This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Myocarditis: Causes 45% of Heart Transplants in the U.S. Each Year
May 3, 2018

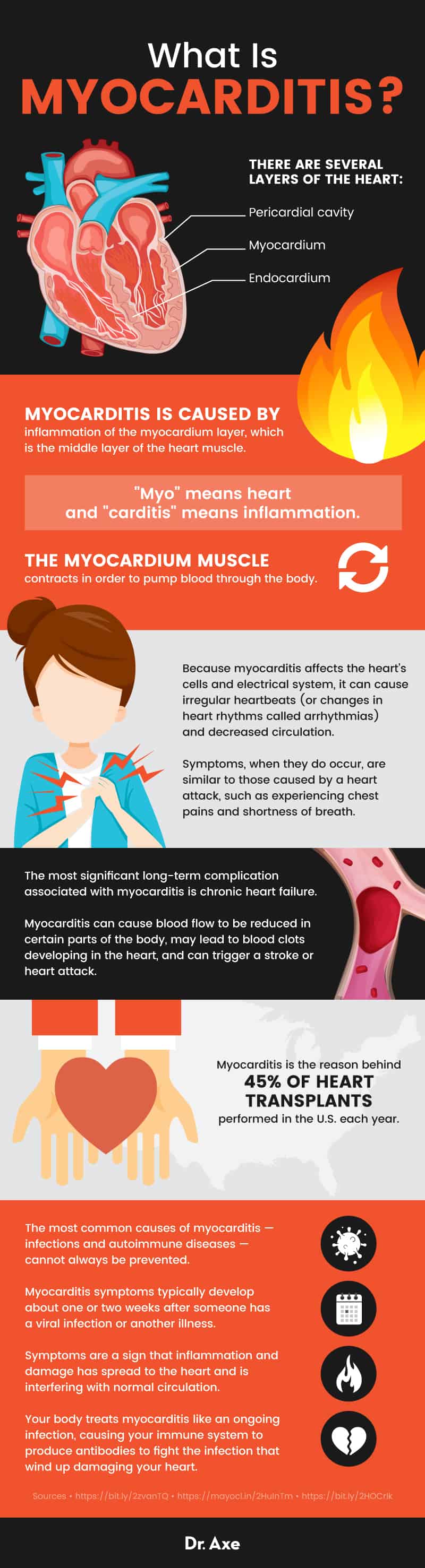
Myocarditis is a rare type of heart disease that usually causes no symptoms, but it can be life-threatening. Myocarditis gets its name because the middle layer of the heart muscle is called the myocardium. “Myo” means heart and “carditis” means inflammation.
Is myocarditis a heart attack? No, but it can sometimes lead to one. Symptoms of myocarditis, when they do occur, are similar to those caused by a heart attack, such as experiencing chest pains and shortness of breath. The most significant long-term complication associated with myocarditis is chronic heart failure. Myocarditis — and the serious symptoms associated with it — is the reason behind 45 percent of heart transplants performed in the United States each year. (1)
The most common causes of myocarditis — infections and autoimmune diseases — cannot always be prevented. But there are some things you can do to decrease your risk, including strengthening your immune system, eating an anti-inflammatory diet, preventing infections by practicing good hygiene habits, and limiting autoimmune reactions by managing stress.
What Is Myocarditis?
According to the Myocarditis Foundation, “Myocarditis is a disease marked by inflammation and damage of the heart muscle.” It can affect both children (called pediatric myocarditis) and adults, including people who have no prior history of heart disease.
The myocardium muscle contracts in order to pump blood through the body. Because myocarditis affects the heart’s cells and electrical system, it can cause irregular heartbeats (or changes in heart rhythms called arrhythmias) and decreased circulation.
Myocarditis can cause blood flow to be reduced in certain parts of the body, may lead to blood clots developing in the heart, and can trigger a stroke or heart attack. This does not always happen, but it is possible when myocarditis becomes severe. (2) Sometimes scar tissue (fibrosis) can develop in the myocardium, which increases the risk for long-term complications.
