This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
What Your Chest Pain Means + 9 Natural Treatments & Prevention
April 15, 2018

Few things are as frightening as chest pains. The first thing that comes to mind is a heart attack. While chest pains and heart attacks often do go hand-in-hand, there are so many other conditions that can cause similar discomfort and pain. Some of the causes are quite serious and potentially fatal, and other causes are less serious and respond well to treatment.
Chest pain is often described as squeezing, stabbing, tightness, pressure or general discomfort and it can occur in several different areas of the chest. As a result of some conditions, the pain may radiate or spread to other parts of the body. Chest pain is a symptom of many serious health conditions, including those affecting the heart and lungs. Many of these conditions require emergency medical attention.
What Are Chest Pains?
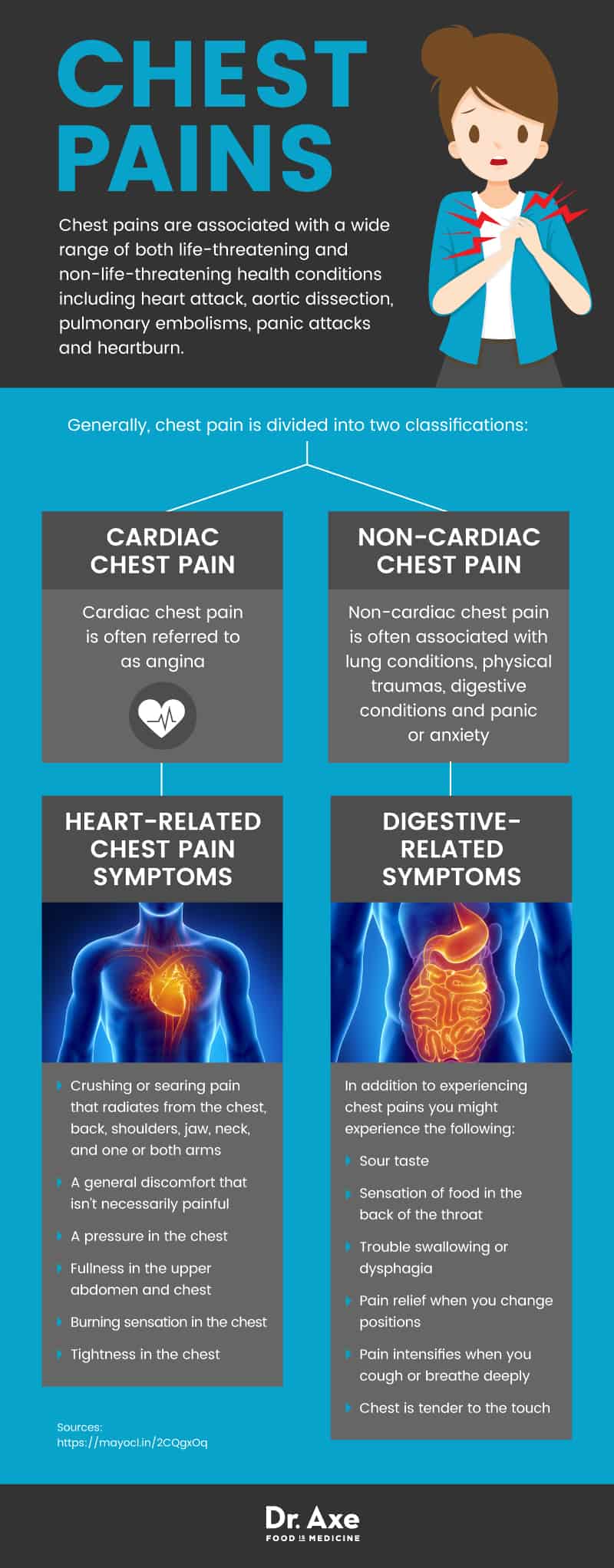
Chest pains are associated with a wide range of both life-threatening and non-life-threatening health conditions including heart attack, aortic dissection, pulmonary embolisms, panic attacks and heartburn. Generally, chest pain is divided into two classifications: cardiac chest pain and non-cardiac chest pain.
