This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Prevent & Treat MCI (Mild Cognitive Impairment) Naturally
August 24, 2017
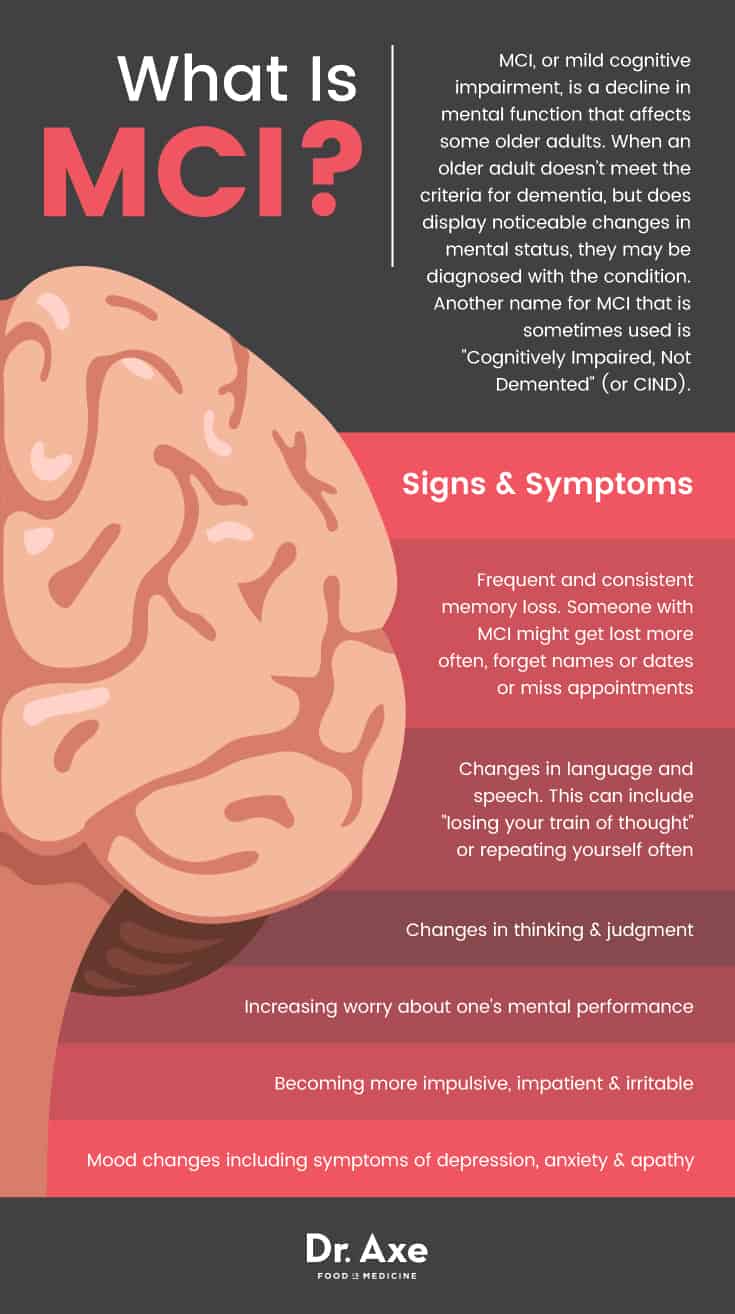
It’s very common, and even considered “normal,” to experience some lapse in memory and mood changes as you age. For some older people, however, forgetfulness and changes in thought processing becomes more serious due to alterations that take place in the brain. When an older adult doesn’t meet the criteria for dementia, but does display noticeable changes in mental status, they may be diagnosed with the condition called mild cognitive impairment (or MCI).
It’s estimated that between 16–20 percent of adults over the age of 60 will develop MCI at some point. This can increase their risk for progressing to dementia. What are some of the ways that symptoms of MCI can be prevented or reversed? According to the Alzheimer’s Association, “Some of the most active areas of research in risk reduction and prevention include cardiovascular factors, physical fitness, and diet.” (1)
What Is MCI?
