This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
4 Natural Remedies for Colon Polyps Symptoms
September 17, 2018
Colorectal cancer — now the second most common cause of cancer death in the U.S. — usually begins as a “polyp,” which is why another name for colon polyps is “colorectal polyps.” The type of colon polyp called an adenoma is a known precursor of colorectal cancer. While in some cases small colon polyps will develop into colon cancer over time, most colon polyps remain small, are non-cancerous and are generally harmless.
How common is it to have polyps in the colon? Polyps are considered “very common” in adults over the age of 60, who have about a 25 to 30 percent chance of having a polyp. However they are much less common among younger adults, such as those in their 20s or 30s. (1)
Doctors highly encourage adults over the age of 50 to visit their doctors for regular colorectal screenings, since finding a colon polyp in its earliest stages greatly limits the chances of complications. Certain lifestyle changes can also help to reduce your risk of developing colon polyps and colorectal cancer, or to support recovery — including eating an anti-inflammatory diet, quitting smoking, exercising, getting enough calcium and vitamin D, and maintaining a healthy weight.
What Are Colon Polyps?
A colon polyp (or colorectal polyp) is an extra piece of tissue, or a small clump of cells, that grows on the lining of the colon. (2) Colorectal polyps can grow in any part of the colon — also known as the large bowel or large intestine, which solid waste moves through before leaving the body — usually forming on the left side of the colon and/or in the rectum. (3) The rectum, where feces is stored before being excreted, begins at the end of the large intestine and ends at the anus.
Types of Colon Polyps:
There are two main types of colon polyps: non-neoplastic polyps and neoplastic polyps (which include adenomas/tubular adenomas). (4)
- Non-neoplastic colon polyps usually do not become cancerous. These include hyperplastic polyps, inflammatory polyps and hamartomatous polyps.
- Neoplastic polyps are more likely to become cancerous, although they don’t always. These include adenomas and serrated types.
- Neoplastic polys are typically larger. Determining colon polyp size is an important part of diagnosis because larger polyps pose a greater risk of causing cancer.
An adenoma (a type of neoplastic polyp) is a tumor of glandular tissue. According to the American Cancer Society, “An adenoma is a polyp made up of tissue that looks much like the normal lining of your colon, although it is different in several important ways when it is looked at under the microscope.” (5) It’s estimated that two-thirds of colon polyps are the precancerous type called adenomas, and that only about 5 percent of adenomas progress to cancer. (6)
Adenoma polyps are not a type of cancer, but they are considered pre-cancerous (meaning that they can turn into cancers). However, most patients with adenoma polyps will never develop colon cancer.
Adenomas can have several different growth patterns, including: tubular and villous, or a mixture of both (called tubulovillous adenomas). Most are tubular adenomas that are small (less than one-half inch), while some are larger adenomas with a villous growth pattern that are more likely to have cancers develop in them.
When viewed under a microscope, polyps that are only mildly abnormal are said to have low-grade (mild or moderate) dysplasia, while polyps that are more abnormal and look more like cancer are said to have high-grade (severe) dysplasia.
Symptoms and Signs
Not everyone with colon polyps will be aware that they have them; in fact, most of the time colon polyps don’t cause any noticeable symptoms.
When they do occur, the most common colon polyps symptoms include: (8)
- Rectal bleeding (which can also be caused by other conditions, not polyps, including hemorrhoids, or tiny tears in the tissue of the anus). You may notice blood on your underwear or on toilet paper after a bowel movement.
- Blood in your stool or other changes in your poop color, such as dark red streaks or black stools.
- Stomach pain, abdominal cramping and aching/tenderness near the bowels. Large colon polyps are more likely to cause pain because they may partially obstruct your bowel.
- Constipation or diarrhea.
- Developing anemia due to iron deficiency and prolonged bleeding. Bleeding from polyps can deplete your body of iron, making it difficult to produce red blood cells and carry oxygen throughout your body, leading to symptoms like fatigue, weakness and shortness of breath.
Causes and Risk Factors
Colon polyps develop when cells grow and divide in an abnormal way inside the colon or rectum, leading to a growth that may become big enough to obstruct the bowel. This can happen to due inflammation of the large intestine, or mutations in certain genes that cause cells to continue dividing when they normally wouldn’t.
Research suggests that colon polyps causes and risk factors that can increase your chances of developing colon polyps include: (9)
- Being over the age of 50.