Cardiac chest pain is often referred to as angina. Several conditions that present with chest pains include heart attacks, atherosclerosis and coronary spasms. Non-cardiac chest pain is often associated with lung conditions, physical traumas, digestive conditions and panic or anxiety. (1)
The discomfort can come on quickly and occur in a variety of places, depending on the root cause. For example, if you experience pressure or burning along with shortness of breath, you may be having cardiac chest pains. If on the other hand, you experience chest pain, a rapid heart rate, an intense sense of fear and sweating, then you may be having a panic attack. Either way, seeking emergency medical attention is advised.
Less serious conditions that are associated with chest pains include panic or anxiety attacks, stomach ulcers, shingles, muscular/skeletal injuries, heartburn, GERD, gallstones and esophageal spasms. However, these conditions still need to be diagnosed appropriately to ensure that your chest pain isn’t associated with a more serious condition. (2)
Signs and Symptoms
Chest pain signs and symptoms vary quite widely. Here are the most common, broken down by root cause. (3)
Heart-Related Chest Pain Symptoms
- Crushing or searing pain that radiates from the chest, back, neck, jaw, shoulders and one or both arms
- A general discomfort that isn’t necessarily painful
- A pressure in the chest
- Fullness in the upper abdomen and chest
- Burning sensation in the chest
- Tightness in the chest
- Generalized pain that continues for more than just a few moments and gets worse with activity
- Pain that may come and go
- Shortness of breath
- Cold sweats
- Dizziness
- Weakness
- Nausea
- Vomiting
Aortic Dissection Symptoms
This is a potentially life-threatening condition, albeit fairly rare. Call 911 if you experience any of the following symptoms — especially if aortic dissections run in your family. As symptoms mimic many other cardiac events, be sure to communicate any previous aortic conditions or family history with emergency responders. (4)
- Pain in the upper back
- Breathlessness
- Fainting
- Weakness
- Paralysis
- Trouble speaking or communicating
- Weaker pulse in one arm than the other
- Confusion
- Dizziness
Lung-Related Symptoms
Certain lung conditions may present with generalized chest pains including:
- Pulmonary Embolism: An event where a blood clot becomes lodged in a pulmonary artery, blocking blood flow to the lung tissue. Pain from a pulmonary embolism is generally accompanied by a fast or irregular heartbeat, sudden difficulty breathing, fainting or lightheadedness. Call 911 as a pulmonary embolism is life-threatening.
- Pleurisy: A condition in which the membrane that covers the lungs becomes inflamed. Chest pains often occur during deep breathing, coughing or sneezing.
- Pneumonia: Shortness of breath and sharp chest pains are typical symptoms with pneumonia. Pneumonia is often accompanied by other symptoms that indicate an infection like fever, chills, shortness of breath and sharp pains, which worsen with deep breaths or physical activity like climbing stairs.
- Collapsed Lung: Caused by a trauma or other underlying condition, a collapsed lung is associated with shortness of breath and acute chest pains.
- Pulmonary Hypertension: High blood pressure in the arteries of the lungs and the right side of the heart can cause pulmonary hypertension. Shortness of breath during activity, fatigue, chest pain and/or pressure, edema in the legs, ankles or ascites, racing pulse, heart palpitations and bluish skin and lips are signs of this potentially life-threatening condition. (5)
Digestive-Related Symptoms
Several digestive tract conditions including GERD, indigestion, gallstones and certain pancreatic symptoms can present with chest pains. In addition to experiencing chest pains you might experience the following:
- Sour taste
- Sensation of food in the back of the throat
- Trouble swallowing or dysphagia
- Pain relief when you change positions
- Pain intensifies when you cough or breathe deeply
- Chest is tender to the touch
- Pain persists for several hours
- Heartburn
- Painful, burning sensation behind your breastbone
Muscular/Skeletal-Related Symptoms
- Injury or Trauma: Injury to the ribs or chest cavity or overexertion of chest muscles can cause generalized chest pains that are dull, stabbing, sharp or electrifying in nature.
