This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Gestational Diabetes: Get the Test (+ Natural Management Tips)
January 26, 2018

You may have heard from your doctor or midwife that gestational diabetes increases your risk of complications during pregnancy — such as miscarriage, the baby being born too early or delivery by cesarean section. But did you know that gestational diabetes is also associated with Type 2 diabetes and cardiovascular disease after pregnancy?
It’s true that gestational diabetes is a dangerous condition that develops during pregnancy, but there are ways to prevent and manage it. Your first line of defense is to follow a diabetic diet plan and make lifestyle changes, like adding in physical activity. There are also certain nutrients that can help to reduce your risk of gestational diabetes and maintain glycemic control.
The key to managing gestational diabetes is to become educated about the foods you should and shouldn’t eat during pregnancy, what everyday lifestyle changes you can make to maintain normal blood sugar levels, and where to get support if you need it. If you are diagnosed with gestational diabetes, you need to take action immediately, as the adverse effects are serious. But know that there are professionals who can help you to develop an effective treatment plan.
What Is Gestational Diabetes?
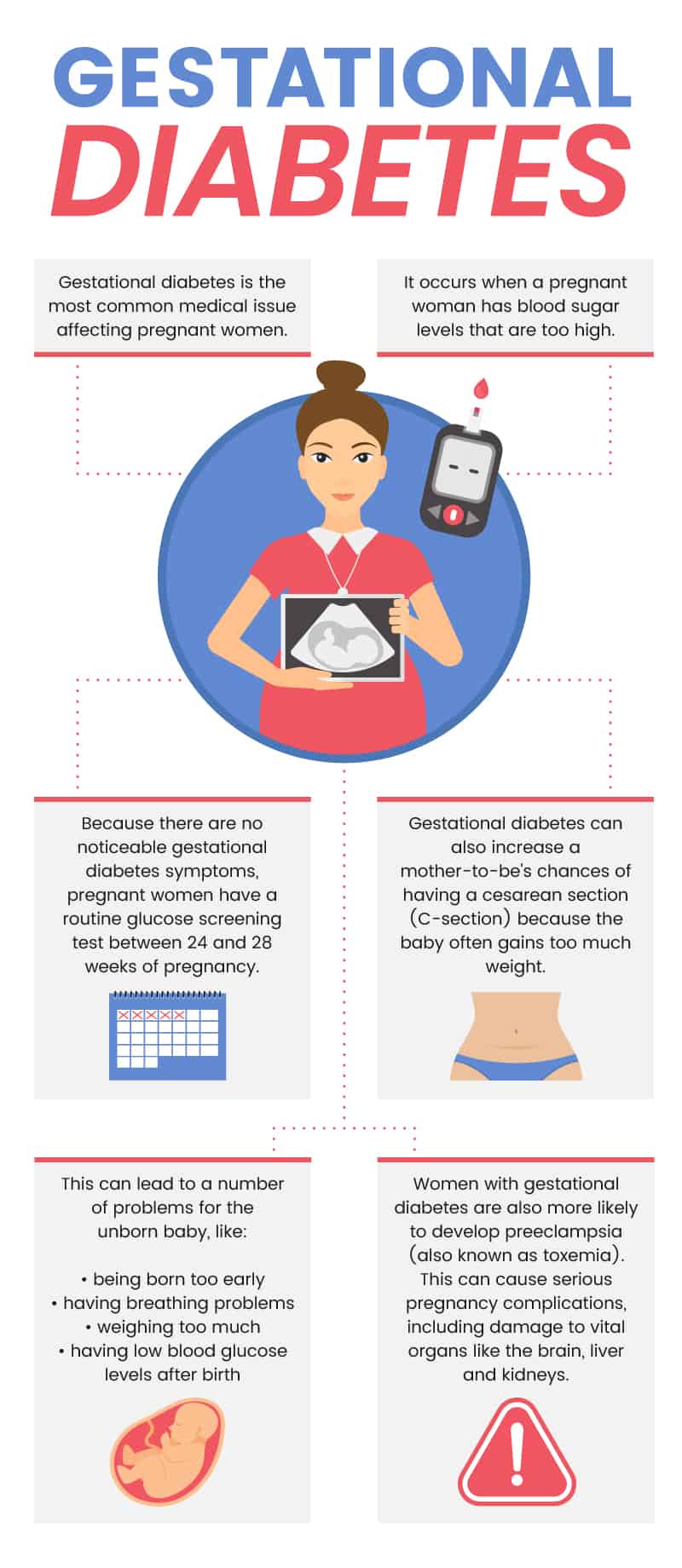
Gestational diabetes is the most common medical issue affecting pregnant women. It’s a type of diabetes that’s actually diagnosed between the 24th and 28th weeks of pregnancy. It occurs when a pregnant woman has blood sugar levels that are too high. This can lead to a number of problems for the unborn baby, like being born too early, having problems with breathing, weighing too much and having low blood glucose levels after birth. (1)
Gestational diabetes is also dangerous for the baby because high blood glucose levels can increase the chance of having a miscarriage or stillborn birth (when the baby dies after 24 weeks of pregnancy). Although insulin secretion increases in early pregnancy, insulin sensitivity is usually unchanged. But at mid-pregnancy, insulin sensitivity starts to decline progressively. The decline becomes worse as the pregnancy progresses. This is why gestational diabetes usually develops in the late second trimester and then disappears instantly after delivery.
