This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Cholangitis (+ 7 Natural Ways to Help Manage Cholangitis Symptoms)
June 29, 2018

Moderate-to-severe pain in the right upper quarter of the abdomen may be a sign of cholangitis. Johns Hopkins Medicine’s cholangitis definition is “an inflammation of the bile duct system that is usually related to a bacterial infection.” Symptoms of cholangitis generally range from moderate to severe, and if suspected, you should seek medical attention as soon as possible as this condition can be life-threatening. (1)
Cholangitis is considered relatively uncommon in the United States and is most often associated with other diseases that cause bile duct obstructions. Women are slightly more likely than men to get cholangitis and conventional treatment depends on the cause and the severity of symptoms. (2)
What Is Cholangitis?
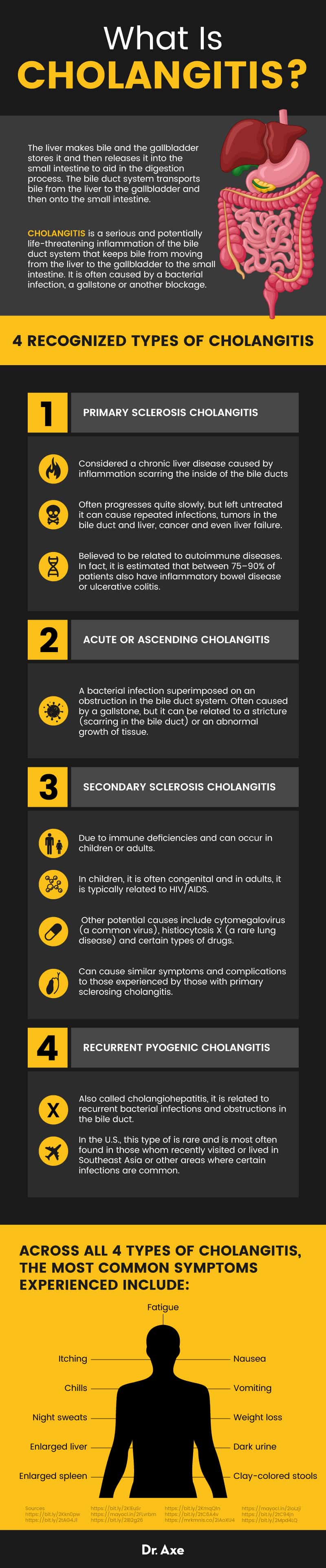
The liver makes bile and the gallbladder stores it and then releases it into the small intestine to aid in the digestion process. The bile duct system transports bile from the liver to the gallbladder and then on to the small intestine. When this system becomes obstructed, an infection is likely and proper treatment is necessary. (3)
Cholangitis is a serious and potentially life-threatening inflammation of the bile duct system that keeps bile from moving from the liver to the gallbladder to the small intestine. It is often caused by a bacterial infection, a gallstone or another blockage. (4)
There are four recognized types of cholangitis:
Primary sclerosis cholangitis
This type of cholangitis is considered a chronic liver disease caused by inflammation scarring the inside of the bile ducts, according to the Mayo Clinic. Primary sclerosing cholangitis often progresses quite slowly, but left untreated it can cause repeated infections, tumors in the bile duct and liver, cancer and even liver failure. (5, 6)
Primary sclerosing cholangitis is believed to be related to autoimmune diseases. In fact, it is estimated that between 75 percent and 90 percent of patients also have inflammatory bowel disease or ulcerative colitis. As the disease progresses, it can cause portal hypertension and cirrhosis of the liver. (7)
Acute or ascending cholangitis
Acute cholangitis is defined as a bacterial infection superimposed on an obstruction in the bile duct system. It is often caused by a gallstone, but it can be related to a stricture (scarring in the bile duct) or an abnormal growth of tissue. (8)
Secondary sclerosis cholangitis
This type of cholangitis is due to immune deficiencies and can occur in children or adults. In children, it is often congenital and in adults, it is typically related to HIV/AIDS. Other potential causes include cytomegalovirus (a common virus), histiocytosis X (a rare lung disease) and certain types of drugs. Secondary sclerosing cholangitis can cause similar symptoms and complications to those experienced by those with primary sclerosing cholangitis. (9, 10)
Recurrent pyogenic cholangitis
Also called cholangiohepatitis, it is related to recurrent bacterial infections and obstructions in the bile duct. In the United States, this type of is rare and is most often found in those whom recently visited or lived in Southeast Asia or other areas where certain infections are common. (11)
Signs and Symptoms
Known as the cholangitis triad, the three most common symptoms are: (12)
- Pain in the upper right quadrant of the abdomen
- Fever
- Jaundice
The Reynolds pentad adds two symptoms to the triad:
- Changes in mental status
- Sepsis
In addition, across all four types of cholangitis, the most common symptoms experienced include: (5, 13)
- Fatigue
- Itching
- Chills
- Night sweats
- Enlarged liver
- Enlarged spleen
- Weight loss
- Dark urine
- Clay-colored stools
- Nausea
- Vomiting
Causes and Risk Factors
Recognized causes of cholangitis include: (14)
- Obstructive tumors
- Pancreatic cancer
- Cholangiocarcinoma, a cancer of the bile ducts (15)
- Ampullary cancer, a rare cancer of the gastrointestinal tract (16)
- Strictures or scars in the bile duct
- Stenosis, an abnormal narrowing of a bile duct
- Common bile duct stones
- Endoscopic manipulation of the central bile duct
- Choledochocele, a cyst in the common bile duct (17)
- Parasitic infestations
- Ischemic bile duct injury
Risk factors for cholangitis include:
Genetics, an 80-fold increased risk of primary sclerosing cholangitis is evident in first degree relatives (18)
- History of gallstones
- HIV
- Congenital bile duct abnormalities
Conventional Treatment
A cholangitis diagnosis requires a variety of tests including: (19)
- Blood tests that check for levels of certain liver enzymes and liver function
- MRIs and X-rays of bile ducts
- Liver tissue samples
There is no cure for any form of cholangitis. Treatments focus on managing symptoms, delaying the progression and fighting bacterial infections. There are currently over 100 clinical trials evaluating new treatments and looking for ways to improve quality of life.