MCI, or mild cognitive impairment, is a decline in mental function that affects some older adults. The Mayo Clinic states that “Mild cognitive impairment (MCI) is an intermediate stage between the expected cognitive decline of normal aging and the more-serious decline of dementia.” (2) Compared to dementia or other cognitive disorders such as Alzheimer’s disease, MCI is usually not severe enough to require treatment or interfere with someone’s day-to-day life.
Another name for MCI that is sometimes used is “Cognitively Impaired, Not Demented” (or CIND). According to a 2013 report published in Clinics in Geriatric Medicine, MCI is characterized by both changes in memory and also non-memory cognitive (thinking) domains. Currently the criteria for diagnosing MCI includes: (3)
- Cognitive complaints from the patient.
- Decline or impairments in thinking compared to earlier in life.
- Objective evidence of impairment in cognitive domains, such as from family members or close friends.
- Mostly normal functional activities (as compared to those with dementia).
MCI Causes & Risk Factors
Does having mild cognitive impairment mean that someone is likely to develop Alzheimer’s or dementia? Not necessarily, although it’s possible. MCI does increase someone’s risk of progressing to dementia or developing another neurological condition. (4) However, this isn’t always the case as some people with MCI never develop more serious symptoms. In fact, it’s even possible in some cases for MCI symptoms to lessen and improve with time. (5) Overall evidence indicates that about 20 to 40 percent of older adults who have MCI will wind up developing dementia (compared to about 3–5 percent of the general adult population). An estimated 20 percent of those with MCI will improve over time.
Experts believe that MCI is due to neurological changes, although it’s still unknown exactly why and how these develop. Contributing factors include genetics, free radical damage, an inability to use glucose properly, vitamin deficiencies or environmental toxins. The same types of neurological changes that contribute to Alzheimer’s disease or dementia are also believed to be the main cause of MCI. Changes that can take place in the brain and central nervous systems (CNS) of people with MCI may include:
- Decreased blood flow/circulation to the brain. This can contribute to small strokes, which sometimes become more frequent but can hardly be detected.
- Decreased use of energy (in the form of glucose) by brain cells.
- Shrinkage in the hippocampus. The hippocampus is a region in the brain that is tied to memory, emotions and other functions.
- Enlargement of ventricles, or fluid-filled sacs in the brain.
- Neuronal injury.
- Decreased cerebrospinal fluid.
- Increased plaque, or clumps of beta-amyloid proteins and Lewy bodies (other types of proteins).
- Small strokes or reduced blood flow through brain blood vessels.
There are a number of risk factors that have been shown to increase the risk for MCI, as well as other neurological conditions. These include:
- Older age.
- Family history of conditions such as Alzheimer’s or dementia. Some people are predisposed to these conditions due to having a gene known as APOE-e4, which increases the risk for cognitive problems, but does not necessarily guarantee that one will develop.
- Having a history of diabetes, cardiovascular disease, stroke or metabolic syndrome risk factors, such as high blood pressure and high cholesterol. These conditions can interfere with blood flow to the brain and worsen inflammation. Some studies have found a link between these conditions and worsened memory and moods.
- Being a smoker, drug user or having a history of alcoholism.
- Suffering from mental health problems including depression, social anxiety and isolation. These conditions tend to make “brain fog” and forgetfulness worse, plus they can lower someone’s motivation to stay active, be social, and to take care of themselves.
- A sedentary lifestyle, or lack of physical exercise. Exercise has been shown to help control inflammation and is beneficial for mental health in many ways.
- Lower income.
- Lack of social support and strong relationships, which are correlated with better mental health in older adults. Older adults living in the “Blue Zones,” who sometimes live to be 100 or beyond, are a great example of how positive social interactions can be protective of health.
- Lack of sleep, along with sleep-related problems like sleep apnea.
Symptoms of MCI
Signs and symptoms of MCI fall somewhere between those associated with “typical aging,” and those associated with Alzheimer’s disease and dementia. For example, someone with MCI may forget about appointments from time to time, or use the wrong words when speaking. In comparison, someone with Alzheimer’s may forget who someone close to them is, not be able to manage their finances, and lose track of what season it is. (6)
Some of the most common signs and symptoms of MCI include:
- Frequent and consistent memory loss. Someone with MCI might get lost more often, forget names or dates or miss appointments.