- Being male. Studies indicate that men are more likely to have colonic neoplasms and twice as likely to have advanced lesions compared to women. Advanced neoplasia polyps affect about 2.9 percent of women in their 50s compared with 4.7 percent of men of the same age.
- Having a personal or family history of colon polyps or colon cancer.
- Suffering from leaky gut syndrome (aka intestinal permeability) or inflammatory gastrointestinal issues or inflammatory bowel disease (IBD), including ulcerative colitis or Crohn’s disease.
- Metabolic syndrome and having type 2 diabetes. Individuals with type II diabetes have a 3-fold increase in colon cancer compared with nondiabetic individuals.
- Obesity or being overweight. Studies conducted in Germany, Japan and the U.S. have found a two- to three-fold increased incidence of colorectal neoplasms in overweight individuals.
- Suffering from chronic inflammation, including having high circulating levels of glucose and lipids that create an oxidative environment.
- Having high serum IGF-I (insulin like growth factor) concentrations than the general public.
- Being a smoker.
- High alcohol consumption.
- Lack of exercise/a sedentary lifestyle.
- Having a rare hereditary disorder that affects the intestines and can cause colon polyps to form, including: Lynch Syndrome (aka hereditary nonpolyposis colorectal cancer), Familial Adenomatous Polyposis (FAP), Gardner’s Syndrome, MYH-Associated Polyposis (MAP), Peutz-Jeghers Syndrome or Serrated Polyposis Syndrome.
- Being African-American (African-American are also at higher risk of developing colon cancer).
- Being deficient in calcium and/or suffering from vitamin D deficiency.
Diagnosis
You should visit your doctor if you start noticing new symptoms like abdominal pain, bloody stools and unexplained changes in your bowel habits — especially if you’re at an increased risk of developing polyps or colorectal cancer (for example if you have a family history of colon cancer).
Because you can have colon polyps and not experience any symptoms at all, it’s important to have regular screening tests after the age of 50, such as a colonoscopy. Polyps are least likely to develop into cancer or cause other problems if they are removed when they are small and their in early stages. A study called The National Polyp Study found that colonoscopic surveillance was associated with a 76 to 90 percent reduction in cancer incidence. (10)
Screening tests used to diagnose colon polys include: (11)
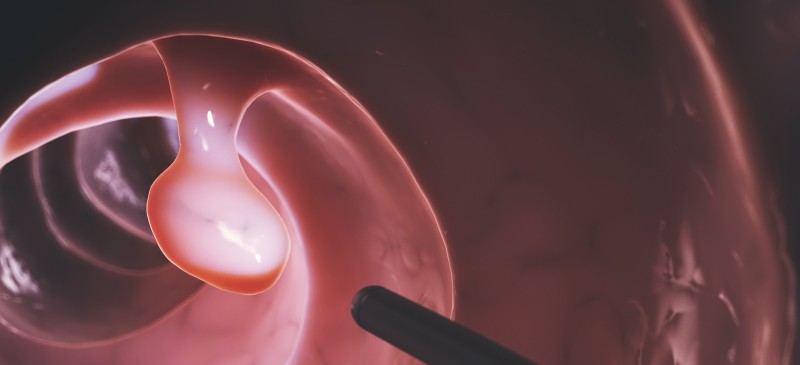
- Colonoscopy or virtual colonoscopy, a minimally invasive test that uses a CT scan to view the inside of your colon. A colonoscopy is an outpatient test in which a long, thin flexible tube with a camera and a light on the end are inserted into the colon.
- Flexible sigmoidoscopy, when a tube is inserted in your rectum to examine the last third of your large intestine.
- Stool-based tests to look for blood.
If your doctor finds a colon polyp during a screening exam (an examination of your bowel), he/she will discuss whether the poly may be cancerous or pre-cancerous.
Are large colon polyps usually cancerous? When it comes to colon polyp size, the larger a polyp is, the more likely it is to be cancerous. This is especially true of especially with neoplastic polyps, including adenomas and serrated types (which look flat under a microscope). But to reiterate, having an adenoma does not mean you will definitely develop cancer.
How long does it take for a colon polyp to turn into cancer? It’s believed that it may take around 10 years for a small adenoma to transform into a cancerous polyp. (9) Because cancer can take a long time to form, this is why it’s so helpful to screen early and remove polyps before it’s too late.