For pregnant women, gestational diabetes may predispose them to develop diabetes after giving birth. Women with gestational diabetes are also more likely to develop preeclampsia, a condition that involves the abnormal development of the placenta, high blood pressure during pregnancy and high levels of protein in your urine. Preeclampsia — also known as toxemia — can cause serious pregnancy complications, including damage to vital organs like the brain, liver and kidneys. Gestational diabetes can also increase a mother-to-be’s chances of having a cesarean section because the baby often gains too much weight.
And a recent study, published in December of 2017 in JAMA Internal Medicine, found that gestational diabetes is positively associated with cardiovascular disease later in life. Over 89,000 pregnant women who were free of cardiovascular disease when the study began participated in questionnaires that evaluated their cardiovascular health after pregnancy. Researchers found that women with a history of gestational diabetes had a 43 percent greater risk of developing cardiovascular disease. They also indicate that this relationship between gestational diabetes and cardiovascular disease — particularly the incidence of heart attack and stroke — is possibly mediated, at least in part, by weight gain and lack of healthy lifestyle during and after pregnancy. (2)
Data shows that the prevalence of gestational diabetes varies from 1–20 percent and continues to rise worldwide. And the amount of gestational diabetes varies in direct proportion to the commonality of Type 2 diabetes in a given population, with the rates being higher among African, Hispanic, Indian and Asian women than for Caucasian women. (3)
Gestational Diabetes Symptoms & Glucose Screening Tests
Women with gestational diabetes usually don’t experience any symptoms. Most of the time, the barely noticeable symptoms of gestational diabetes are very similar to normal pregnancy symptoms. You may notice that you’re feeling: (4)
- tired and fatigued
- very thirsty
- the need to urinate often
Because there are no noticeable gestational diabetes symptoms, pregnant women go through a routine glucose screening test that’s done between 24 and 28 weeks of pregnancy. For women who have high glucose levels in their urine during their routine prenatal visits, they my be tested for gestational diabetes sooner.
The test requires you to drink a sweet liquid that contains glucose. Then you have your blood drawn one hour later to measure how the glucose solution affected your blood glucose levels. The normal result for this kind of test is a blood sugar level that’s 140 milliliters per deciliter or less one hour after drinking the glucose solution. If your blood levels are too high for the one-hour test, you will be asked to return for a three-hour glucose tolerance test. (5)
For the three-hour test, you cannot eat or drink anything, other than a few sips of water, for eight–14 hours beforehand. You will drink a sweet liquid containing glucose, then wait an hour and have your blood drawn in order to check your blood glucose levels. This needs to be repeated three times. (6)
Although it’s not common to feel symptoms of gestational diabetes, drinking the sugary liquid may make you feel lightheaded and nauseated, especially if you aren’t able to eat or drink anything beforehand. Don’t worry; these symptoms will pass once the test is over and you are able to enjoy a full meal.
Causes & Risk Factors
It’s not exactly clear why some pregnant women develop gestational diabetes and others don’t. Gestational diabetes is caused by high blood sugar levels. Normally, when you eat something, your body digests that food to produce glucose. The glucose enters your bloodstream. With the help of your pancreas, it then moves into your body’s cells so that it can be used for energy. During pregnancy, however, the placenta produces high levels of insulin-counteracting hormones. These hormones impair the action of insulin in your body’s cells, thereby raising your blood sugar levels.
Some women only experience modest elevations of blood sugar after eating, which is completely normal during pregnancy. But others are affected by the growth of the placenta and rise of hormones. These women go on to develop gestational diabetes, usually around 24 weeks of pregnancy.
There are risk factors that put pregnant women at a greater risk of developing gestational diabetes. The most common risk factors include:
- High BMI: Research shows that a higher BMI before pregnancy and a higher BMI at 28 weeks of pregnancy are strongly related to increased insulin resistance. A BMI of 30 or higher can increase your risk of developing gestational diabetes. (7)
- Ethnicity: Studies show that African-American, Hispanic, Asian and Native American women living in the United States have a higher risk of developing gestational diabetes than Caucasian women in the U.S. (8)
- Age: If a pregnant woman is over the age of 25, she is at a greater risk of developing gestational diabetes.
