This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Thermography: Breast Cancer Detection + Better Risk Assessment
March 7, 2019
What is thermography? Thermography is a state-of-the-art, and potentially life-saving, method of detecting cancer by using thermal imaging. The technology used to perform thermograms is considered one of the most reliable for risk assessment and detection, especially in the case of breast cancer — as opposed to potentially cancer-causing mammograms.
The Breast Thermography website calls the thermography procedure “one of the most important adjunctive breast imaging procedures available today.” (1)
A Key Tool in Risk Assessment
Early detection of breast cancer is one of the keys to significantly improving survival rates; in fact, it’s estimated that up to 95 percent of breast cancer cases can be overcome when the cancer is detected in its earliest stages.
Every year, more than 70,000 adult men and women between the ages of 15 and 39 are diagnosed with cancer in the U.S., with breast cancer being the most common, and also most deadly, type in women in this age group. (2) Today, doctors don’t typically order mammograms for women under the age of 40, and because up to 75 percent of women who get breast cancer have no family history of the disease, detection often comes late.
Over the past 20 years, thermography (also sometimes called infrared thermography, or IRT) has come a very long way, and today doctors rely on using ultra-sensitive, high-resolution digital infrared cameras to track thermal (heat) patterns throughout patients’ bodies. Thermography is performed as a 15-minute non-invasive test — there is no compression, radiation or contact involved, explains explains Dr. Alexander Mostovoy, DHMS, BCCT, of the Thermography Clinic Inc.
Doctors can also perform full-body imaging scans using thermography to predict if any areas of the body show signs of abnormality or inflammation. If thermography results appear abnormal, a patient’s doctor is alerted to changes that could indicate early stages of disease development that could lead to cancer. If a disease like breast cancer is suspected and later confirmed, a doctor can continue closely monitoring the patient’s progress and come up with the best cancer treatment plan to combat the disease before it’s able to progress.
How Thermography Works
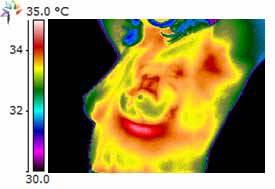
Photo: Thermography Clinic Inc.
Thermographic cameras work by detecting heat that naturally emits from the body. Results of thermal imaging tests are known as thermograms.
Infrared thermography is the technique of converting infrared energy (radiant heat) into an image that can be seen. All substances in the universe give off some heat in the form of radiation naturally, and the amount of radiation emitted increases with temperature. (3)
In other words, infrared energy emitted from an object is directly proportional to its temperature. Thermography tests can track variations in body temperature from one person to another, and also to track changes in the same person’s surface temperature over time. But it’s important to point out that heat radiating from the body is not the same thing as dealing with radiation therapy.
While it’s been researched most extensively for its role in detecting breast cancer, the benefits of thermography can also be applied to the rest of the body. Other than helping to provide risk assessment relating to breast cancer, thermography imaging is used to track changes in women with fibrocystic conditions, infections, allergies and even cardiovascular diseases that affect the arteries. (4) Thermal imaging cameras are even used in airports to detect illnesses (like the swine flu) or concealed weapons, by firefighters to detect smoke and find trapped civilians, and utilized by the military as part of surveillance protocols.
The primary reason that thermography tests are so beneficial is that they offer an earlier, more reliable way to detect abnormal cellular activities and suspected tumor growths compared to other tests like self-examinations.
Thermography imaging tests are both precise and sensitive, picking up on even subtle changes in the body that can signify a lurking problem. They are also inexpensive and don’t require any exposure to radiation or invasive procedures, limiting barriers to testing.
Key Facts About Thermograms:
- Thermal vision tests are designed to detect fast-growing, active tumors. The tests demonstrate heat patterns that can be strongly indicative of abnormalities, including those associated with breast cancer. They can also be used to evaluate sensory-nerve irritation or significant soft-tissue injuries and to identify pain sources. (5)
- The primary way that thermal imaging works is by detecting temperature variations related to blood flow and demonstrating abnormal patterns associated with the progression of tumors. When the body is viewed through a thermal imaging camera, warm areas stand out against cooler areas, and changes in patterns can be tracked over time. Because cancer cells are growing and multiplying very fast, blood flow and metabolism are higher in the areas near a growing tumor, which means skin temperature near these locations increases. (6)
- Thermography is not invasive, is low-cost, and does not require use of radiation.