Conventional Treatment
To help prevent cancer from potentially forming, doctors commonly remove colon polyps and test them. It’s most important to have a colonoscopy performed if in the past you’ve: had one or more adenomas within the previous 5 years, you’ve had more than two adenomas measuring 0.4 inches (about 1 centimeter) or larger, you’ve had more than 10 adenomas, or you’ve had a very large adenoma that was recently removed.
Colon polyps treatment typically includes:
- Removal of adenoma polyps. If an adenoma is found during a colonoscopy, it is usually removed and biopsied to check for cancer. Polyps can be removed in several ways, such as witha wire loop (polypectomy) or a liquid that is injected into the tissue surrounding the polyp to make it separate. A laparoscopy can also be performed by inserting an instrument called a laparoscope into the bowel.
- Surgery to remove a large adenoma. When an adenoma becomes too large to remove during colonoscopy, surgery may be needed to have the adenoma removed.
Unfortunately, it’s common for polyps that have been removed to come back. Around 30 percent of patients will develop new polyps after removal, which is why follow-up tests are recommended over the next 3–5 years. There’s some evidence that taking a daily aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) may reduce the risk of new polyps forming, but this is not a guarantee and may contribute to side effects.
4 Natural Remedies for Symptoms of Colon Polyps
1. Eating a Healthy, Anti-Inflammatory Diet
Prior to having screening tests done to look for colon polyps (including a colonoscopy), it’s recommended that you eat a low-fiber diet for four to five days to reduce the chances that fiber will remain in your colon wall and block the doctor’s view.
What type of diet is best if you’ve been diagnosed with colon polyps? A healing diet that includes plenty of antioxidants, fiber and essential nutrients helps to protect the large intestine and may be beneficial for fighting cancer.
- Include plenty of fruits and vegetables in your diet. Some of the best for protecting against cancer include: cruciferous veggies like broccoli and cauliflower, leafy greens like kale and spinach, sea vegetables, berries, citrus fruits, mushrooms, carrots, beets, tomatoes and bell peppers.
- Incorporate other nutrient-dense and cancer-fighting foods into your diet such as: fresh herbs and spices like turmeric, ginger, basil, parsley or oregano, herbal infusions, fresh green juices, green tea, matcha tea, cocoa powder, organic, grass-fed and/or pasture-raised meats, wild-caught fish like salmon, mackerel, sardines or herring, olive and coconut oil, nuts, seeds and raw garlic.
- Reduce consumption of added sugar, refined grains, foods with additives and preservatives, and alcohol. Have no more than two alcoholic drinks a day if you’re a man, or one drink a day if you’re a woman.
- Eventually, increase your fiber intake. Replace processed grains with 100 percent whole grains like quinoa, brown rice, buckwheat and rolled oats. Other high-fiber foods to have often include: avocados, berries, apples and pears, coconut flakes, figs and dates, artichokes, winter or acorn squash, Brussels sprouts, sweet potatoes, beans and legumes, flax seeds and chia seeds.
- Increase your consumption of calcium (from foods, not supplements), which studies suggest can help prevent recurrence of colon adenomas. Foods high in calcium include: raw milk, yogurt, kefir, fermented cheeses, kale, sardines, broccoli, okra, kale beans and almonds.
- Consider having more plant-based meals and eating less meat, especially processed meat like hot dogs, cold cuts, cured meats like salami, deli meats, etc. Some studies have found that people who eat diets high in meat (especially processed meat and red meat) have higher rates of colon cancer.
2. Alleviating Vitamin D Deficiency
Research has shown that vitamin D may be protective against colorectal cancer and is supportive of immune function in general. For example, a 2014 study published in the World Journal of Gastrointestinal Oncology states that “several studies confirmed that increasing vitamin D3 lowers colon cancer incidence, reduces polyp recurrence, and that sufficient levels of vitamin D3 are associated with better overall survival of colon cancer patients.” (12)
In the past, if you were at an increased risk for colon polyps, your doctor might recommend taking 1,000 milligrams per day of calcium supplements for help with cancer prevention, depending on your age. However, recent studies suggest that calcium supplements and vitamin D supplements may actually raise your risk of colon polyps. (13)
Studies investigating the effects of calcium and vitamin D supplements on polyp prevention have yielded inconsistent results overall. Recently, a randomized clinical trial tested the use of calcium and vitamin D supplements over the course of 10 years in preventing colorectal polyps. Findings showed that 6–10 years after the start of supplementation, participants had a higher incidence of serrated polyps if they took calcium, either on its own or with vitamin D. However, no such link was found for vitamin D taken on its own.