Primary sclerosis cholangitis
Conventional treatment focuses on closely monitoring liver function and managing symptoms. The only known cure for advanced primary sclerosing cholangitis is a liver transplant. However, a small number of patients may have the disease recur even after successful transplantation surgery. (5)
Itching is one of the top complaints for this type of cholangitis. The intense itching is believed to be caused by bile acids. Certain medications called bile acid sequestrates as well as antihistamines, opioid antagonists and ursodeoxycholic acid medications may be prescribed.
For the infection, repeated courses of antibiotics may be necessary.
To treat a blockage, surgical options include balloon dilation and stent placement.
Acute or Ascending Cholangitis
Treatment focuses on eliminating the infection with broad-spectrum antibiotics to prevent sepsis. In severe cases, emergency surgery known as decompression of the biliary tree may be required. (12)
Secondary sclerosis cholangitis
Treating the primary cause of this type is key. However, treatment options are rather limited. Bacterial infections are generally treated with broad-spectrum antibiotics and a variety of surgical procedures may be necessary, including a liver transplant. (20)
Recurrent pyogenic cholangitis
This form of cholangitis must be treated with nutritional rehabilitation, antibiotics and possibly a variety of surgical procedures including hepatectomy (with or without drainage) or a biliodigestive bypass. Close monitoring is vital to be able to quickly identify any potentially serious complications. (21)
Natural Ways to Manage Cholangitis
1. Don’t drink alcohol
Alcohol is hard on the liver, and it can cause liver disease. Because of this, when you have any type of liver disease, avoiding alcohol is recommended. (19, 22)
2. Exercise
Regular exercise can help your body expel toxins. When your liver and bile duct system isn’t working properly, it is imperative to exercise every day. The Mayo Clinic indicates that walking 30 minutes each day can help reduce symptoms. (19)
In a small clinical trial published in the World Journal of Transplantation, physical exercise in those with liver disease is associated with increased muscle strength, improved functional capacity and better quality of life. Low-impact exercises like swimming, Pilates and strength training may help you cope with cholangitis symptoms. (23)
3. Manage stress
Every chronic illness causes stress and impacts your overall quality of life. Learning to manage stress is imperative for your health. Chronic stress is associated with increasing your risk of heart attack, stroke, digestive disorders, pain and addiction.
The Mayo Clinic recommends using a variety of stress management techniques, including meditation, relaxation exercises and yoga. Other ideas to help you manage stress include music therapy, art therapy, journaling and spending quality time with those you love. (19)
4. Take milk thistle
One of the most effective and popular natural supplements for liver health, milk thistle helps to draw toxins out of the body. Historically, this herb has been used in the treatment of several liver diseases including alcoholic liver disease, acute and chronic viral hepatitis and toxin-induced liver diseases. (24)
It is also associated with preventing gallstones and may protect against certain types of cancer. As a liver detoxing agent, taking 150 milligrams of milk thistle one to three times a day is generally recommended. To support ongoing liver health, taking between 50 and 150 milligrams daily is recommended. (25)
5. Include probiotics in your diet
Taking a high-quality probiotic supplement with liver disease is vital and most studies show that taking at least 500 million CFU daily for three months, or 12 billion CFU daily for eight days, is associated with improved liver function. (26)
And, in the treatment of primary sclerosis cholangitis with IBS, probiotics can be beneficial. There is also evidence that the use of prebiotics and probiotics reduce bacterial infection rates in those with liver transplantation. (27)
In addition to taking a high-quality probiotic supplement, preferably from soil-based organisms, adding probiotic-rich foods like sauerkraut, yogurt, and kombucha is imperative. With cholangitis, antibiotic use kills off not only the bad bacteria but the healthy bacteria in your gut that helps you properly digest foods. (28)
6. Reduce toxin exposure
As the liver is responsible for removing toxins from our system, when you have liver disease, including chronic cholangitis, it is important to try to reduce your exposure to toxins. Reducing toxins also means to quit smoking, avoid second-hand smoke and avoid other drugs.
Eating organic foods and using natural cleaners without harsh chemicals is recommended. The cleaner your diet, the better. Avoid processed foods and any foods that you have a sensitivity to. If you also have inflammatory bowel disease, like most with cholangitis, following an IBS diet plan is recommended.
7. Try curcumin
The Mayo Clinic is currently studying whether curcumin is a safe and effective cholangitis treatment for primary sclerosing cholangitis. In the small clinical trial, participants are taking 750 milligrams of curcumin twice a day for 12 weeks to determine its efficacy in reducing certain liver disease markers as well as quality of life factors and fatigue. Results of this study are expected summer 2018. (29)
Final Thoughts
- Cholangitis is a serious and chronic liver disease where an infection occurs in the bile duct.
- The cholangitis triad is three most common symptoms: pain in the upper right quadrant of the abdomen, fever and jaundice.
- Genetics is the top risk factor with nearly estimated 80 percent of first-relation family members getting the disease.
- There is no cure; treatment focuses on killing the infections and managing symptoms.
- A liver transplant may be necessary as the disease progresses, but for some patients, the disease will return.
Read Next: How to Improve Liver Function in 6 Steps