- These tests can be especially helpful in the intervals between other types of screenings, including mammographies (which are usually not indicated for women under 50 years old). (7) Approximately 15 percent of all breast cancers occur in women under 45, which means risk assessment in this age group is still very important. Breast cancer tends to be more aggressive when it strikes this young population of women.
- Thermogram results differ from person to person, so once a “baseline” thermal image is recorded, it’s kept on file to compare against future evaluations. Some experts describe thermogram results as being like a “thermal fingerprint,” since they are unique to each person and only change if pathology (disease) develops.
- Doctors track a patient’s thermal image recordings in order to ensure that their images remain consistent and stable for several years in a row, which signifies that they aren’t experiencing abnormal changes.
Breast Cancer Thermography Research and Effectiveness
The American Cancer Society estimates that 230,480 new cases of invasive breast cancer are diagnosed every year among U.S. women alone, and that of these cases, about 1,200 women under the age of 40 die every year from breast cancer. (8)
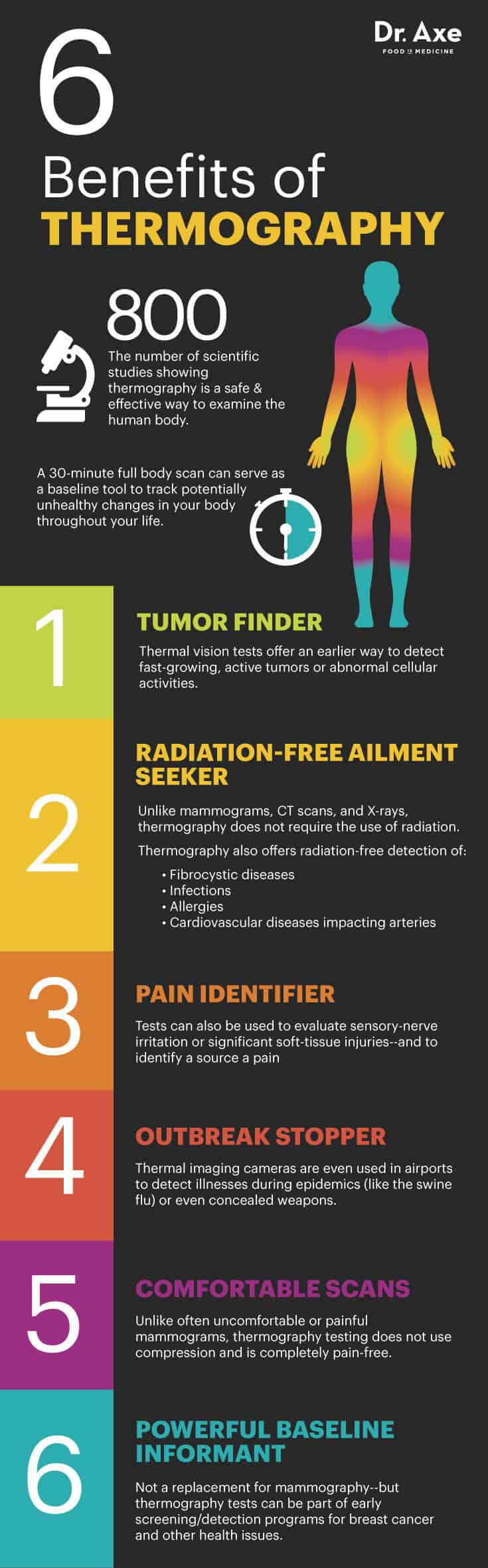
Although they aren’t intended to treat cases of cancer, thermography tests are being performed today on many adult women as part of early risk assessment programs for breast cancer. They’re even commonly recommended for women under the age of 50, the age group that mammograms might be the least accurate for. This gives women of all ages the best possible protection against breast cancer by offering the opportunity to establish risk factors early on. Thermography has the ability to identify patients at the highest risk and actually increase the effective usage of mammograms imaging procedures afterwards.
- One of the primary advantages of thermography is that it’s usually performed years before conventional mammograms are ordered. This allows doctors to identify patients who are at a higher risk for cancer development so that they can be monitored more carefully
- Following thermography indicating a potential problem in the breast, it’s very common to utilize other tests like mammography or ultrasound to confirm if there is a lesion, growth or tumor forming. Because various tests are used together to give the patient the best chance of a full recovery and positive outcome, thermography has been called “an adjunct to the appropriate usage of mammography, and not a competitor.”
- As of now, the American Cancer Society does not recommend thermography as a replacement for mammograms. Thermography can be used to supplement information from a mammogram to help identify cancer, the organization notes.