Given this recent finding, it’s now suggested that adults who have, or have ever had, precancerous serrated polyps — particularly women and those who smoke — should avoid taking calcium and vitamin D supplements.
A better way to prevent vitamin D deficiency is by encouraging your body to naturally make its own vitamin D, which happens when you expose your skin to sunlight for about 15–20 minutes. If you live in a cold climate or don’t spend much time outdoors, discuss with your doctor whether you should be supplementing.
3. Staying Active and Maintaining a Healthy Weight
Stay physically active and getting regular exercise not only has helps you to maintain a healthy body weight, but also has anti-inflammatory effects.
Exercise may even be protective against colon polyps and colorectal cancer due to mechanisms like: reducing inflammation, improving circulation, supporting the immune system, improving digestive function, reducing stress, and helping to prevent diabetes and obesity. Certain studies have even found that getting regular exercise may reduce your colon cancer risk by a whopping 40 percent to 50 percent! (14)
A sedentary lifestyle and being overweight or obese have been linked to higher risk for colon and rectal cancer, so find some type of exercise that you enjoy and can stay consistent with — whether it’s waking, jogging, swimming, cycling, weight lifting, etc. You can work towards losing weight or maintaining a healthy weight by eating an anti-inflammatory diet, managing stress, getting enough sleep and regularly exercising.
4. Reducing Chronic Inflammation
Inflammation of the bowel, which may or may not lead to inflammatory bowel disease (IBD), can increase your risk for polyps and growths that may become cancerous over time. Some steps you can take to reduce inflammation and improve digestive health include:
- Eating a therapeutic diet. You may need to work with a dietician/functional medicine doctor if you have IBD in order to help heal your condition with a specific type of diet.
- Managing stress and getting enough rest and sleep (7-9 hours per night for most adults).
- Quitting smoking and drinking excessive alcohol.
- Taking supplements, such as vitamin D, probiotics and omega-3 fish oil supplements.
- Preventing nutrient deficiencies, such as in calcium.
- Eliminating certain foods if necessary, such as: gluten, dairy, some FODMAPs, caffeine and alcohol.
To help control inflammation. your physician might recommend that you start taking aspirin daily to reduce your overall colon cancer risk. There have been mixed findings about how effective aspirin is in the situation. Talk to your doctor about the risks and benefits of using aspirin or an NSAID drug for added protection against colon conditions.
How to Prevent Colon Polyps
How do you prevent polyps in the colon from forming? While preventing them isn’t always possible, below are ways that research suggests you can help reduce your risk for colon polyps:
- Quit smoking. For help quitting smoking, talk to your doctor about useful interventions; speak with a therapist; or start an online program that specializes in smoking cessation.
- Eat an anti-inflammatory diet that includes plenty of vegetables, fiber and high-antioxidant foods.
- Treat calcium and vitamin D deficiency by eating calcium-rich foods and exposing your skin to sunlight.
- Avoid excessive alcohol consumption.
- Limit the amount of processed meat and red meat you consume.
- Take steps to maintain a healthy weight, such as by eating well, staying active, exercising and practicing mindful eating.
- Talk to your doctor about preventative options and genetic screening tests if you have a family history of colon polyps or a hereditary disorder that causes colon polyps.
Final Thoughts
- A colon polyp (or colorectal polyp) is an extra piece of tissue, or a small clump of cells, that grows on the lining of the colon.
- The type of colon polyp called an adenoma is a known precursor of colorectal cancer, however, most colon polyps remain small, are non-cancerous and are generally harmless.
- Many people don’t experience any noticeable colon polyp symptoms, but when they do occur, they can include: rectal bleeding, bloody stools, abdominal pain, constipation and diarrhea.
- Risk factors for colon polyps include: having a family history of personal history of polyps and/or colorectal cancer, being male, being over 50, smoking, being overweight or obese, having inflammatory bowel disease, experiencing chronic inflammation, and being African-American.
- Four natural remedies for symptoms of colon polyps include eating an anti-inflammatory diet, alleviating vitamin D deficiency, staying active and maintaining a healthy weight as well as reducing chronic inflammation.



