This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
How to Maintain Normal Blood Sugar
October 17, 2023

If you are one of the millions of people who has prediabetes, diabetes, metabolic syndrome or any other form of “insulin resistance,” maintaining normal blood sugar levels can be challenging. Over the past several decades, these chronic disorders have swept through the U.S. and many other nations, reaching epidemic proportions and causing serious, but often preventable, side effects like nerve damage, fatigue, loss of vision, arterial damage and weight gain.
Elevated blood sugar levels maintained for an extended period of time can push someone who is “prediabetic” into having full-blown diabetes (which now affects about one in every three adults in the U.S.). Even for people who aren’t necessarily at a high risk for developing diabetes or heart complications, poorly managed blood sugar can lead to common complications, including fatigue, weight gain and sugar cravings. In extreme cases, elevated blood sugar can even contribute to strokes, amputations, coma and death in people with a history of insulin resistance.
Blood sugar is raised by glucose, which is the sugar we get from eating many different types of foods that contain carbohydrates. Although we usually think of normal blood sugar as being strictly reliant upon how many carbohydrates and added sugar someone eats, other factors also play a role. For example, stress can elevate cortisol levels, which interferes with how insulin is used, and the timing of meals can also affect how the body manages blood sugar.
What can you do to help avoid dangerous blood sugar swings and lower diabetes symptoms? As you’ll learn, normal blood sugar levels are sustained through a combination of eating a balanced, low-processed diet, getting regular exercise and managing the body’s most important hormones in other ways (such as getting enough sleep and reducing stress).
The power is within your hands, since many of the disorders triggered by poorly managed blood sugar are avoidable and can be managed naturally and successfully through practicing certain healthy habits.
What Is Normal Blood Sugar?
What doctors consider to be “normal” blood sugar depends on your medical history (such as if you have or ever had diabetes) and when the last times you ate something and exercised were. Blood sugar is measured in terms of milligrams of sugar per dL of blood, and measurements are most often taken in the morning after you’ve been fasting through the night.
The following blood sugar measurements are considered healthy and normal according to health authorities, including the American Diabetes Association:
- If you’re generally healthy (you don’t have diabetes) and you haven’t eaten anything in the past eight hours (you’ve been “fasting”), it’s normal for blood sugar to be anything between 70–99 mg/dL (less than 100 mg/dL).
- If you’re healthy and you’ve eaten within the past two hours, it’s normal for blood sugar to be anything less than 140 mg/dL.
- If you do have a history of diabetes, fasting glucose should ideally also be below 100 mg/DL, which might need to be managed through the use of insulin. It’s also considered healthy to have levels between 70–130 prior to eating.
- If you have diabetes and you’ve eaten in the past two hours, the goal is to have blood sugar below 180 mg/dL.
- If you have diabetes, you want to keep blood sugar between 100–140 mg/dL prior to bedtime and at least 100 mg/dL prior to exercising.
Signs of High/Low Blood Sugar
Even without measuring your blood sugar levels, there are certain clues that things might not be “normal.” How do you know if you’re not successfully managing your blood sugar levels throughout the day?
Common signs and symptoms not to ignore that can signify diabetes and fluctuating blood sugar levels include:
- Fatigue or chronic fatigue syndrome, low energy levels
- Sugar/carb cravings
- Excessive thirst
- Weight fluctuations/weight loss
- Increased urination
- Mood swings, nervousness or “jitteriness”
- Blurred, worsening vision
- Slow healing of skin wounds, dryness, cuts and bruises
- Frequent infections
- Heavy breathing and trouble exercising
- Tension headaches
Causes of Abnormal Blood Sugar Levels
People who tend to experience fluctuating, “abnormal” blood sugar levels include:
- anyone with prediabetes or diabetes
- those eating a poor diet, high in sugar, refined grains, artificial ingredients and packaged foods
- people who skip meals, don’t eat enough or who fad diet
- anyone who doesn’t eat around the time of exercising, before or after workouts, to help refuel
- people who don’t get enough sleep and live with high amounts of chronic stress
- pregnant women (who can be at risk for gestational diabetes)
- people with a history of insulin resistance/diabetes in their families
Your diet is the single most influential factor when it comes to your blood sugar levels. The foods that we eat fall into one of three categories: carbohydrates (sugars and starches), proteins and fats.