- Costochondritis: Often associated with fibromyalgia, costochondritis can cause non-cardiac related pain. It often presents as a stabbing, aching or burning pain in the chest wall and rib cage. It often worsens with activity or exercise, sneezing, coughing or exercise. The pain can radiate to arms and the shoulders.
Anxiety/Panic Attack-Related Symptoms
Researchers from Massachusetts General Hospital and Harvard Medical School recognized in 2002 that nearly 25 percent of patients who seek treatment for chest pain also have a panic disorder. (6)
Chest pain is one of the most common symptoms of a panic attack and the pain is often accompanied by rapid heartbeat, rapid breathing, profuse sweating, intense fear, shortness of breath, dizziness, nausea and a fear of dying.
Causes and Risk Factors
Recognized causes of chest pain can stem from heart, lung, digestive, emotional, muscular and other causes, including: (7)
Heart-Related Causes
- Heart Attack: When blood flow is blocked to the heart muscle. This is often the result of narrowed arteries or a blood clot.
- Angina: Generally recognized as chest pain caused by poor blood flow to the heart. Angina is often caused by a buildup of plaque in the arteries that restrict the heart’s blood supply, particularly during exertion. (8)
- Pericarditis: An inflammation of the sack around the heart, the pericardium, can cause chest pains. Pericarditis can be caused by a virus or other infection, injury, radiation therapy or may be a side effect of certain medications.
- Aortic Dissection: A life-threatening condition where the main artery from the aorta is damaged, separating the inner layers of the blood vessel. Blood is then forced between the layers, causing the rupture.
Lung-Related Causes
- Pulmonary Embolism: A blood clot becomes lodged in the pulmonary artery blocking the flow of blood to the lung tissue. Pain is generally accompanied by a fast or irregular heartbeat, sudden difficulty in breathing or lightheadedness with a pulmonary embolism. Call 911 if these symptoms present.
- Pleurisy: When the membrane that surrounds the lungs becomes inflamed, it is called pleurisy. This can cause chest pains that worsen with a cough, sneeze or deep breath.
- Pneumonia: Generally caused by an infection, pneumonia often presents with sharp chest pains and shortness of breath. These symptoms are often accompanied by a fever, chills or coughing.
- Collapsed Lung: When a lung collapses, chest pain can begin suddenly and last for several hours. The pain is often accompanied by shortness of breath.
- Pulmonary Hypertension: High blood pressure in the arteries that carry blood to the lungs can cause chest pains.
Digestive-Related Causes
- Heartburn: Chest pain that presents as a painful, burning sensation behind the breastbone. It generally happens as the acid washes up from the stomach into the esophagus.
- Swallowing Disorders: Esophagus disorders that make swallowing difficult or painful can cause chest pains similar to cardiac-like chest pains.
- Gallstones: Gallstones or an inflammation of the gallbladder can cause abdominal pain that radiates to the chest area, simulating chest pains.
- Pancreatitis: An inflammation of the pancreas can cause a potentially dangerous condition called pancreatitis. Both chronic and acute pancreatitis can cause upper abdominal pain that radiates to the back and is often described as chest pain. It is often accompanied by an increased heart rate, fever, nausea and a swollen or tender abdomen. (9)
Muscular/Skeletal-Related Causes
- Bone & Muscle Causes: Chronic pain syndromes, fibromyalgia, or injured, bruised or broken ribs may cause chest pains.
- Costochondritis: Often associated with fibromyalgia, trauma, overuse or arthritis, it is an inflammation of the chest wall between the ribs and breastbone that can cause a stabbing and aching pain in the chest.
Anxiety and Panic-Related Causes
Anxiety and panic attacks can cause intense chest pain that is often accompanied by intense fear, rapid heartbeat, rapid breathing, profuse sweating, shortness of breath, nausea and a fear of dying. The chest pain symptom often lasts only a moment or two.
