This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Raynaud’s Syndrome (+ 6 Tips for Natural Raynaud’s Treatment)
February 17, 2018

Do you ever experience a numb or tingling feeling in your fingers and toes when it’s really cold outside? For most people this is just an occasional problem that occurs when blood flow to your extremities is reduced. But for some people this is an ongoing problem that leads to uncomfortable and unsightly attacks or episodes.
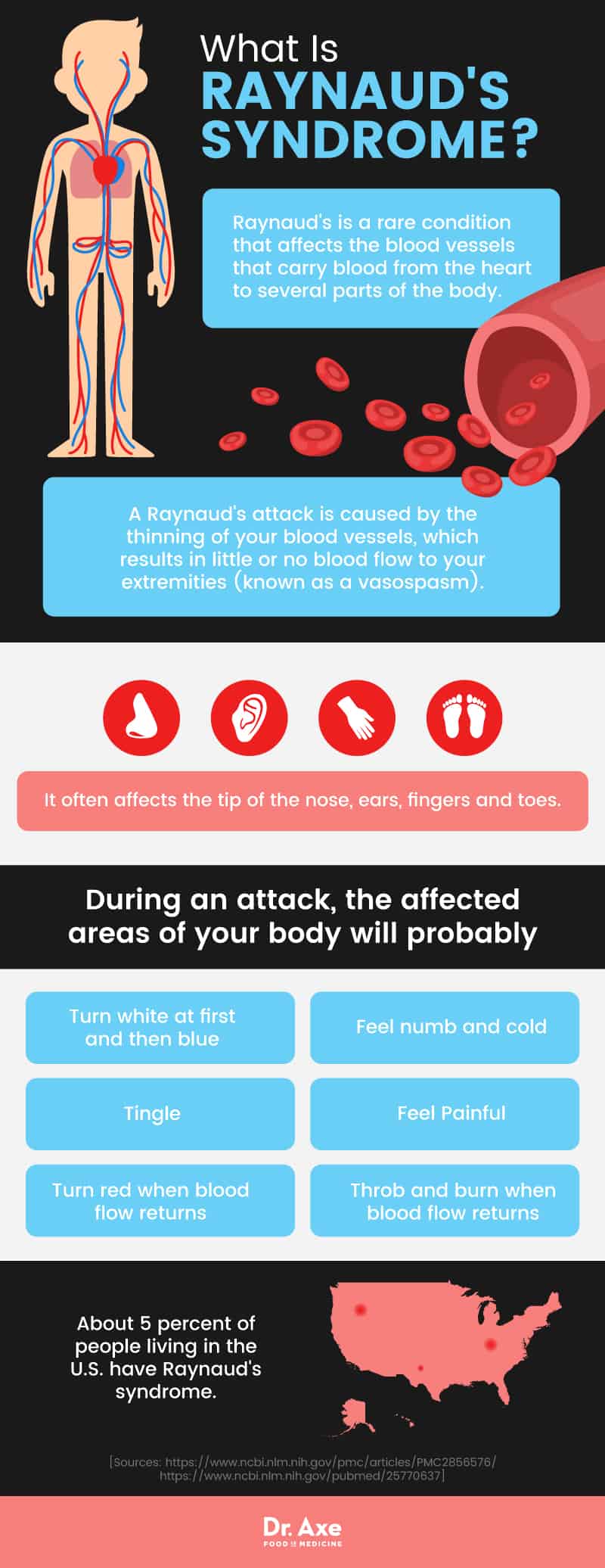
About 5 percent of people living in the United States have Raynaud’s syndrome. There are two types of this condition — one that happens sporadically and can’t be explained and another that’s linked to other health conditions, especially autoimmune diseases like scleroderma. Dealing with Raynaud’s can be scary and frustrating, but there are natural ways to reduce the severity and frequency of attacks that leave your fingers blue and numb. By controlling your low body temperature, reducing your stress levels and avoiding activities that can trigger reduced blood flow, you’ll be able to take charge of your symptoms so that they’re a thing of the past.
What Is Raynaud’s Syndrome?
Raynaud’s is a rare condition that affects the blood vessels that carry blood from the heart to several parts of the body. People with Raynaud’s experience brief episodes of vasospasm, which causes the blood vessels to narrow and reduce blood flow to your extremities.