Fats don’t affect blood sugar, while carbohydrates — and to a small extend proteins — do. Carbohydrates in our diets along with a portion of the protein we eat are turned into glucose, which is what gives cells most of their energy and helps fuel the majority of the body’s many functions.
Glucose requires insulin in order to be brought into cells, which is the hormone secreted by the pancreas that’s most important for blood sugar control. When we eat carbohydrates or proteins, blood sugar rises, which alerts the body to produce more insulin in order to bring levels back to normal by ushering sugar to cells. Insulin levels rise and fall in accordance with our diets and are also impacted by levels of other hormones, such as cortisol.
In people who have diabetes (whether type 1 or type 2), cells stop responding to insulin the way they should and the process described above starts to break down. Either not enough insulin is being produced by the pancreas or cells are no longer responding to normal amounts of insulin (called “insulin resistance). This is when a lifestyle and diet to manage diabetes become especially important.
Problems maintaining normal blood sugar can arise when:
- Insulin-releasing mechanisms no longer work as they should — specifically beta cells within the pancreas stop reacting to changes in blood sugar normally and too little insulin is produced, leaving blood sugar elevated.
- When blood sugar levels aren’t managed, hyperglycemia and hypoglycemia can then occur as levels rise and fall drastically. These comes with many side effects that are indicative of prediabetes or diabetes, including fatigue, sugar cravings, changes in blood pressure, weight loss or gain, nerve damage, and nervousness.
- Cells stop receiving enough energy since insulin is no longer doing its job of bringing them enough glucose (sugar). At the same time, blood glucose levels can remain elevated, which damages the kidneys, heart, arteries and nerves — which in turn affects the whole body negatively.
How to Maintain Normal Blood Sugar
Most of the habits that help us maintain healthy, normal blood sugar levels are fairly obvious and simple to carry out. However, some might also surprise you, especially if you think it will be tough to start managing your blood sugar better.
Small changes in your diet, exercise routine and sleep schedule can wind up making a big difference when it comes to blood sugar management. Let’s look at some of the best ways to help get you on the right track to reaching and maintaining normal blood sugar levels for life.
1. Eat a Low-Processed, Anti-Inflammatory Diet
A healthy diet is key to blood sugar management and preventing or treating diabetes. It’s not that you must avoid consuming any carbohydrates or sugar when trying to maintain normal blood sugar — just that you need to balance them out with protein/fats, and focus on getting them from real, whole foods.
Eating a source of protein, fiber and healthy fat with all of your meals can help stabilize blood sugar, especially when you consume carbs/sugar (such as starchy veggies like potatoes, fruit or whole grains). These slow down the absorption of sugar into the bloodstream, help manage your appetite, and are also important for your metabolism and digestion.
