This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Cluster Headaches Causes and Possible Treatments
February 28, 2023

A cluster headache is one of the most painful afflictions. Sufferers have described cluster headaches as a hot dagger being poked through the eye and into the brain. Women have even compared cluster headache pain to be equivalent to labor pain, while men express that it’s the worst pain they’ve ever felt.
Although the pain can be intense, cluster headaches are rare and the symptoms can be reduced or relieved with a mix of conventional and natural headache remedies. Let’s explore the most effective conventional and natural treatments, along with the symptoms and causes of cluster headaches and how they differ from a migraine or even a tension headache.
What Is a Cluster Headache?
Cluster headaches involve intense and relentless pain in or around one eye on one side of the head. The symptoms can sometimes be confused with a migraine, but there is one major difference. This type of headache occurs in patterns, and it arises in cluster periods — or outbursts of frequent attacks that generally last from six to 12 weeks. A cluster period usually ends in remission, when there are no symptoms for months or even years.
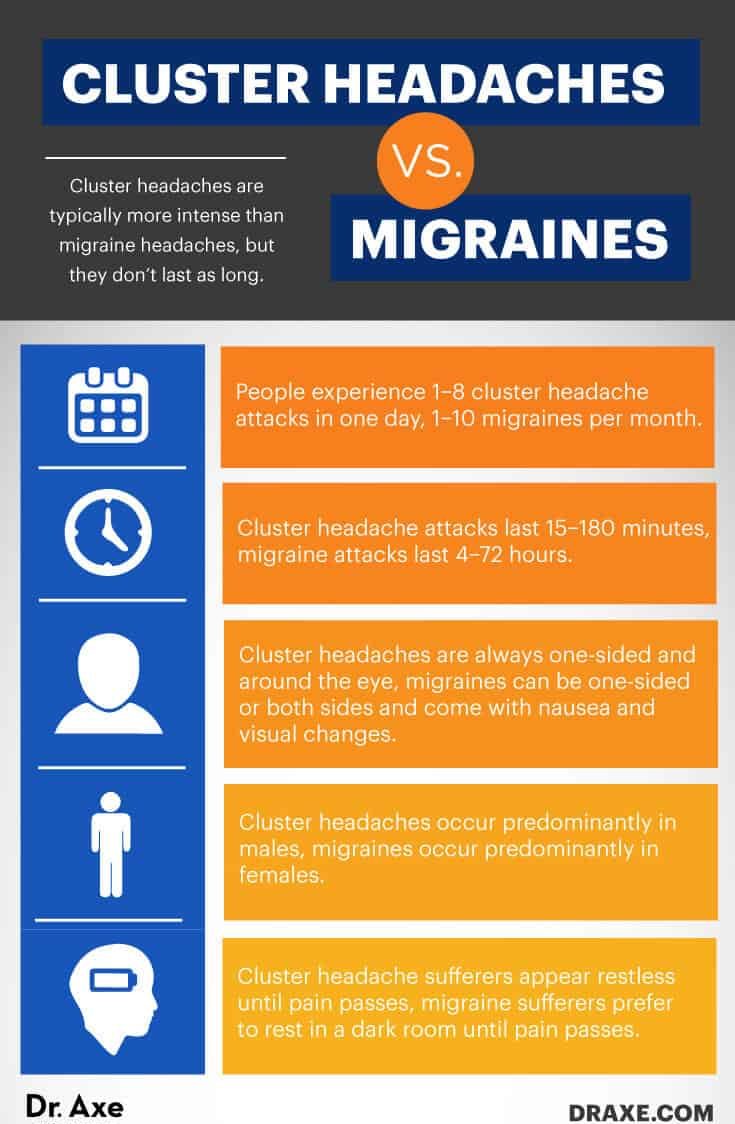
Given the intense, oftentimes debilitating pain associated with the two, cluster headaches and migraines can be difficult to distinguish at first. However, there are several ways in which you can tell the difference between these types of headaches, such as:
- Cluster headaches are typically more intense than migraine headaches, but they don’t last as long.
- People experience one to eight cluster headache attacks in one day, while migraines typically occur one to 10 times per month.
- Cluster headache attacks last 15–180 minutes, while migraine attacks last four to 72 hours.
- Cluster headaches are always one-sided and around the eye, whereas migraines can be one-sided or both sides and come with nausea and visual changes.