Symptoms and Signs
Myocarditis usually affects people who are otherwise healthy and it’s the cause of between 5 percent to 20 percent of all cases of sudden death in young adults. Most people with myocarditis experience no noticeable symptoms or signs. How is a heart infection diagnosed? Someone might display certain symptoms, or they might only receive a diagnosis after an electrocardiogram (ECG) or blood test reveals signs of heart injury or inflammation.
When symptoms of myocarditis do occur they can include: (3)
- Shortness of breath, especially during exercise or periods of exertion. Difficulty breathing or rapid breathing might occur. Shortness of breath at night is also possible.
- Fatigue and weakness.
- Heart palpitations (abnormal heart rhythms)
- Chest pains or pressure.
- Swelling in the legs and arms due to fluid retention (called peripheral edema). Edema is usually the worst in the ankles and feet.
- Lightheadedness.
- Other symptoms due to infection (headaches, body aches, joint pain, fever, a sore throat or diarrhea).
- Sudden loss of consciousness.
- Increased risk for heart failure, blood clots, stroke or heart attack.
Myocarditis symptoms typically develop about one or two weeks after someone has a viral infection or another illness. Symptoms are a sign that inflammation and damage has spread to the heart and is interfering with normal circulation. Your body treats myocarditis like an ongoing infection, causing your immune system to produce antibodies to fight the infection that wind up damaging your heart. (4) This can cause scar tissue to form that stops the heart from pumping properly.
What type of long-term damage might myocarditis cause?
Myocarditis recovery time will depend on the severity of the condition and the person’s overall health. It might take several months to feel completely better, or longer if any permanent damage developed.
Myocarditis has been associated with permanent heart damage and in some cases can lead to sudden death, heart failure, heart attacks, stroke, and heart arrhythmias. Why does myocarditis cause swelling of the heart and heart failure? It can stop the heart muscle from properly being able to pump blood, which might cut off blood supply to the brain or other organs. Injury to the heart might also cause blood to pool in your heart and develop into clots. Clots can travel to your arteries causing a heart attack, or travel to your brain leading to a stroke. Arrhythmias might also cause your heart to stop beating (called sudden cardiac arrest), which is deadly.
Causes and Risk Factors
There are several layers of the heart, including the myocardium, endocardium and pericardial cavity. Myocarditis is caused by inflammation of the myocardium layer, which is the middle layer of the heart muscle.
What can cause the heart muscle (or myocardium) to swell and become damaged? There are many reasons that someone might become affected by myocarditis.
It’s not entirely known what causes all cases of myocarditis. Experts believe that when the myocardium becomes inflamed or damaged it is usually infectious, but not contagious and not hereditary (not passed down from parents to their children). Two of the most common causes of myocarditis are:
- Viral or bacterial infections
- Autoimmune responses that affect the heart
Infections that are associated with myocarditis include various types of upper respiratory tract infections and a variety of other types.
Myocarditis can be non-infectious, which is the case when it’s due to causes like autoimmune reactions or medications. Autoimmune responses are self-directed responses from the immune system that cause damage to various tissues and organs. Examples of autoimmune diseases include polymyositis (causing systematic/general inflammation), lupus, rheumatoid arthritis or Lyme disease.
Another type of myocarditis is called giant-cell myocarditis. The cause of this type is unknown. Giant-cell myocarditis happens when macrophages fuse together to form giant cells in the heart, interfering with normal activities.
The most common myocarditis causes include: (5)
- Viral infections. This can include the common cold, respiratory infections, hepatitis C and B, parvovirus, measles, mumps, the flu, fifth disease, HIV, herpes simplex virus, echoviruses, rubella and mononucleosis (Epstein-Barr virus). (6)
- Bacterial infections. This can include infections caused by staphylococcus, streptococcus, or tick-borne bacterium that cause Lyme disease.
- Autoimmune diseases, including lupus or Lyme disease.