- History of Diabetes: Women who have already had gestational diabetes, or those with prediabetes symptoms before pregnancy, are at a greater risk of developing gestational diabetes again. If you have a family history of diabetes, such as a parent or sibling having Type 2 diabetes, you are also at an increased risk of gestational diabetes.
- Polycystic Ovary Syndrome: A nationwide population-based survey published in PLoS ONE indicates that a history of polycystic ovarian syndrome (PCOS) is a significant and independent risk factor for the development of gestational diabetes. About 50 percent of women with PCOS experience metabolic disturbances, which is why they are often monitored closely during pregnancy to ensure that they they follow a strict diet and don’t gain too much weight. (9)
Conventional Treatment
There are a number of conventional treatments for gestational diabetes. Along with dietary changes and increased physical activity, the following medications or forms of therapy may be utilized: (10, 11)
Insulin Therapy: Insulin injections may be needed to lower your blood sugar levels. Insulin therapy is utilized when dietary and lifestyle changes alone do not maintain glycemic control during pregnancy.
Glyburide: Glyburide is an oral antidiabetic agent that is often used as a first-line agent for gestational diabetes or as an alternative to insulin therapy.
Metformin: Metformin is another oral anti-diabetic drug that’s used to fight gestational diabetes. According to researchers, there is now a reasonable amount of data to support that both metformin and glyburide can be useful for women with gestational diabetes. The safety and efficacy of these drugs, compared to insulin therapy, are still being researched. (12)
Women with gestational diabetes will have to monitor their blood sugar levels to make sure that they stay in a healthy range. To do this, you simply draw blood from your finger and place it on a test strip that serves as a blood glucose meter. The meter will measure and display your blood sugar levels so that you can be sure they’re normal in the morning and after meals.
5 Natural Ways to Manage Gestational Diabetes Symptoms
1. Nutritional Therapy
Your pregnancy diet is the most important factor in preventing and managing gestational diabetes. Pregnant women need to eat a diet that provides adequate nutrition in order to support their baby’s and their own well-being. It’s very important that women who are pregnant don’t consume too many calories, especially empty calories that come from processed and packaged foods, junk food, baked goods and sweetened beverages. Achieving appropriate weight gain is one of the most important ways to prevent and manage gestational diabetes. During pregnancy, excessive weight gain can lead to adverse outcomes for both the mother and baby. Plus it can even lead to childhood obesity for your little one. (13)
Here are some dietary tips for managing gestational diabetes:
- Your carbohydrate intake should only be 35 percent to 45 percent of your total calories per day. Distribute your carb intake over three meals and about two to three snacks. Avoid eating meals that are carb-heavy, like a bagel, a bowl of pasta, a plate of pancakes or a bowl of fruit.
- Make sure you’re eating plenty of high fiber foods, which can help to slow down or decrease the release of insulin into the bloodstream. Include fiber in all of your meals and snacks throughout the day. Some of the best options include avocados, squash, beans, lentils, chia seeds and flax seeds.
- Pair your carbohydrates with good quality protein so that your body can more easily break down the carbs. Some of the best high protein foods to include in your diet include grass-fed beef, organic chicken, wild-caught salmon, eggs, yogurt, nuts and bone broth.
- Use healthy fats in your recipes, like coconut oil, ghee and grass-fed butter. These foods help to burn fat and balance your blood glucose levels.
- Avoid sugary foods that will throw off your blood sugar levels. Simple, refined sugars that are found in soda, fruit juice and other sweetened beverages are some of the worst culprits for women with gestational diabetes because they lead to rapid blood glucose spikes.
2. Physical Activity
Research shows that exercise can improve glycemic control in women with gestational diabetes. Moderate physical activity for 30 minutes a day or more is recommended for all pregnant women and especially those with gestational diabetes, as long as there aren’t any medical or obstetric complications. (14)
Some beneficial exercises for women with gestational diabetes includes brisk walking, arm exercises while seated in a chair and prenatal yoga. Engaging in these types of physical activity at least 10 minutes after each meal can help to reduce the rise of glucose levels, helping women with gestational diabetes to reach their glycemic goals.