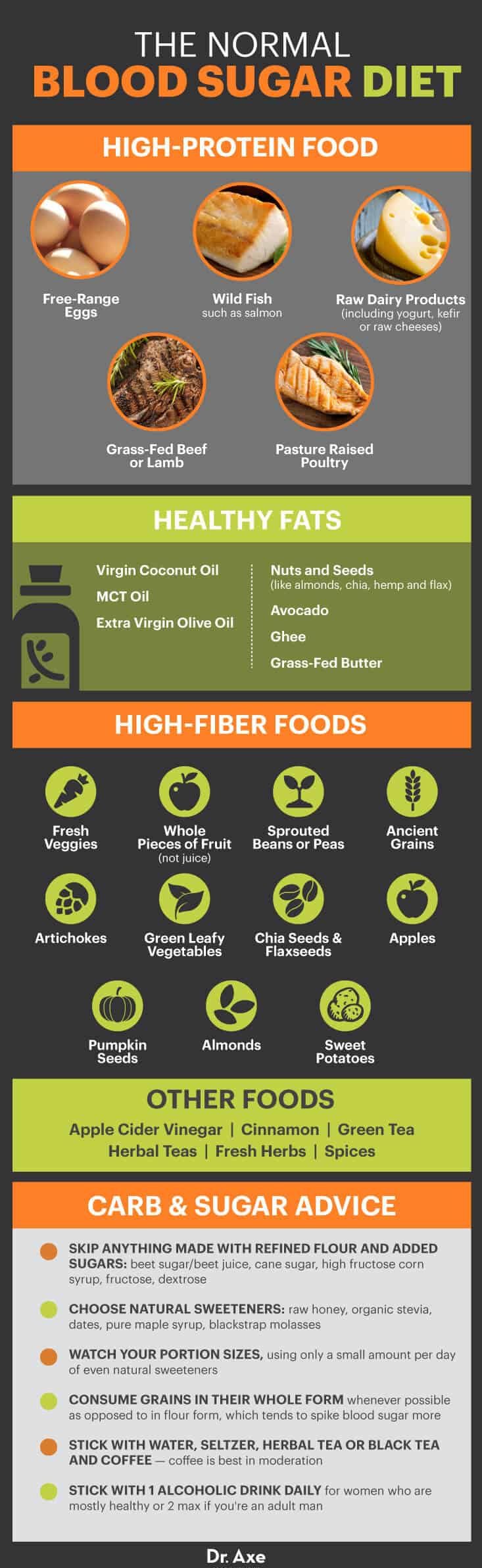
- Some of the best protein foods for managing blood sugar include: wild fish such as salmon, free-range eggs, grass-fed beef or lamb, raw dairy products (including yogurt, kefir or raw cheeses), and pasture-raised poultry
- Healthy fats include: virgin coconut oil, MCT oil, extra virgin olive oil, nuts and seeds (like almonds, chia, hemp and flax), and avocado. Coconut oil, ghee and grass-fed butter are all some of my favorite fat-burning foods for managing blood glucose levels while also improving the taste and filling quality of your meals.
- High-fiber foods include: fresh veggies, whole pieces of fruit (not juice), sprouted beans or peas, and ancient grains. Some of my favorite foods especially high in fiber are artichokes, green leafy vegetables, chia seeds, flaxseeds, apples, pumpkin seeds, almonds, avocado and sweet potatoes.
- Consider the supplement berberine to control blood sugar and lipid metabolism as effectively as metformin, with researchers describing it as a “potent oral hypoglycemic agent.” A study published in the World Journal of Cardiology demonstrated that red yeast rice extract may also help with healthy maintenance of normal blood sugar levels. This study specifically looked at the effects of a supplement containing berberine, red yeast rice and policosanol.
- Other foods and drinks that make great additions to a blood-sugar-stabilizing diet include apple cider vinegar, cinnamon, green tea, herbal teas, fresh herbs and spices.
2. Switch Up Your Carbs and Sweeteners
While all types of added sugars are capable of raising blood sugar levels, some sources of sugar/carbs affect blood glucose levels more so than others. When you use appropriate amounts sparingly, natural/unrefined, ideally organic sugar sources (such as those from fruit or raw honey) are less likely to contribute to poor blood sugar management than refined sugars (such as white cane sugar or refined products made with white/bleached wheat flour).
To help sustain normal blood sugar, check ingredient labels carefully, since sugar can be listed under dozens of different names.
- Skip anything made with refined flour (also called wheat flour or “enriched flour”) and added sugars, such as beet sugar/beet juice, cane sugar, high fructose corn syrup, fructose and dextrose.
- Instead choose natural sweeteners, including raw honey, organic stevia, dates, pure maple syrup or blackstrap molasses.
- Most importantly, still watch your portion sizes, using only a small amount per day of even natural sweeteners (such as one to three teaspoons daily).
- When it comes to grain-flour products, it’s best to consume grains in their whole form whenever possible as opposed to in flour form, which tends to spike blood sugar more. But if you must use flour, choose those made with 100 percent whole grains, or else try coconut flour or almond flour for an even healthier option.
- In terms of beverages, stick with water, seltzer, herbal tea or black tea, and coffee. Coffee is best in moderation, meaning one to two cups daily, especially compared to sweetened drinks, juices or soda.