Shingles
A reactivation of the virus that causes chickenpox causes and extremely painful band of blisters around the back and chest wall is called shingles.
Diagnosis
If you go to the emergency room or call 911 with chest pains (which is advisable) your medical history and family history will be considered, in addition to the acute symptoms you are experiencing. To determine the root cause of your chest pains, your medical team will order a wide range of tests.
Heart-Related Diagnosis
If your symptoms appear to be related to your heart, your emergency medical team will order a range of tests, including an electrocardiogram (ECG), certain blood tests, chest X-rays and a CT scan. If certain heart conditions are suspected, further testing may include: (10)
- CT Angiogram: A CT with dye that checks the heart arteries and lung arteries for blockages and other problems.
- Stress Test: Used to measure how the heart and blood vessels respond to exertion. A treadmill, stationary bike may be used, or a drug may be administered, to stimulate the heart to measure its health and strength.
- Coronary Catheterization (Angiogram): Used to identify individual arteries of the heart that may be blocked or narrowed. A liquid dye is injected into the arteries through the wrist or groin. As the dye fills the arteries, the medical team can see blockages and other abnormalities on X-rays.
- If an aortic dissection is suspected, this is a life-threatening condition that requires specialized tests, including: (11)
- TEE or Transesophageal Echocardiogram: Used to get an image of the heart to determine if there is an aortic dissection
- MRA or Magnetic Resonance Angiogram: Used to examine blood vessels and any damage.
Lung-Related Diagnosis
When an initial test or your medical history indicates that the chest pain may be a result of an issue in the lungs, further tests will be ordered depending on the symptoms. Often testing begins with blood tests, chest X-rays, CT scans, ultrasounds and an ECG. When the following conditions are suspected, additional tests may be ordered.
- Pulmonary Embolism: Pulmonary angiogram to determine if there is a blood clot in the lungs. (12)
- Pleurisy: A surgical diagnostic procedure like a thoracentesis, thorascopy or pleuroscopy will likely be ordered. (13)
- Pneumonia: Blood culture, sputum test, pleural fluid culture, pulse oximetry and bronchoscopy may be performed to determine the type of pneumonia. (14)
- Collapsed Lung: Arterial blood gas test may be ordered. (15)
- Pulmonary Hypertension: MRI, pulmonary function tests, right heart catheterization, ventilation/perfusion scan and an open-lung biopsy may be required. In addition, genetic tests may be ordered to check for a genetic mutation often linked to pulmonary hypertension. (16)
Digestive Diagnosis
- Heartburn: Chest X-rays, an endoscopy, acid probe tests and esophageal motility testing may be ordered to determine if heartburn is at the root of the chest pains being experienced. (17)
- Gallstones: If gallstones or a gallbladder problem is believed to be causing chest pains, an abdominal ultrasound as well as a CT, HIDA scan, MRI, ERCP and a variety of blood tests will likely be ordered. (18)
Muscular/Skeletal Testing
- Injury or Trauma: To determine if the chest pain is associated with a physical injury or trauma, certain physical examinations, X-rays and other imaging tests may be required.
- Fibromyalgia: If the pain is believed to be associated with fibromyalgia, a thorough medical examination and medical history will be taken along with blood tests and pain testing. (19)
- Costochondritis: To check for swelling and tenderness in the chest, a physical examination will be conducted. Diagnosis will likely require chest X-rays, a CT or MRI and an ECG. (20)
Panic/Anxiety Attack
In addition to a physical examination, blood tests including thyroid function tests, a psychological evaluation and an ECG are likely. (21)
Conventional Treatment
The treatment of chest pains depends on the root cause found during diagnosis.