The condition was first described in 1862 by a French physician named Maurice Raynaud. He explained the “tricolor change” that occurs when the blood vessels narrow and cut off blood supply to the extremities. At first your fingers and toes appear pale or white and then they quickly become bluish because of a lack of oxygen. Then, when the blood rushes back to these areas, they turn red. (1)
There are two types of Raynaud’s that are different because of their root causes and symptoms. Primary Raynaud’s, which is also called Raynaud’s disease, is the more common form of this disorder and it’s known to be less severe. The cause of primary Raynaud’s isn’t known, but the condition is known to be isolated from other health problems and it results in reduced blood flow to the arteries.
Secondary Raynaud’s — often called Raynaud’s phenomenon — is the more severe form of this condition affecting the arteries. It’s believed to be caused by an underlying disease or health condition, like connective tissue disorders, or other environmental and lifestyle factors.
Signs & Symptoms
The symptoms of both primary and secondary Raynaud’s syndrome are similar. People with Raynaud’s usually experience an attack that’s triggered by exposure to cold temperatures or stress. The attack usually affects the fingers and toes, but symptoms are sometimes noticeable in the ears, nose, lips and nipples as well. Symptoms may develop in different areas of the body during each attack, and they don’t necessarily occur in all of your fingers and toes at one time. The symptoms may only be noticeable in one or two fingers or toes, or start there and then spread to the others.
A Raynaud’s attack is caused by the thinning of your blood vessels, which results in little or no blood flow to your extremities. This is referred to as “vasospasm,” which is the term used to describe the sudden constriction of your blood vessels. During an attack, the affected areas of your body will probably: (2)
- Turn white at first and then blue
- Feel numb and cold
- Tingle
- Feel painful
- Turn red when blood flow returns
- Throb and burn when blood flow returns
Not only does the loss of blood flow cause Raynaud’s symptoms, but the return of blood flow also leads to a throbbing and burning sensation until the attack is over.
The duration of a Raynaud’s attack varies. It can last only a few minutes or linger for many hours. Depending on what triggers your attacks, you may experience them every day, even several times a day, or only once in a while.
There are some complications that are associated with Raynaud’s syndrome. Secondary Raynaud’s can produce tissue ischemia, which is caused by an inadequate supply of blood to parts of the body. This can result in digital ulcers, which causes sores to develop on your fingers and toes, and gangrene, which refers to the actual death of body tissue in your extremities. Although this is rare, Raynaud’s can also lead to amputation. (3)
Causes & Risk Factors
Although the cause of primary Raynaud’s isn’t known, there are some triggers that can lead to an attack. The two most common triggers include:
- Cold temperatures: Exposure to cold temperatures is known to trigger a Raynaud’s attack, leading to the sudden constriction of the blood vessels and reduced blood flow in the extremities. Research shows that being exposed to cold temperatures, especially for those with other skin or blood conditions, can provoke more Raynaud’s attacks. (4)
- Stress: Higher stress and anxiety levels are related to more Raynaud’s attacks, even when you aren’t exposed to cold temperatures. Stress and anxiety is also linked to greater attack severity at all temperatures, according to research published in the Journal of Behavioral Medicine. (5)
Secondary Raynaud’s syndrome can be caused by a number of conditions or factors. Many people with Raynaud’s have another disease or health condition that affects their arteries or nerves. The diseases that are most commonly linked to Raynaud’s syndrome include:
- Scleroderma: Scleroderma is an autoimmune, connective tissue disease that literally means “hard skin.” It is caused by the abnormal growth of connective tissue that supports your skin and internal organs. For people with scleroderma, their skin becomes thick and hard, and they experience a buildup of scar tissue. The blood vessels can be affected by systemic scleroderma, which limits blood circulation to smaller arteries in the body, like those found in your fingers and toes. Research shows that most people with this condition experience Raynaud’s symptoms, usually early on in the course of the disease. (6)
- Lupus: Lupus is another type of autoimmune disease that affects the skin. One of the most common lupus symptoms is poor circulation in the extremities, which can cause Raynaud’s attacks. According to research conducted in Brazil, Raynaud’s phenomenon appears in 18 percent to 46 percent of patients with systemic lupus erythematosus, the type of lupus that affects the entire body. (7)
- Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune disease that affects the joints and can lead to swelling in and around certain joints, like those in the hands. Some other rheumatoid arthritis symptoms include joint pain, muscle aches, stiffness and trouble moving normally. Data suggests that rheumatoid arthritis is among the diseases associated with Raynaud’s syndrome. (8)
- Atherosclerosis: Atherosclerosis is a heart or vascular issue that occurs when the blood vessels become thick and stiff. One of the main symptoms of both atherosclerosis and Raynaud’s is sudden numbness in the arms and legs. Because atherosclerosis affects your blood vessels, researchers have found that it’s linked to vasospasm, which slows the flow rate of blood and leads to Raynaud’s symptoms. (9)
- Sjögren’s Syndrome: Sjögren’s syndrome is an autoimmune disease that primarily affects the tear ducts and salivary glands but can also affect soft tissue, joints and nerves in the body. This disease occurs when your body produces extra antibodies in the blood that attack your healthy cells and tissue. Research published in the Journal of Rheumatology indicates that Sjögren’s syndrome and Raynaud’s phenomenon are linked, as a cross sectional study found that 13 percent of patients (40 patients out of 320) with primary Sjögren’s also displayed Raynaud’s symptoms. (10)
- Buerger’s Disease: Buerger’s disease is a condition that affects the blood vessels in your arms and legs. It causes the blood vessels to swell, thereby preventing blood flow and causing clots to form. Buerger’s disease causes symptoms of Raynaud’s syndrome like cold hands and feet, skin color changes, pain in the extremities and painful sores. (11)
- Thyroid Problems: Some people with thyroid problems, especially hypothyroidism, experience an intolerance to cold that can lead to issues with blood flow to the extremities.