- Cluster headaches occur predominantly in males, while migraines occur predominantly in females.
- Cluster headache sufferers appear restless until pain passes, but migraine sufferers prefer to rest in a dark room until pain passes.
Symptoms
The duration of cluster headaches is different for everyone: 80 percent to 90 percent of people who suffer from cluster headaches experience a cluster period that lasts for several weeks and then a remission period for a year, when they experience no symptoms. Chronic cluster periods, which occur in about 20 percent of people, may continue for more than a year, with only a short remission period.
A single cluster headache attack typically lasts between 15 minutes and three hours. During a cluster period, a headache hits around the same time every day, usually occurring at night a few hours after going to bed.
Lying down during a cluster headache attack seems to worsen the conditions, so people are awakened during night attacks and appear restless, pacing back and forth or sitting through an outburst. Some people also experience agitation, changes in heart rate and blood pressure, and sensitivity to light, sound or smell. There are daytime attacks as well, sometimes one to three a day, but they’re typically less severe than nightly bouts.
An attack usually lasts between 15–180 minutes, and then it ends just as rapidly as it began. Although the cluster headache pain ends suddenly, studies indicate that it leaves the person feeling drained and weak afterward.
Here are the most common cluster headache symptoms:
- Excruciating pain that is almost always one-sided, located behind or in the eye region and radiating to the forehead, temple, nose, cheek or upper gum of the affected side.
- Constant pain during an attack that’s described as burning, throbbing or piercing.
- Pain that lasts from 15 minutes to three hours — an attack generally occurs one to three times throughout the day, typically at the same time every day, which is why they’re sometimes called “alarm clock headaches.”
Causes
Cluster headaches are rare, only affecting less than one in 1,000 people, and population-based surveys suggest that there is a considerable diagnostic delay of about seven years. Cluster headaches occur predominantly in males, with a 9:1 ratio of males to females. They generally begin between the ages of 20 and 50, but they may start at any age. Smokers tend to experience cluster headaches more often than nonsmokers.
The headache occurs when the nerve pathway in the base of the brain, called the trigeminalautonomic reflex pathway, is activated. This main nerve is responsible for sensations in the face, so when it’s activated it causes eye pain — a major symptom of cluster headaches. The activated trigeminal nerve also stimulates another group of nerves that cause other symptoms of cluster headaches, such as eye tearing and redness, nasal congestion, and discharge.
Cluster headaches are not caused by an underlying brain condition, like a tumor or aneurysm, but they do seem to come from the hypothalamus, a section of the brain that governs physiological functions, such as temperature, regulation, thirst, hunger, sleep, mood, sex drive and the release of hormones within the body. Recent studies have shown that the hypothalamus is stimulated during a cluster attack.
A 2013 study conducted in China detected significant increases of functional correlation to the right hypothalamus in cluster headache patients during “in attack” periods in comparison to those during the “out of attack” periods. Researchers concluded that cluster headache patients have a dysfunction of brain function connectivity, mainly in brain regions that are related to pain processing.
Cluster headaches are commonly mistaken for allergies because they tend to occur in the spring and fall, which further suggests that the hypothalamus plays a role in this condition. Some researchers posit that the increased familial risk suggests that cluster headaches have a genetic component in some families as well.
Conventional Treatment
There is no cure for cluster headaches, so treatments are used to relieve the symptoms and prevent future attacks. Here is a brief explanation of the most common conventional cluster headache treatments:
1. Deep Brain Stimulation of the Hypothalamus
Because tests have shown that the posterior hypothalamus is activated during cluster headache attacks, the stimulation of the ipsilateral posterior hypothalamus is used to counteract the hyperactivity and prevent intractable cluster headaches.
Hypothalamic stimulation has proved to be success at preventing attacks in more than 60 percent of 58 hypothalamic implanted, drug-resistant and chronic cluster headache patients. The study, published in Therapeutic Advances in Neurological Disorders, states that the implantation procedure has generally been proven safe, although it does carry a small risk of brain hemorrhage.
2. Verapamil
One clinical trial found that 360 milligrams a day of verapamil was superior to the placebo. In clinical practice, daily doses of 480–720 milligrams are mostly used, which may be double the dose used in cardiology. Although verapamil is the most common medication prescribed for cluster headaches, methysergide, lithium and divalproex sodium may also be used.
