This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
How to Get Rid of Varicose Veins: 11 Natural Remedies
April 27, 2025

Although we tend to think of them as a woman’s problem, both men and women develop varicose veins, those bulgy veins that appear lumpy and dark in color (usually blue or purple). In fact, it’s believed that about 50 percent to 55 percent of women and 40 percent to 45 percent of men in the U.S. suffer from some sort of vein problem, with varicose veins affecting about half of all people 50 years and older. This naturally leads many people to explore how to get rid of varicose veins.
They’re a common problem among older or pregnant women due to hormonal influences, and they tend to develop over time as someone ages and veins lose their natural elasticity due to rising levels of inflammation.
Women are at least twice as likely as men to develop varicose veins, but people of any age and race can be affected. They’re usually most noticeable on, and therefore the biggest concern for, people with light skin.
There are a number of different ways to prevent and treat varicose veins, ranging from expensive surgeries to using natural essential oils. Before turning to irritating prescription creams or expensive laser surgeries, which aren’t always effective and should really be considered last-resort options, it’s a good idea to try varicose veins home remedies first to lower the visibility of bulging veins without much risk involved.
Keep reading to learn more on how to get rid of varicose veins.
What are varicose veins?
Varicose veins are swollen, twisted veins that develop when blood pools due to weakened vein valves. Normally, veins carry blood back to the heart, but when the valves in the veins malfunction, blood can flow backward and accumulate, leading to the characteristic bulging appearance.
Varicose veins are a common condition affecting millions of people worldwide. These enlarged, twisted veins typically appear on the legs due to the pressure from standing and walking and can cause discomfort, swelling and aching sensations.
While often considered a cosmetic concern, they can also indicate underlying circulatory issues. That’s why many people look for treatment options.
If you’re wondering how to get rid of varicose veins, there are natural remedies and medical treatments available to help reduce their appearance and symptoms.
Causes and symptoms
What causes varicose veins?
Common causes include:
- Genetics (family history of varicose veins)
- Prolonged standing or sitting
- Obesity, which increases pressure on the veins
- Pregnancy, due to increased blood volume and hormonal changes
- Aging, which weakens vein walls and valves
- Lack of physical activity, leading to poor circulation
What are the symptoms of varicose veins?
Some of the symptoms are:
- Visible, swollen veins that appear blue or purple
- Aching, throbbing or heavy sensation in the legs
- Swelling in the lower legs and ankles
- Itching or irritation around the affected veins
- Muscle cramps, especially at night
- Skin discoloration around the veins
The reason varicose veins appear blue is because they hold deoxygenated blood. They develop on the legs most often (especially the thighs and calves), but since any vein can become varicose, they also show up on other parts of the body at times, including the face, stomach or lower back.
Who gets varicose veins most? According to the Interventional Radiology & Surgery Department at the Hospital of the University of Pennsylvania, the people most likely to develop varicose veins are:
- older people, specially those over the age of 50
- people who are overweight or obese
- people who have jobs that require them to sit or stand for many hours, allowing blood to “pool” in the legs or blood flow to slow down
- those with low levels physical activity and a sedentary lifestyle
- people with poor circulation and high levels of inflammation, caused by things like a poor diet, lack of exercise, injuries to the limbs, hormonal imbalances and high amounts of stress
- pregnant women or those who have recently given birth
- teens going through puberty, women on birth control pills or women going through menopause
- those with family members who have had varicose veins
- people with light skin who have experienced high levels of sun exposure and skin damage
In addition to developing unsightly veins, people with varicose veins sometimes struggle with symptoms like fatigue, muscle aches and “heavy limbs.”
Most dermatologists will tell you that there’s no singular cause for varicose veins, although the mechanism by which they develop is well-understood. The underlying reason that varicose veins form is because veins become stretched and filled with stagnant blood.
As the Vascular Disease Foundation described it, “Under the pressure of gravity these veins continue to expand and, in time, they may become longer, twisty, pouched, thickened and painful.”
Normally blood travels from the heart around the body to various cells through a network of arteries and capillaries. It then returns to the heart through veins, which normally only move blood in one direction.
Movement of muscles helps squeeze veins, which pumps blood back to the heart. (One reason regular exercise is beneficial for circulation.)
Veins contain one-way valves that have a built-in mechanism in place to help prevent blood from flowing in the wrong direction, but in varicose veins a portion of the blood starts moving backward, which causes swelling. Weakness in the valves of veins contributes to poor circulation, although it’s not entirely understood why some people’s valves malfunction more than others.
As blood starts pooling in varicose veins, the walls of the veins become stiff and lose some of their natural elasticity and ability to pump blood back to the heart effectively.
Because varicose veins form where valves stop working properly, they often show up around deep or perforated veins. The great saphenous vein, sometimes also called the long saphenous vein, is a large, subcutaneous vein within the legs that is one of the most common to trigger varicose veins.
This problem of blood pooling in certain veins is called venous insufficiency, and it winds up expanding the vein as blood stays stagnant and the vein hardens.
Some of the underlying reasons this process of blood pooling might occur is because of risk factors like:
- Hormonal changes, such as pregnancy or menopause: Studies have suggested that women are more likely to develop varicose veins than men due to hormonal effects. The belief is that female-dominant hormones tend to relax the veins more often and increase the likelihood of blood leakage, especially during pregnancy, puberty, when taking birth control pills or during the transition into menopause. Pregnant women also produce an increased amount of blood to support the growing baby and are therefore susceptible to blood pooling in the legs or near the stomach as it tries to fight against the force of gravity and pressure.