Heart-Related Conventional Treatments
- Nitroglycerin: Used to prevent chest pain for those with coronary artery disease. It works by relaxing and widening blood vessels so blood flows more freely through narrow spaces. (22)
- Aspirin: Daily low dose aspirin therapy may be prescribed to lower the risk for heart attack as it interferes with the blood’s clotting action. (23)
- Thrombolytic Drugs: If you are having a heart attack, a clot-busting drug is used to dissolve the clot that is blocking the blood from reaching the heart muscle. (24)
- Blood Thinners: If you have a clot in an artery feeding your heart or lungs, drugs that inhibit blood clotting and prevent new clots may be prescribed. (25)
- Angioplasty and Stent Placement: If the chest pain is caused by a blockage in the artery feeding the heart, a surgeon will insert a catheter with a balloon on the end into a large blood vessel in the groin and feed it up to the blockage to widen the artery. A stent also may be placed. (26)
- Bypass Surgery: If you have a blocked artery, surgeons will take a healthy blood vessel from another part of your body to create an alternate path for the blood to travel to your heart. (27)
- Aortic Dissection Repair: Aortic dissections are often fatal and often require surgery. As symptoms mimic other conditions and diseases, proper diagnosis may be delayed. Be sure to communicate any past conditions or family history of aortic dissections. (28)
Lung-Related Conventional Treatments
- Pulmonary Embolism: To keep the clot from getting bigger and to prevent new clots, blood thinners, clot dissolvers and surgical intervention may be required. (13)
- Pleurisy: Treatment focuses on the underlying cause of the inflammation. (14)
- Pneumonia: Treatment depends on the type of pneumonia diagnosed; antibiotics or antiviral medications may be prescribed. (15)
- Collapsed Lung: Depending on the severity of the situation, treatment may range from observation to surgical intervention. (29)
- Pulmonary Hypertension: Prescription medications including blood vessel dilators are administered continuously through an IV catheter. Additional medications including endothelin receptor antagonists, sildenafil, tadalafil, anticoagulants, high-dose calcium channel blockers and diuretics may be prescribed. Oxygen may be administered and in rare cases a lung or heart-lung transplant may be required. (18)
Digestive-Related Conventional Treatments
- Heart Burn: Antacids, H-2 receptor antagonists and proton pump inhibitors (PPIs) may be recommended and prescribed depending on the severity and the frequency of the symptoms. (30)
- Gallstones: Medications are often prescribed to dissolve the gallstones and, in some cases, surgery to remove the gallbladder may be required. (20)
Muscular/Skeletal Conventional Treatments
- Fibromyalgia: Pain relievers, antidepressants, anti-seizure drugs, physical therapy, occupational therapy and counseling are often prescribed. (21)
- Costochondritis: NSAIDs, narcotic pain relievers, antidepressants, anti-seizure medications and physical therapy are often prescribed for this condition. (22)
Anxiety & Panic Conventional Treatments
- Antidepressants: Often prescribed for panic attacks and anxiety disorder, tricyclic antidepressants may be prescribed to reduce the number and the severity of panic attacks. (31)
- Antianxiety Medications: Benzodiazepines may be prescribed to provide rapid intervention in the event of a moderate to severe panic attack. (32)
- Psychotherapy: With or without medication, psychotherapy, cognitive behavioral therapy, biofeedback and relaxation techniques are often prescribed with moderate to severe conditions. (33)
Shingles Treatment
Research shows that this painful, blistering rash can increase the risk of heart attack by 59 percent and the risk of stroke by 35 percent in the months and years following diagnosis. (34) Stay in touch with your medical team and be sure to seek emergency medical attention for any chest pain or stroke symptoms. The treatment of shingles often includes the administration of antiviral drugs and pain medications. (35)
Natural Treatments and Prevention
1. Quit smoking, especially when your chest pains are related to heart disease or lung disease. Smoking is the leading cause of heart disease and heart attacks. But, when you quit smoking, within 24 hours your risk for a cardiac event starts to decline. And, it just takes nine months for your lungs to heal significantly.
The healing continues and at five years smoke-free, your arteries and blood vessels start to widen again, lowering your risk for clots and a stroke. After 10 years of being smoke-free, your chance of lung cancer is half. And finally, 20 years after your last cigarette, your risk of coronary heart disease is the same as a nonsmoker. (36, 37)
2. Eat for your health. When your chest pains are caused by heart conditions, it is vital that you start following a diet that focuses on heart-healthy foods that help to reduce cholesterol levels and lower your blood pressure. Following a high-blood pressure diet may help to relieve your symptoms and start the healing process.
