protecting joints/tendons.
Facts and Figures
- As of the early 2000s, there are an estimated 232,000 Achilles injuries due to sports alone in the U.S. every year. It’s hard to estimate how many adults deal with mild to moderate achilles pain for other reasons (such as aging or normal exercising), but it’s considered very prevalent. Many with minor pain never see a doctor but rather rest the affected foot and take time off from activity.
- The incidence of Achilles tendon rupture in the general population is only about 7 per 100,000 people. Over 80 percent of ruptures occur during recreational sports.
- About 75 percent of all partial Achilles tendon ruptures are related to sports activities involving abrupt repetitive jumping and sprinting movements. Athletes in running sports also have a high incidence of achilles tendon overuse injuries. (9)
- The majority of Achilles tendon injuries from sports occurs in young to middle-aged males, mainly because of their higher rates of participation in vigorous, contact sports or exercises. About 90 percent of athletes with Achilles injuries will heal and return to their sport following treatment, and only about 3–5 percent need to abandon their training.
- Achilles tendonitis overuse injuries occur at a higher rate in older athletes than younger or middle-aged adults. Overuse injuries are most common in middle-aged “weekend warriors” who exercise vigorously only 1–2 days per week.
- Strengthening and stretching the calf muscles is very important for Achilles tendonitis treatment; studies have found that eccentric (heel‐drop) training helps about 80 percent of patients return to their previous activity level and reduce pain substantially. (10)
Precautions
No matter what treatment method you choose, remember that pain can always come back, so prevention of achilles injuries is very important. To help prevent inflammation of the Achilles tendon and decrease risk for severe injury or rupture, keep the following in mind:
- When starting a new type of exercise, begin slowly and always stretch afterwards.
- Try to cross-train and vary workouts to prevent overuse.
- Strengthen and stretch muscles around any painful joint to reduce compensations.
- Take breaks between workouts, especially from repetitive activities.
- Don’t push yourself too hard. Stop activities if they start to cause throbbing or swelling.
- Try not to sit for long periods, but rather get up and stretch or walk around to prevent stiffness.
- Practice good posture, or speak to a professional if you’re concerned about poor form.
- If you’ve suffered any injuries in the past and notice pain coming back, talk to your doctor to get an opinion about which types of exercises and activities might be risky.
Final Thoughts
- Achilles tendon pain is the result of inflammation, tearing or over-stretching of the large band of connective tissue running down the back of the calf and meeting at the heel. Overuse, trauma caused during athletic competitions and aging are all risk factors.
- Symptoms of Achilles tendonitis include stiffness, swelling or tenderness near the heel (especially the sides) along with trouble exercising or walking and limited range of motion in the heel. Pain when lifting the heel is a good indication of Achilles pain.
- Treatments for Achilles tendon pain include rest and gentle stretching, active release technique and/or other soft tissue therapies, supplementation, exercise, physical therapy and a diet high in collagen.