- Changes in language and speech. This can include “losing your train of thought” or repeating yourself often.
- Changes in thinking and judgment.
- Increasing worry about one’s mental performance.
- Becoming more impulsive, impatient and irritable.
- Mood changes including increased symptoms of depression, anxiety and apathy.
Conventional Treatments for MCI
There is still a lot that is unknown about how memory loss, dementia and Alzheimer’s develop, as well as the very best ways to prevent them. At this time, the goal of treating patients with MCI is to manage symptoms, improve quality of life and stop the disorder from progressing. There is no standard MCI treatment plan or drugs that doctors use to treat patients. So each case is handled a bit differently. Depending on how much symptoms interfere with someone’s quality of life, certain doctors may choose to prescribe cholinesterase inhibitors to adults with MCI. Cholinesterase is a type of drug approved for Alzheimer’s disease, so it might help to prevent MCI from worsening.
Prevention & 5 Natural Treatments for MCI
1. Anti-Inflammatory Diet
A “whole foods” diet that’s high in antioxidants from veggies and fruit, along with adequate healthy fats, is supportive of mental health in both younger people and aging adults. Elements of two popular dietary plans that are known to promote cardiovascular health — the Mediterranean diet and the DASH diet — have been combined to form what’s known as the “MIND Diet.” The MIND diet is believed to help slow cognitive decline because it’s nutrient-dense and high in fiber and antioxidants like resveratrol, quercetin, flavonoids and beta carotene. (7) The following MIND diet foods have been shown to help protect the brain from inflammation and may decrease the risk for mild cognitive impairment:
- High-antioxidant foods including leafy green veggies, berries, cruciferous veggies like broccoli or cauliflower, and orange and yellow veggies like peppers, squash, pumpkin and carrots.
- Wild-caught fish that are high in omega-3 fatty acids, such as salmon, mackerel and sardines. Additionally, astaxanthin, a carotenoid antioxidant found in wild-caught salmon, can support brain health.
- Healthy fats including olive oil, avocado, nuts and seeds.
- Lean proteins including eggs, legumes, beans and pasture-raised poultry.
- 100 percent whole grains (for those who can tolerate them well).
- Wine and coffee, in moderation.
One study published in the Journal of the Alzheimer’s Association found that people eating the most MIND diet foods on average sustained cognitive health for 7.5 years longer than those eating the fewest MIND foods. (8) As part of the MIND diet, limiting, or even eliminating, inflammatory foods is recommended including: processed meats and factory-farm raised red meat, butter and stick margarine, cheese, pastries and sweets, and fried or fast foods.
In order to reduce your intake of pesticides and potentially harmful chemicals found in the food supply, it’s best to buy organic food whenever possible — including grass-fed meat, wild-caught fish and organic produce. Try to avoid eating non-organic produce imported from countries that still use chemicals like DDT, which has been linked to higher risk for Alzheimer’s disease. If don’t have access to a variety of organic foods, at least try to avoid buying “the dirty dozen” when buying non-organic foods. These are the 12 most pesticide-laced foods. You can refer to this list of the dirty dozen.
2. Exercise & Staying Active
Exercise is beneficial for circulation and has been shown to offer protection against memory loss and other cognitive symptoms tied to aging. Walking, especially outside when the weather allows, seems to be one of the best types of exercise for mental health. (9) When researchers involved in one study tested the effects of brisk walking on older adults’ mental health they found that walking helped reduce activation in certain parts of the brain (the left lateral occipital cortex and right superior temporal gyrus), which contributed to significant improvements in cognitive task performance. Other types of beneficial exercises that are suitable for older adults include swimming, cycling, yoga or using an elliptical. Whichever type you choose, aim to exercise at least 3–4 times per week for about 30–60 minutes at a time. Try to move briskly enough to raise your heart rate to about 65 percent of your maximum capacity.
3. Supplements
- Omega-3 fatty acids — Omega-3s have anti-inflammatory effects that are associated with better mental health.
- Vitamin D3 — Certain studies have found that people who are severely vitamin D deficient seem to be at an increased risk of dementia. To prevent deficiency, try to get regular sun exposure on your bare skin. If this isn’t enough, you may need to supplement, but make sure it’s with vitamin D3 for the best absorption. Aim for about 5,000 IU daily, unless directed by your doctor to take another dose.