3. Stress Management
Research shows that women with gestational diabetes often experience stress and anxiety that’s related to feeling like they’re losing control of their condition, having trouble sticking to dietary changes, and experiencing fear of maternal and infant complications. (15)
A 2012 study conducted at the National University of Ireland found that when 25 women with gestational diabetes were compared to 25 women without gestational diabetes, those with the condition were more likely to become depressed and experienced diabetes-related distress. Women with gestational diabetes also felt like they didn’t have enough social support from outside their family. (16)
This risk of increased stress, anxiety and signs of depression during pregnancy is problematic because these mental health issues can affect your hormone levels, including your insulin levels. Plus, studies show that stress, anxiety and depression during pregnancy is associated with lower birth weight for infants and potential issues with infant development. Experiencing stress and depression during pregnancy also increases your risk of suffering from postpartum depression after giving birth. (17)
To manage your stress levels, start by finding a support group, a nutritionist, dietitian, health coach or even a friend who has experience with gestational diabetes and can help you to find comfort and stay on track with your diet plan. You should also focus on relieving stress and anxiety by making small lifestyle changes, like taking walks outside every day, trying prenatal yoga, meditating or practicing silent prayer, journaling or taking a warm bath with lavender oil. These little changes can help you to stay focused on getting well and maintaining your health for the duration of your pregnancy.
4. Vitamin D
A number of scientific studies show an association between vitamin D deficiency and gestational diabetes. Vitamin D insufficiency is also related to maternal obesity and adverse outcomes for both the mother and child. Although the data isn’t completely conclusive yet, there have been studies that suggest that vitamin D supplementation can reduce the risk of developing gestational diabetes and help to improve glycemic control in pregnant women who are diabetic and have low vitamin D levels. (18)
5. Calcium
According to research published in Public Health Nutrition in 2017, higher dietary calcium intake was inversely associated with the risk of gestational diabetes. Compared with women who consumed less calcium, those with higher calcium levels had a 42 percent lower risk of gestational diabetes. And researchers found that among women with a calcium intake below 1,200 milligrams per day, a 200 milligram increase in daily intake was associated with a 22 percent reduction in gestational diabetes risk. (19)
The best way to increase your calcium levels is to eat calcium-rich foods like yogurt, cheese, cooked kale, broccoli and almonds. There is mixed research about the safety of calcium supplements and consuming very high levels of calcium, so talk to your doctor before using supplements to increase your levels.
Prevention
Are you thinking about becoming pregnant and want to prevent the development of gestational diabetes? It’s smart to start thinking about the threat of gestational diabetes before you’re pregnant or during the early stages of pregnancy, especially if you are overweight, have a history of gestational diabetes or prediabetes, have family members with Type 2 diabetes symptoms or have PCOS.
The best way to prevent gestational diabetes is to reach your ideal weight before getting pregnant. Losing extra weight and increasing physical activity are sure ways to reduce your risk of gestational diabetes. This will allow your body to improve how it uses insulin for energy and it will help you to maintain healthy blood sugar levels. If you are already pregnant, it’s not recommended that you try to lose weight. But you can focus on eating nourishing, nutrient-dense foods so that you don’t gain too much weight during your pregnancy.
The amount of weight that you should gain during pregnancy depends on your BMI before getting pregnant. Women at a normal weight before getting pregnant should gain between 25 and 26 pounds, and those who were overweight should only gain 15 to 25 pounds during pregnancy. (20)
Precautions
If you have been diagnosed with gestational diabetes, it’s important that you work with your health care provider to manage your condition until the end of your pregnancy and even after giving birth. Work with your doctor or a nutrition expert to set up a dietary and lifestyle plan. If you plan to use these natural ways to manage your gestational diabetes, do it under the care of your doctor. Gestational diabetes can lead to many adverse effects for you and your baby, so it’s important that it’s treated properly as soon as you’re diagnosed.
Key Points
- Gestational diabetes is the most common medical issue that affects pregnant women. It occurs when a pregnant woman’s blood sugar levels are too high and the condition is usually diagnosed after 24 weeks of pregnancy.
- Women with gestational diabetes usually don’t experience any symptoms, but they may notice signs like fatigue, feeling very thirsty and needing to urinate frequently. These signs are normal for any pregnant woman, so a glucose screening is necessary around your 24th week of pregnancy.
- Gestational diabetes is caused by high blood sugar levels. Because your placenta produces high levels of insulin-counteracting hormones during pregnancy, this impairs the action of insulin in a pregnant woman’s body, leading to increased blood sugar levels. It’s not exactly clear why some women get gestational diabetes and others don’t. But women with a high BMI, those over the age of 25, women with PCOS, and those with a family or personal history of diabetes are at a greater risk.
- The first line of defense for gestational diabetes is dietary and lifestyle changes. When these changes don’t work to maintain glycemic control, insulin therapy or oral anti-diabetic agents are used.
5 Natural Ways to Manage Gestational Diabetes Include:
- Nutrition therapy
- Physical activity
- Managing stress
- Increasing vitamin D intake
- Increasing calcium intake