- Parasites, such as Trypanosoma cruzi (which causes Chagas disease) and toxoplasma. Fungus can also cause myocarditis in people with weakened immune systems. Examples of fungi that have been associated with myocarditis include certain types of mold, candida, yeast infections and histoplasma.
- Exposure to environmental toxins or metal poisoning.
- High levels of inflammation.
- Adverse reactions to medications or recreational drugs, including cocaine. Medications including certain antibiotics, sulfonamide drugs, anti-seizure medications and cancer medications have been associated with myocarditis. Adverse reactions to these drugs can cause hypersensitivity, which inflames the heart.
- Rarely, certain types of cancer.
- Rarely due to infections caused by snake or spider bites.
Diagnosis and Conventional Treatments
There are several ways that myocarditis is diagnosed. Lab (blood) tests might reveal that levels of troponin or creatine kinase cardiac isoenzymes are elevated. ECG tests can also reveal abnormal heart rhythms by detecting T-wave inversions and saddle-shaped ET inversions. Some doctors may also choose to do imaging studies to look for an enlarged heart, or perform a biopsy of the myocardium, looking for signs of inflammation such as edema, increased lymphocytes and increased microphages. (7)
Myocarditis treatment will depend on the underlying cause of the condition and how severe the patient’s symptoms are. Mild or moderate viral myocarditis can go away on its own, so a patient’s symptoms might just be monitored. The most common way that moderate-to-severe myocarditis is treated is with steroids and medications that are used to treat heart damage and heart failure. Medications that can be prescribed for myocarditis include:
- Diuretics, to help control edema/fluid retention
- Digoxin, which helps to prevent heart failure. Digoxin helps to improve contractions of the heart muscle and to slow heartbeats, which might help control palpitations.
- Milrinone and ACE inhibitors, which help to regulate heart rhythms.
- Aldosterone agonists, which can help to prevent scarring of the heart and remove excess fluid.
- Corticosteroids to manage inflammation of the heart and prevent further damage.
- Antibiotics if an infection is the underlying cause.
- Use of oxygen to help ensure enough circulates through the body.
- If it’s been detected that someone has abnormal heart rhythms that require intervention, then they might need to take certain medications and use a pacemaker. Arrhythmias will usually resolve once inflammation levels decrease.
Your doctor might also recommend resting, avoiding any strenuous activity, and eating a low-salt diet. After having myocarditis, you’ll need to recover for a period of time and ease back into physical activity slowly.
Prevention and Natural Recovery
1. Strengthen Your Immune System with a Nutrient-Dense Diet
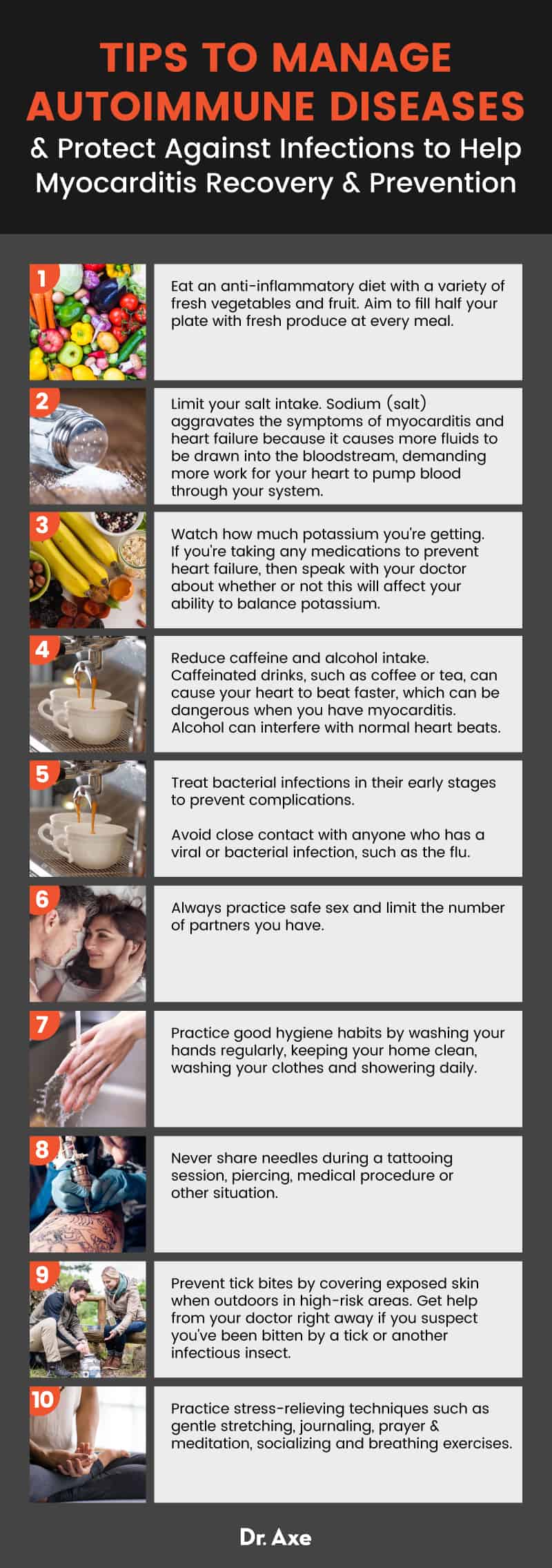