- Blood Disorders: Blood disorders that affect the blood vessels and reduce blood flow are also associated with Raynaud’s syndrome. Cryoglobulins, for example, is a blood disorder that’s caused by abnormal proteins in the blood. For people with cryoglobulins, cold temperatures can cause flare ups, leading to clumps in the blood vessels.
Secondary Raynaud’s may also be caused by the following factors: (12)
- Hand and Foot Injuries: Raynaud’s syndrome may develop after an injury to your hand or foot. This can be from an accident or some sort of trauma, a surgical procedure or after developing frostbite.
- Repetitive Actions: Some repetitive actions or movements, like typing, using vibrating tools or playing the piano can damage the arteries and nerves, leading to Raynaud’s symptoms.
- Smoking and Alcohol Consumption: Research shows that smoking and nicotine exposure is one of the biggest risk factors for Raynaud’s. One study also found that heavy alcohol consumption increased the risk of developing Raynaud’s symptoms in women. However, researchers found that moderate red wine consumption reduced the risk of Raynaud’s. (13, 14)
- Certain Medications: Some medications cause the arteries to narrow, reduce your blood pressure or can affect your blood flow. These actions can increase your risk of experiencing a Raynaud’s attack. The medications that may cause secondary Raynaud’s include beta blockers, birth control pills, allergy medications, diet pills, migraine medications that contain ergotamine and some cancer medicines, including cisplatin and vinblastine. (15)
Women are more likely to develop both primary and secondary Raynaud’s than men. Primary Raynaud’s symptoms usually develop before the age of 30, while secondary Raynaud’s symptoms commonly develop after the age of 30.
Conventional Treatment
For most patients with Raynaud’s, avoiding exposure to cold temperatures and focusing on keeping the hands and feet warm has proven to be beneficial in reducing episodes. For those who continue to experience symptoms, a number of pharmacologic and surgical therapies are utilized.
For people who aren’t seeing improved symptoms with lifestyle changes, there are vasodilation strategies that can help to reduce the occurrence of Raynaud’s attacks. This usually involves taking medications that help to regulate your blood flow and avoid the sudden constriction of the blood vessels. Some examples of medications used to do this include nitrates, calcium channel blockers and prostaglandins.
Nitrates are used to widen your blood vessels. Some people with Raynaud’s syndrome use nitrate cream or gel formulations on the affected area to reduce the severity of pain during an attack. But research shows that many patients using nitrates for Raynaud’s experience headaches that limit their use. (2)
Calcium channel antagonists are used for the treatment of severe Raynaud’s cases. However, research shows that these drugs have adverse effects, including headaches, low blood pressure and dilation of the blood vessels. (16)
Prostaglandin E1 is a naturally occurring prostaglandin that’s used as medication to open the blood vessels. Research shows that it can be an effective form of treatment for patients with Raynaud’s phenomenon by limiting attacks and helping to heal digital ulcers. There are some adverse side effects that are associated with prostaglandin E1, including headaches and nausea. (2)
For severe cases of Raynaud’s, surgery may help to prevent attacks. The surgery involves blocking the nerves in the hands and feet, which can help to control blood flow in the arteries. Sometimes, repeated shots may be needed to relieve symptoms after surgery, especially after a few years.
For patients with secondary Raynaud’s, treating the underlying condition that’s causing the attacks is most important.