A 2021 study indicates that gabapentin, topiramate, divalproex sodium and melatonin are other drugs that are possibly effective for preventing cluster headaches. New drug therapies being considered also include ketamine, onabotulinumtoxinA, lysergic acid and sodium oxybate.
3. Corticosteroids
Corticosteroids are often known as steroids, anti-inflammatory medicines that are prescribed for a wide range of conditions, including painful and inflamed joints, inflammatory bowel disease, Crohn’s disease, and chronic obstructive pulmonary disease. Corticosteroids are used to replace certain hormones that are not being produced by the body naturally, and they have been used in the treatment of cluster headaches for 50 years.
Researchers state that corticosteroids are effective when used as a treatment for cluster headaches because they influence inflammation, hypothalamic-pituitary-adrenals, histaminergic and opioid systems. The downside of using corticosteroids for cluster headaches is that a high dose is needed, which comes with safety concerns.
That’s why this type of medication shouldn’t be used for more than four weeks at a time. The possible side effects from corticosteroids include thinned skin that bruises easily, an increased risk of infection, mood changes, diabetes, high blood pressure, osteoporosis and withdrawal symptoms.
4. Occipital Nerve Blockages
An occipital nerve block is an injection of a steroid around the occipital nerves that are located on the back of the head, just about the neck area. Our occipital nerves supply feeling, including pain, to a good portion of the back and top of the head.
The injected steroid reduces inflammation and swelling of tissue around the occipital nerves, which helps to reduce headache pain. The injection needs to be done at a health care clinic or doctor’s office; it typically starts working in three to five hours, and its effect can last for several days to a few months. The most common side effect of occipital nerve blockages is pain at the injection sight. Some uncommon side effects include infection, bleeding and worsening of symptoms.
There are mixed reviews about the efficacy of occipital nerve blocks. A 2005 study conducted in Germany found that the injections were not effective in the treatment of chronic tension headaches. Another review published in Current Pain and Headache Reports mentions that some studies did show positive outcomes, but few were controlled and blinded, so more research is needed.
5. Sumatriptan
Sumatriptan is typically used in the treatment of migraine headaches. It’s a class of medications called selective serotonin receptor agonists. Sumatriptan narrows the blood vessels in the head, stopping pain signals from being sent to the brain and blocking the release of substances that cause headache symptoms.
Sumatriptan does not prevent headache attacks or reduce the number of headaches attacks; it only relieves the symptoms. It may cause side effects, including drowsiness, weakness, dizziness, upset stomach, diarrhea, nausea and muscle cramps.
Most studies suggest that sumatriptan is effective for the treatment of a single acute headache or migraine attack. In order to treat cluster headaches, the medication would have to be taken with each attack, which can be up to eight times a day.
Natural Treatments
Natural remedies for cluster headaches include certain supplements and lifestyle changes.
1. Magnesium
People who suffer from cluster headaches typically have low blood levels of magnesium and can benefit from magnesium supplementation or injections. Preliminary trials show that intravenous magnesium injections may relieve a cluster headache attack, and a magnesium deficiency can cause exasperated conditions.
To relieve cluster headache symptoms and reduce attacks, take 400 milligrams of magnesium three times a day, taking one capsule before bedtime because attacks are most common in middle of the night. Eating magnesium-rich foods like spinach, chard, pumpkin seeds, yogurt, almonds, black beans, avocado and bananas can also be helpful.
2. Vitamin B2
Vitamin B2 may decrease the severity and frequency of cluster headaches. It’s an important vitamin that also acts as an antioxidant in the body, maintaining healthy blood cells and boosting energy levels.
A vitamin B2 deficiency can result in nerve damage and inflammation, two conditions that may increase the intensity of cluster headaches. In a 2004 study published in the European Journal of Neurology, patients who received 400 milligrams of vitamin B2 capsules per day experienced fewer headache attacks than before supplementation.
3. Kudzu Extract
Kudzu extract comes from a semi-woody, perennial and leguminous vine native to Southeast Asia. For more than 2,000 years, kudzu has been used as an herbal treatment for fever, acute dysentery, diarrhea, diabetes and cardiovascular disease. Over 70 phytochemicals or phytonutrients have been identified in kudzu root, with isoflavonoids and triterpenoids as the major constituents.