- Eat an anti-inflammatory diet. Include a variety of fresh vegetables and fruit in your diet, aiming to fill half your plate with fresh produce at every meal. Some of the best choices include leafy greens, berries, carrots, tomatoes, squash, cruciferous veggies like broccoli or cauliflower, asparagus, avocado, cranberries, blueberries, grapes and mushrooms. Other healthy food choices for heart health include flax and chia seeds, almonds and other nuts, olive oil, wild-caught fish, dark chocolate (if caffeine is OK), beans and legumes, fresh herbs and green tea.
- Limit salt intake. Sodium (salt) aggravates the symptoms of myocarditis and heart failure because it causes more fluids to be drawn into the bloodstream, demanding more work for your heart to pump blood through your system. The best way to reduce salt intake is to avoid eating processed foods, including fast food, frozen meals, canned foods, processed meats, cheeses, condiments, pre-made soups and packaged baked goods. Avoid foods that damage gut health and increase inflammation, such as those made with additives, refined grans and trans-fats.
- Watch how much potassium you’re getting. If you’re taking any medications to prevent heart failure, then speak with your doctor about whether or not this will affect your ability to balance potassium. You might need to get less or more potassium from your diet depending on your condition and any medications you take. Low potassium levels can worsen heart rhythm problems, so you might need to supplement with more if needed.
- Reduce caffeine and alcohol intake. Caffeinated drinks, such as coffee or tea, can cause your heart to beat faster, which can be dangerous when you have myocarditis. Alcohol can interfere with normal heartbeats and potentially worsen heart arrhythmia or interfere with medications you’re taking. When myocarditis is severe no alcohol or caffeine should be consumed until a doctor says otherwise because both can weaken the heart muscle.
2. Protect Against Viruses and Infections
- Treat bacterial infections in their early stages to prevent complications. Visit a doctor if you suspect you have any type of serious infection, especially if its affects your respiratory system or ability to breathe. Following surgery, an incision, cut or wound to your skin, keep a close eye on your symptoms in order to spot signs of a developing infection.
- Avoid close contact with anyone who has a viral or bacterial infection, such as the flu. Protect other people by staying home from work or school if you yourself are infected.
- Always practice safe sex and limit the number of partners you have.
- Practice good hygiene habits by washing your hands regularly, keeping your home clean, washing your clothes and showering daily. Some of the most common places that infections are spread are hospitals or doctors offices, nursing homes, daycares, schools, universities and gyms.
- Never share needles if you are ever getting a tattoo, piercing, medical procedure or using illegal drugs.