Thermography tests can also detect subtle changes in breast temperature that indicate a variety of breast diseases other than cancer, too. These include other forms of fibrocystic syndrome or Paget’s disease. A detection of abnormal heat patterns will then lead your doctor to prescribe follow-up procedures, in order to properly diagnose your condition and confirm if, or if not, you’re developing cancer.
Is Thermography Always Safe and Effective?
Here’s what you need to know first before having a thermogram done:
- In February 2019, the U.S. Food and Drug Administration (FDA) issued a safety communication to warn patients that thermography is “not cleared by the FDA as an alternative to mammography and should not replace mammography for breast cancer screening or diagnosis.” At the same time the FDA also issued a warning letter to a clinical in California that offers thermography to patients stating that the clinic was “illegally marketing and distributing an unapproved thermography device as a sole screening device for breast cancer and other diseases.” This is the sixth time the FDA has sent warning letters to manufacturers for marketing unapproved thermographic devices and/or making misleading claims about thermography.
- The FDA has stated that in their opinion, people who substitute thermography for mammography may miss the chance to detect breast cancer in its earliest and most treatable stages.
- The FDA does consider IR Thermography to be a safe practice when used as an adjunctive tool in cancer screening; thermography tests were FDA registered as of 1982. However, thermography is still considered an “alternative screening option” for cancer and is not intended to replace other procedures.
- The latest version of the The American Cancer Society’s Guidelines for Breast Cancer Screening does not consider thermography alone an effective way to screen for cancer. (9) The FDA remains concerned that women will believe thermography tests can replace mammograms altogether, and they advise all patients to still receive regular mammograms according to screening guidelines and recommended by their health care providers. (10)
- Thermography is painless and does not require the use of invasive procedures or even radiation, and there is no contact. However, it’s not 100 percent accurate (no test is) and is best used along with other detection methods.
- Thermographers should always a hold certification from a professional school. Check with your provider to make sure the facility is following all approved codes of ethics and quality control guidelines.
Pre-Imaging Protocol Guidelines
Prior to having a thermal imaging test done, you’ll be expected to prepare by following these guidelines:
- Avoid attending physical therapy, getting a massage, or having a test using electromyography done on the same day as thermography
- Wear loose clothing to the test
- You shouldn’t exercise within 4 hours of your test, since this can affect your internal body temperature
- Don’t drink anything very hot or cold for at least 2 hours before the test, however you can eat normally
- Avoid smoking at least 2 hours before the test
- Don’t use any products including lotion, deodorant, perfume, powder, etc. on your skin before the test
- Don’t have a thermal imaging test if you have a sunburn on your skin. And following the test stay out of the sun for the day
What to Do After Thermography
If your thermography is abnormal, wondering what you do next?
If your doctor suspects a problem based on your thermogram results, you’ll be closely monitored and offered a number of treatment paths. Ultimately you want to make sure that your thermography results are interpreted by an adequately trained and experienced doctor who can help you make the best decisions about your treatment plan. No matter what avenue you choose to go down in order to slow the progression of your disease, there are several things that you can do to help you manage (and hopefully completely overcome) your health condition:
- Eat a nutrient-dense diet and limit consumption of processed, packaged foods. Make sure to include plenty cancer-fighting foods including leafy greens, probiotic foods and berries.
- Consider trying the Gersen Therapy or Budwig Protocols and vegetable-juicing, in order to supply your body with plenty of healing nutrients and antioxidants.
- Exercise regularly, manage stress and get plenty of rest.
- Avoiding too many cocktails. Alcohol and breast cancer risk are intricately linked. The more you drink, the higher your risk of developing breast cancer.
- Improve your body’s ability to detox by utilizing supplements (such as turmeric/curcumin, medicinal mushrooms, pancreatic proteolytic enzymes, potassium, omega-3 fish oils and vitamin B12). Even consider trying safe and effective coffee enemas.
- Spend about 20 minutes outdoors everyday in order to produce enough vitamin D.
- Find support in whatever way works for you, whether it’s online, joining a support group, or through prayer.
- Research other alternative cancer treatments including oxygen therapy, hyperbaric chambers, vitamin C chelation therapy and frankincense essential oil.
Final Thoughts
Thermography is a safe, contact-free, radiation-free tool that can be used in risk assessment for several diseases, including breast cancer. Thermography should not take the place of other recommended screenings, but serve be a powerful tool to track diseases in your body that could point to early disease development.