Related: Why Am I Always Cold? Causes + How to Fix It
6 Natural Remedies for Raynaud’s Syndrome Symptoms
1. Avoid Cold Temperatures
Research shows that proper body insulation and the avoidance of cold temperature exposure are the two most important lifestyle modifications that should be made to avoid Raynaud’s attacks. You have to protect yourself from cold temperatures, which means wearing extra layers and always covering your hands and feet when it’s cold outside. Make sure to wear thick mittens and socks and warm shoes. It may also help to use hand and foot warmers when you are planning on going outside in the cooler months. (2)
Here are some other ways you can avoid exposure to cold temperatures and help to prevent Raynaud’s attacks:
- Be prepared with extra clothing if you are going to an air-conditioned place
- Wear gloves to take something out of your freezer
- Avoid a quick change in temperature, like putting your hands in cold water
- In colder months, warm up your car before driving
- Move your arms and legs around when they are cold to improve blood circulation
- Massage your fingers and toes when they are cold
2. Reduce Emotional and Physical Stress
Emotional or physical stress can cause vasoconstriction and induce Raynaud’s symptoms, so incorporating natural stress relievers into your daily routine can be helpful in reducing attacks. (17) What actions can you bring into your everyday life to reduce your stress levels? Examples include practicing yoga, taking walks outside, or trying meditation or devotional prayer. Make sure to take care of yourself and get enough rest every night.
If you think that having support would help you to work through your emotional stressors, consider cognitive behavioral therapy or joining a support group with like-minded people. Even getting involved with a local religious club, moms’ club or activity club can be a great stress reliever.
When it comes to physical stress, mechanical stresses to your fingers can cause increased vasospastic attacks. Research shows that prolonged exposure to vibrations can lead to blood restriction in your extremities and other repetitive hand movements can be problematic because they may damage your arteries and nerves. Avoiding these practices, when possible, can help to reduce Raynaud’s attacks. (17)
3. Stop Smoking
Research shows that blood flow is reduced in the fingers of people who regularly smoke. For this reason, smokers with both primary and secondary Raynaud’s syndrome should absolutely quit smoking. If you have tried quitting smoking with no success, try using mind-body practices like acupuncture, spinal manipulation, meditation, reiki, guided imagery and relaxation techniques. (18)
4. Eat an Anti-inflammatory Diet
Secondary Raynaud’s is commonly associated with autoimmune disease symptoms, so working to reverse or relieve the condition can also reduce Raynaud’s attacks. One of the best ways to do this is to eat a diet full of anti-inflammatory foods, like omega-3s, green leafy vegetables, berries, wild-caught salmon and bone broth. Nuts and seeds, good quality organic meats, fresh vegetables and spices and herbs are also excellent choices.
In addition to adding these healing foods to your diet, you need to avoid eating foods that weaken your immune system and lead to inflammation. Certain foods can trigger an inflammatory response and make autoimmune symptoms worse. This includes refined carbohydrates, foods made with artificial ingredients and chemicals, alcohol and even caffeine.
5. Try Acupuncture
There is some research to suggest that acupuncture can be helpful in reducing pain and inflammation and improving joint stiffness in patients with Raynaud’s phenomenon. One study involving 33 patients with Raynaud’s syndrome found that acupuncture serves as a reasonable treatment alternative. In the study, researchers found that patients undergoing acupuncture experienced a significant decrease in the frequency of Raynaud’s attacks, reduced the number of attacks experienced and decreased the duration of reduced blood flow. (19, 20)
6. Avoid “Vasoconstrictive” Medications
If you are using a medication that can lead to reduced blood flow and increase your risk of having a Raynaud’s attack, talk to your doctor about some alternatives. This includes birth control pills, medications used to relieve allergies, diet pills, migraine medications that contain ergotamine, beta blockers that slow your heart rate, some ADHD medications and certain cancer medications. (12)
Raynaud’s Syndrome Key Points
- Raynaud’s syndrome is a rare condition that affects the blood vessels that carry blood from the heart to several parts of the body. When your blood vessels narrow, your blood flow is reduced and this can lead to Raynaud’s attacks.
- Raynaud’s attacks usually affect your fingers and toes. As blood flow to your extremities is reduced, your fingers and toes will likely turn white and then blue. They will also feel cold and numb until blood flow returns. Once blood flow returns to these areas, they will turn red and begin to tingle or burn until the attack is over.
- Cold temperatures, emotional stress and smoking can trigger a Raynaud’s attack. There is no known cause of primary Raynaud’s, but secondary Raynaud’s is believed to be associated with connective tissue diseases, like scleroderma.
6 ways to reduce or prevent Raynaud’s symptoms include:
- Avoiding cold temperatures
- Reducing emotional and physical stress
- Smoking cessation
- Eating an anti-inflammatory diet
- Trying acupuncture
- Avoiding vasoconstrictive medications