- Prevent tick bites by covering exposed skin when outdoors in high-risk areas, checking your clothing and skin afterwards, washing your clothes and controlling pests around your home. Get help from your doctor right away if you suspect you’ve been bitten by a tick or another infectious insect.
3. Reduce Autoimmune Flare-Ups
- In addition to eating an anti-inflammatory diet, you can also reduce your risk for autoimmune flare-ups by controlling stress, preventing nutrient deficiencies and getting enough sleep.
- High levels of stress can lead to many health problems, including those that affect your immune and cardiovascular systems. Uncontrolled stress is associated with higher risk of heart disease, high blood pressure and susceptibility to viral or bacterial illnesses.
- Make a plan for how you can adopt stress-relieving techniques to handle some of the biggest worries and obstacles in your life. You can start by trying to exercise gently every day, trying acupuncture, meditating or practicing mindfulness, praying, reading, writing, joining a social group, doing yoga and breathing exercises, or anything else soothing.
4. Avoid Risky Drugs or Medications
- Be cautious about using new supplements and taking over-the-counter medications when you have myocarditis because some of these can add stress to your already weakened heart. Certain medications might contain caffeine or cause your heart rate to speed up, such as headache medications or drugs used to treat colds/flu.
- Stop using tobacco and nicotine products as soon as possible since chemicals in these products can increase inflammation, worsen arrhythmias and cause damage to arteries.
- Consider taking supplements that can help reduce inflammation. Remember that you should always ask your doctor before taking any supplements. Some that might be helpful for protecting your heart, which you can discuss with your doctor include: Antioxidants like vitamin C and vitamin E, omega-3 fatty acids, coenzyme Q10, vitamin D and herbs like garlic, gingko, ginseng and hawthorn.
5. Manage Edema (Fluid Retention) and Swelling
Monitor edema by weighing yourself each morning, looking for sudden increases that point to fluid build-up. Weight gain of about three or more pounds that either appears suddenly or keeps creeping up over several days can mean that congestion and edema is building in your lungs, legs or abdomen. This can indicate that heart failure may be getting worse. If you notice this happening, especially along with other symptoms like shortness of breath or chest pain, then visit your doctor right away.
Limit the amount of fluids you drink in order to prevent edema from worsening. You can ask your doctor how much he or she recommends. Temporarily, you may need to limit the amount of water you drink. So if you feel thirsty, try rinsing your mouth with water, taking very small sips, sucking on frozen grapes or ice chips, chewing gum or your brushing your teeth.
6. Exercise with Caution
Exercise is a great way to prevent inflammation and boost immunity, but if you already have a heart condition, such as a heart arrhythmia, you need to clear exercise with your doctor first. Use caution when beginning exercise again during recovery and don’t do more than your doctor advises. If you notice shortness of breath, pains or fatigue, then you’re likely doing too much and should rest before gradually reintroducing exercise. Take breaks throughout the day to rest and relax. Avoid very strenuous activity that makes it hard to breathe, instead focusing on soothing activities like walking, swimming, light cycling and stretching.
Precautions
Head to either the emergency room of your doctor right away if you experience any signs or symptoms of myocarditis, especially shortness of breath, edema or chest pains. Following surgery, a virus or bacterial infection, or a flare-up in autoimmune disease, be extra careful to look for any signs of myocarditis. Symptoms can progress quickly and be deadly, so always go to the emergency room is you suspect there’s a problem with your heart.
Final Thoughts
- Myocarditis is a disease marked by inflammation and damage of the heart muscle.
- Symptoms don’t always occur, but can include those similar to a heart attack such as chest pains, trouble breathing and heart palpitations.
- Myocarditis can increase the risk for scar tissue developing on the heart, a heart attack, heart failure or stroke.
- The most common causes of myocarditis are viral infections, autoimmune diseases, bacterial infections, drug or medication use, or, rarely, tick/insect bites.
Read Next: Angina + 8 Natural Ways to Help Relieve Mild Chest Pain