- Keep in mind that alcohol can also raise blood sugar, especially if you consume sweetened alcoholic drinks (such as certain dessert/fortified wines, sherries, liqueurs, mixed drinks with juice and ciders).
3. Get Regular Exercise
You’re probably already aware that there are literally dozens of benefits associated with exercise. According to the National Diabetes Association, exercise manages blood sugar in more than one way. Short-term exercise helps cells in your muscles to take up more glucose in order to use it for energy and tissue repair, therefore lowering blood sugar in the process. Long-term exercise also makes cells more responsive to insulin and helps prevent resistance.
Doing about 30–60 minutes of exercise most days of the week (such as running, cycling, swimming and lifting weights) is also a simple, beneficial way to lower inflammation, manage stress, improve immunity and balance hormones. Insulin sensitivity is increased, so your cells are better able to use any available insulin to take up glucose during and after activity.
4. Manage Stress
Excessive stress can actually cause blood sugar levels to rise due to an increased release of the “stress hormone” cortisol. Stress kicks off a vicious hormonal cycle for many people. It not only contributes to high blood sugar by raising cortisol, but also tends to increase cravings for “comfort foods” (many of which are refined and filled with sugar or other inflammatory ingredients) and often interferes with getting good sleep.
All around, dealing with high amounts of stress makes it less likely that people will take good care of themselves and keep up with healthy habits that contribute to normal blood sugar. For example, skipping workouts and drinking more alcohol and caffeine are both common among chronically stressed adults.
These self-destructive habits contribute to even more stress, which interferes with blood sugar management even more. It’s no wonder that people who develop health problems like diabetes or heart disease, or even who wind up gaining a lot of weight and facing obesity, tend to feel more depressed and hopeless but find it hard to break the cycle and develop new habits.
What are some ways you can help deal with the inevitable stresses that occur in life? Studies have found that natural stress relievers, including exercise, yoga, meditation and using relaxing essential oils for anxiety (such as lavender, rose and frankincense) are all helpful for diabetics and those with insulin resistance.
Other ways to wind down include spending more time outdoors, joining groups in your community, and connecting with family and friends more.
5. Get Enough Rest
Being well-rested is crucial for maintaining a healthy outlook on life, sticking with healthy habits and even managing hormone levels.
A lack of sleep can raise stress and appetite hormones (like cortisol and ghrelin, which make you hungry), making it harder to void sugary snacks, refined grain products and caffeine overdose.
Sleep and metabolic processes are linked in several key ways, and research shows our natural circadian rhythms can trigger high blood glucose or raise the risk for diabetes when they’re disturbed. Sleeping too little, getting poor quality sleep or sleeping at the wrong times can impair insulin secretion even if you don’t change your diet.
Aim to get between seven to nine hours of sleep per night, ideally by sticking with a normal sleep/wake schedule — in order to balance hormones, curb stress responses, and have enough energy to exercise and keep up with your day.
Final Thoughts
- Elevated blood sugar levels maintained for an extended period of time can push someone who is “prediabetic” into having full-blown diabetes (which now affects about one in every three adults in the U.S.).
- People who tend to experience fluctuating, “abnormal” blood sugar levels include anyone with prediabetes or diabetes; those eating a poor diet, high in sugar, refined grains, artificial ingredients and packaged foods; people who skip meals, don’t eat enough or who fad diet; anyone who doesn’t eat around the time of exercising, before or after workouts, to help refuel; people who don’t get enough sleep and live with high amounts of chronic stress; pregnant women (who can be at risk for gestational diabetes); and people with a history of insulin resistance/diabetes in their families.
- Signs of high/low blood sugar include fatigue and low energy levels; sugar/carb cravings; excessive thirst; weight fluctuations/weight loss; increased urination; mood swings, nervousness or jitteriness; blurred, worsening vision; slow healing of skin wounds, dryness, cuts and bruises; frequent infections; heavy breathing and trouble exercising; and tension headaches.
- In order to achieve normal blood sugar levels and maintain them, eat a low-processed, anti-inflammatory diet that includes protein foods, healthy fats and high-fiber foods; switch up your carbs and sweeteners, avoiding refined flour and utilizing natural sweeteners in moderation; get regular exercise; manage stress; and get enough rest.