In 2009, cluster headache patients were questioned about their use of various alternative remedies. Of the 235 patients identified, 16 had used kudzu, and they consented to interviews and provided medical records. Eleven (69 percent) experienced decreased intensity of attacks, nine (56 percent) decreased frequency and five (31 percent) experienced decreased duration — all with minimal side effects.
4. Melatonin
Melatonin is used as an adjunctive therapy in patients with cluster headaches who have incomplete relief of their headaches when using conventional treatments. Melatonin levels have been found to be decreased in cluster headache patients, and a lack of melatonin secretion may predispose the patient to headache attacks.
Some studies have found that melatonin treatment can rapidly alleviate cluster attacks but only in episodic cluster headache patients. In studies that showed no results after treatment, researchers suggested that melatonin be used before the cluster period begins for the best results.
5. Capsaicin Cream
Apply a small amount of capsaicin cream to the inside of your nostril (the same side that’s experiencing the pain). The main ingredient in capsaicin cream is cayenne pepper, which works by blocking nerve pain signals.
A study published in the Clinical Journal of Pain states that capsaicin application reduced the number of headache attacks in the 60 days after the end of treatment. For some people, applying capsaicin cream to the inside of the nostril can cause a temporary painful sensation, sneezing and nasal secretion — however, as the results indicate, it can help remedy cluster headaches.
6. Psilocybin Mushrooms
These psychedelic mushrooms may seem like a strange natural treatment for incredibly painful cluster headaches, but many sufferers are turning to psilocybin mushrooms for relief when nothing else has worked. Psilocybin is a classic hallucinogen, and case studies suggest that it may be effective for the treatment of cluster headaches.
These reports suggest that further research on the effects of doses of psilocybin on cluster headaches may be warranted.
7. Get Outdoors
People with cluster headaches experience a relief of symptoms after receiving oxygen during an attack. This can be done naturally by getting outdoors and taking deep breathes of fresh air, such as forest bathing.
8. Exercise
Daily exercise can reduce stress and boost blood circulation. In between headache attacks and when in remission, take a long hike, attend a yoga class or practice interval training. It’s been proven to help relieve headache symptoms, adding cluster headache relief to the long list of the benefits of exercise.
9. Breathing Exercises
Deep, rhythmic breathing allows more oxygen into the brain, relieving the pain during headache attacks and leaving the body at ease. That’s what makes yoga such a great activity for headache suffers. Its physical exercise combined with breathing exercises have been found to alleviated headache symptoms.
10. Stick to a Regular Sleep Schedule
A 2020 study revealed that cluster headaches can often begin during your sleep cycles, and they may be related to sleep apnea. It’s important that people who experience cluster headaches stick to a regular sleep schedule.
Cluster periods may actually begin when there are changes in your normal sleep routine, so it helps to stay consistent. If you have insomnia, that could also trigger cluster headaches, so do everything you can to ensure a regular, quality sleep schedule.
11. Use Peppermint Essential Oil
Peppermint oil is known to relieve headaches, boost energy, release tight muscles and improve mental focus. Before and during a cluster headache attack, apply two to three drops of peppermint oil topically to the temples, back of neck and bottoms of the feet.
12. Drink Ginger Tea
A bioactive ingredient in ginger, called gingerol, has therapeutic benefits. It acts as a highly potent antioxidant and anti-inflammatory agent. It also reduces pain by acting on vanilloid receptors and relieves nausea, which can be a symptom of intense cluster headache attacks.
Drink ginger tea one to two times daily to relieve the symptoms of cluster headaches.
13. Avoid Alcohol and Tobacco
Alcohol and tobacco use can increase the frequency of cluster headache attacks and make the pain even worse. If you suffer from cluster headaches, avoid alcohol and tobacco, especially during a cluster period.
Final Thoughts
- Cluster headaches only occur in one out of every 1,000 people. Although they’re rare, they can be a serious condition for sufferers, as the pain is continuous and excruciating.
- There are a number of conventional treatments for cluster headaches; they mainly focus on reducing pain and frequency of cluster headache attacks.
- Some natural remedies, such as magnesium and vitamin B2 supplements, capsaicin cream and melatonin, have proven to be effective against cluster headaches. They won’t stop the attacks altogether, but they do offer relief from the pain and frequency of attacks.
- Some easy lifestyle changes can help to reduce the symptoms of headache clusters, including deep breathing exercises, avoiding alcohol and tobacco, and using peppermint oil before and during attacks.