- CoQ10 — Some research indicates that because CoQ10 levels decline with age, supplementing may help to slow down the progress of cognitive impairment. Start with a dose around 200 milligrams daily.
- Ginkgo Biloba and Ginseng — While they haven’t been proven to work for all patients, the herbs ginseng and ginkgo biloba may help improve circulation and are tied to enhanced energy, retention of memory and other cognitive benefits. Take 120 milligrams daily to start.
- Phosphatidylserine — Phosphatidylserine plays a role in cellular structures and is key in the maintenance of cellular function in the brain. Supplementing may improve brain cell communication and memory, and it’s shown to be beneficial for early-stage Alzheimer’s disease. Take about 300 milligrams daily.
- Other nutrients including copper, B vitamins, folate and vitamin E may also be protective against cognitive decline. Try to get adequate amounts from a balanced diet. Or consider taking a high-quality multivitamin to make sure your needs are covered.

4. Social Support
Evidence indicates that people with strong social networks, close relationships, a sense of direction and purpose in life, and positive feelings regarding past accomplishments, have better protection against cognitive impairment and are overall happier in life. What are some ways that older adults can stay connected to their communities and increase meaning in their life? Examples include:
- spending more time with family members
- joining a support group to deal with stress
- staying active by walking or exercising with friends
- playing an instrument
- reading and writing
- volunteering with a group in need
- joining a religious organization
- engaging in any other fun hobbies (ideally those that can be done socially)
- “memory training” activities may also slow down cognitive impairments by offering stimulation that helps support mental function
5. Reducing Certain Medications & Toxin Exposure
Smoking cigarettes or using other tobacco products, along with taking certain medications, is known to increase the risk for memory loss and dementia. There’s even evidence that some common allergy, antidepressant, antispasmodic, antipsychotic, and sleep medications may be linked to dementia. If you’re at risk for cognitive impairment, it’s definitely worth speaking to your doctor about how you can replace medications like Benadryl®, Dramamine®, Advil PM® and Unison® with others that don’t pose the same risks.
These drugs have been found to have anticholinergic effects. This means they block the neurotransmitter called acetylcholine in the central and the peripheral nervous systems. This leads to decreased parasympathetic activity and changes in moods, muscular and motor control in the brain. (10). Studies have found that older people using anticholinergic medications at the minimum effective dose for at least three years are at highest risk for side effects including cognitive impairment. A study published in Therapeutic Advances in Drug Safety states that:
Given this potential risk and the myriad of other well-known adverse effects (i.e. constipation, blurred vision, urinary retention, and delirium) associated with anticholinergic medications, it is prudent for prescribers and older adults to minimize use of these medications and consider alternatives when possible. (11)
Precautions Regarding MCI
People with mild cognitive impairment can typically take care of themselves for the most part and don’t require around the clock assistance. However, if MCI starts to progress and symptoms worsen, increased supervision might be needed to prevent an accident or emergency.
To monitor progression of MCI, keep up with regular doctors’ visits. Signs such as frequent confusion, wandering around lost, and poor judgment can signal that treatment, therapy and/or increased supervision from a caregiver or professional is needed. It helps people with cognitive impairments to have an organized schedule, to live in a home that has been checked for safety, to have written to-do list/checklists and to get frequent reminders of events and appointments. Someone who is close to the person should also be within close contact in case of an emergency.
Final Thoughts on MCI (Mild Cognitive Impairment)
- MCI, or mild cognitive impairment, is a decline in mental function that affects about 16–20 percent of older adults, especially those with a history of diabetes, heart disease, smoking, mental illness or neurological conditions.
- MCI causes symptoms related to memory loss, personality or mood changes and increased trouble performing everyday tasks. However, symptoms are not severe enough to greatly interfere with quality of life. And they do no meet the criteria for dementia or Alzheimer’s disease.
- Prevention and treatment for MCI includes eating a healthy diet, exercising, avoiding exposure to cigarettes and harmful medications or drugs, and staying socially engaged.