Central to your diet should be lean proteins like wild-caught salmon and free-range poultry and plenty of fiber-rich foods like oats, leafy green vegetables like kale, sprouted whole grains, artichokes, raspberries, split peas and apples and pears with their skins. (38)
In a systematic review of clinical studies, researchers found that high-fiber diets are associated with a reduction of risk in cardiovascular disease and coronary heart disease. (39) Start your day with a healthy bowl of overnight oatmeal that’s ready to consume when you rise and for lunch enjoy a nutrient-dense salad. For dinner, enjoy a hearty bowl of chicken paprikash.
3. Exercise daily: With your physician’s approval, exercise daily to help reduce stress, lower blood pressure, improve heart health, and to lose excess weight. (40)
Walking is a great way to start exercising after a cardiac-related diagnosis. Listen to your body and get moving. Adding 2,000 steps a day to your daily routine equates to nearly a mile. Set a target of 10,000 or 12,000 steps a day as you grow stronger. The goal is to walk at least 30 minutes each day, as briskly as you can. To build strength and balance, in addition to walking, add a 10-minute at-home workout to your day. And, as you continue to heal and your conditioning improves, swimming and tennis are great to add to your weekly exercise routine.
4. Avoid common trigger foods including alcohol, caffeine, processed foods, artificial sweeteners, spicy foods and fried foods if your chest pains are related to digestive conditions. Eat a nutrient-dense diet that includes plenty of fresh, organic vegetables and fruits, healthy fats, probiotics, free-range chicken and grass-fed beef.
5. Eat three or more servings of magnesium-rich foods and take 55 micrograms of selenium daily when your chest pains are associated with fibromyalgia. According to an older small study, selenium and magnesium deficiency is linked to muscle pain in fibromyalgia patients. (41)
6. TENS, or transcutaneous electrical nerve stimulation, use helps to interrupt and mask pain signals for those with costochondritis, according to the Mayo Clinic. (22, 42)
7. Practice guided meditation or mindfulness 30 to 45 minutes daily to relieve stress and anxiety. Stress is a universal side effect (or contributing factor) of many of the conditions associated with chest pains. Finding a way to manage it is essential for your long-term health. (43)
8. Take ashwagandha (500 milligrams, twice daily) to stabilize your stress response and to improve anxiety symptoms, according to multiple studies. For those with an anxiety disorder, taking ashwagandha significantly improves anxiety scores over a placebo according to a study published in the Journal of Alternative and Complementary Medicine. (44)
Another small clinical study of patients with moderate-to-severe anxiety found that a combination of dietary counseling, deep breathing relaxation techniques, a multivitamin and an ashwagandha supplement resulted in a 56.5 percent decrease in anxiety scores. (45)
9. Diffuse lavender oil to help relax the body and the mind to relieve anxiety, nervousness and improve sleep quality. Researchers at the University of Minnesota School of Nursing found that inhaling lavender essential oil during sleep improves sleep quality. (46)
Precautions
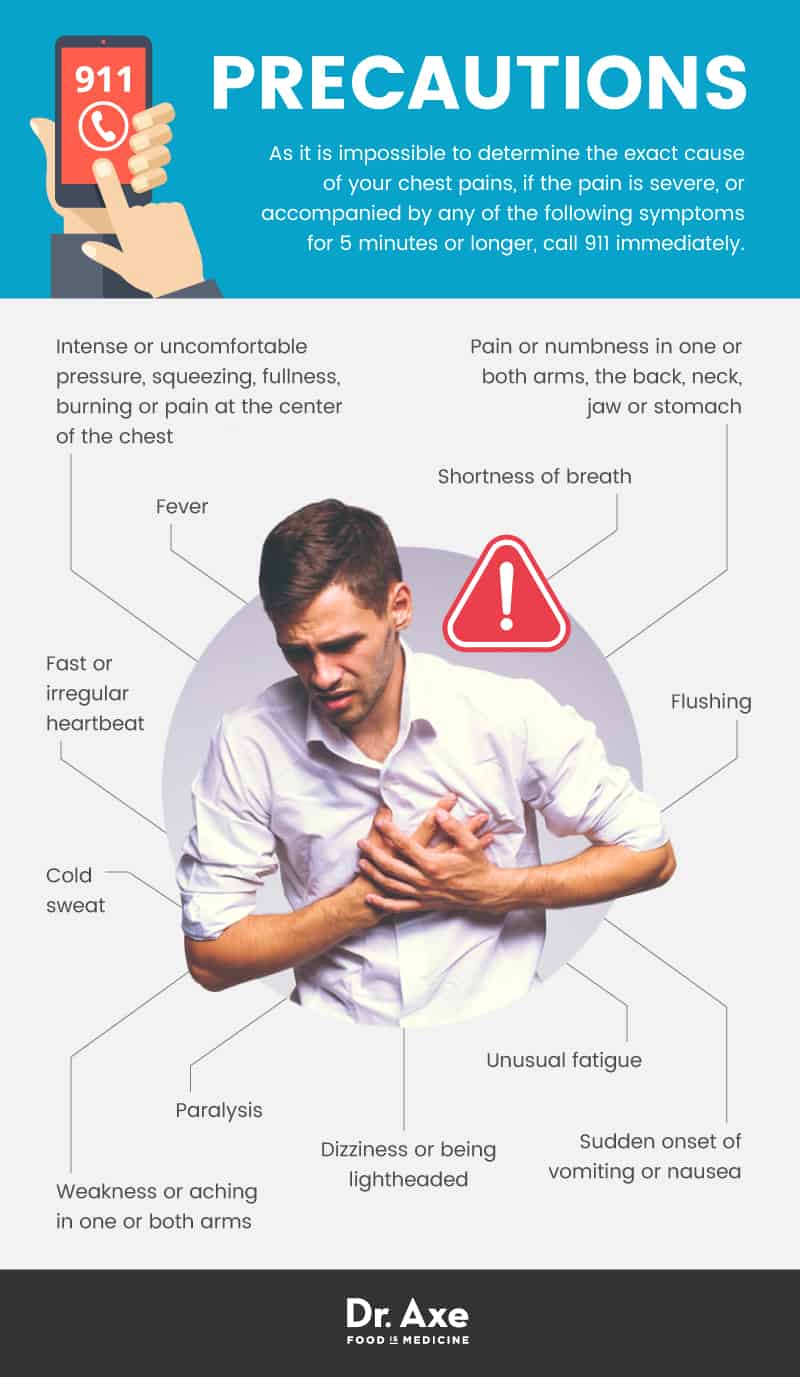
As it is impossible to determine the exact cause of your chest pains, if the pain is severe, or accompanied by any of the following symptoms for five minutes or longer, call 911 immediately. (47)
- Intense or uncomfortable pressure, squeezing, fullness, burning or pain at the center of the chest.
- Pain or numbness in one or both arms, the back, neck, jaw or stomach
- Shortness of breath
- Sudden onset of vomiting or nausea
- Dizziness or being lightheaded
- Unusual fatigue
- Flushing
- Cold sweat
- Weakness or aching in one or both arms
- Paralysis
- Fast or irregular heartbeat
- Fever
Final Thoughts
- Chest pains are associated with a wide range of conditions, including cardiac problems, lung problems, digestive tract conditions, muscular/skeletal conditions and anxiety.
- Seek medical treatment immediately if you experience chest pains along with numbness, paralysis, unusual fatigue, fever, cold sweats, dizziness, shortness of breath or a sudden weakness in one or both arms.
- Conventional treatment and natural treatments depend on the root cause of the chest pain. Some causes require emergency intervention while other causes may be effectively treated with a healthy diet and practicing relaxation and mindfulness.