- Structural (congenital) abnormalities of the veins
- Inflamed veins or blood clots within the veins
- Injuries to the veins, heart disease or an obstruction that blocks normal blood flow
- Weight gain: Circulation can slow when someone gains weight if that person also experiences increased inflammation, plus the veins come under more pressure when a higher body weight needs to be carried around.
Are varicose veins a serious problem and something to worry about?
Most of the time, varicose veins won’t cause symptoms and are a cosmetic issue, not one that’s likely going to contribute to more serious health problems. The amount of blood that pools in the veins is small, and most blood is still being sent back to the heart.
However, you can think of them as a warning sign that something is impairing normal blood flow.
In some cases, varicose veins can actually rupture and cause complications like open sores on the skin and swelling. When painful symptoms are present, the most common are muscle aches or swelling in the ankles and legs, which can make it hard to get comfortable sleep, work, exercise and walk normally.
Some people, especially pregnant women, also wind up developing heaviness or fullness in the legs, restlessness, fatigue, pain, cramps, skin ulcers and itching, and thickening and discoloration of skin. There’s also a small risk that varicose veins will lead to blood clotting (thrombophlebitis), in which case immediate treatment will be necessary.
According to a 2012 report published in the Journal of the American Medical Association, “treatment options for varicose veins range from conservative (e.g., medications, compression stockings, lifestyle changes) to minimally invasive (e.g., sclerotherapy or endoluminal ablation), to invasive (surgical techniques), to hybrid (combination of ≥1 therapies).”
A 2007 report published in the Journal of the Royal College of Surgeons of England found that nerve injuries following varicose vein surgeries are common and that more than half the patients treated will develop some recurrent varicose sites within 10 years of surgery.
Varicose veins are a symptom of an underlying venous insufficiency disorder. This is true whether or not you experience other symptoms like pain and swelling.
If you visit a dermatologist or doctor to talk about treatment options, you’ll likely be advised to make certain lifestyle modifications first, before surgery or other treatments are even considered. These can greatly help decrease blood pooling in your veins, while also offering many other perks, like more energy, clearer skin, better heart health and improved digestion.
The best part is that natural remedies pose little to no risk and are far less expensive than surgeries too, so if you’re wondering how to get rid of varicose veins, starting with natural treatments is a great idea.
How to get rid of varicose veins naturally
If you’re looking for natural ways for how to get rid of varicose veins, several lifestyle changes and home remedies can help improve circulation and reduce symptoms.
1. Exercise
Regularly getting exercise is one of the best things you can do to improve blood flow and lower inflammation, which you can add to the extensive list of exercise benefits. The National Heart, Blood and Lung Institute has stated that sitting (especially with poor posture, like forward head posture, or your legs crossed) or standing for long periods of time without moving around much is associated with an increased risk for varicose veins and other forms of blood pooling.
When you stay stagnant for too long, it’s harder for your veins to pump blood efficiently back to your heart and fight the effects of gravity. Exercise is also a great way to help balance hormones naturally, lose weight or maintain a healthy body weight, and lower blood pressure, which can all contribute to varicose veins.
Experts recommend preventing varicose veins by performing leg lifts, calf raises, bicycle legs and side lunges to strengthen and stretch the veins around the legs. Low-impact exercises, such as walking, swimming and bicycling, are also ideal for varicose vein sufferers since they alleviate pressure.
If you experience pain when starting to exercise, take it slowly, and try icing or heating sore muscles after a workout. You can also elevate your legs to help decrease swelling and pain, or try compression stockings to create gentle pressure up the leg that keeps blood from accumulating.
2. Maintaining a healthy weight
People who are overweight are more likely to develop varicose veins, especially overweight women and elderly people. Carrying excess body weight puts higher amounts of pressure on your veins and can contribute to inflammation or reflux, especially in the largest superficial veins, such as the saphenous vein in the legs.
According to a report published by the Huffington Post about the connection between obesity and varicose veins, for overweight people varicose veins are often more difficult to assess and treat because they commonly go unnoticed until they progress to be more inflamed and larger in size (up to four or five centimeters long, deep inside the leg).
3. Essential oils to balance hormones
Many different essential oils are beneficial for improving blood flow while also lowering inflammation and hormonal imbalances. One of the best for specifically treating vein problems is cypress oil, which has the ability to increase circulation and support the circulatory system.
Try rubbing five drops of cypress essential oil on the problematic area twice daily for several weeks. If you experience muscle aches, swelling or skin blisters, try using other diluted essential oils like peppermint, tea tree and lavender oil in small amounts to soothe problem areas.
4. Anti-inflammatory diet
Certain foods help reverse inflammation and improve blood flow, making it possible to treat varicose veins faster and prevent future ones from forming.
A poor diet, high in things like trans fats, sugar, caffeine, alcohol and processed foods, can contribute to arterial damage, low circulation, blood pressure problems, hormonal imbalances and weight gain. Many of these foods are also high-sodium foods, which are dehydrating, and contain toxins that can worsen swelling in varicose veins.
Some of the best anti-inflammatory foods for reducing the appearance of varicose veins include:
- High-fiber foods. Fiber helps improve heart health and is also necessary for healthy digestive functions. Eating 30 to 40 grams of fiber every day is a great way to prevent constipation, which can cause bloating and increased pressure on the veins around the abdomen and legs. High-fiber foods to eat include chia seeds and flaxseeds, (which are also omega-3 foods,), vegetables, fresh fruit, and soaked/sprouted legumes and ancient grains.
- High-antioxidant foods. Antioxidants, such as flavonoids (present in berries), vitamin C and vitamin E (both present in green veggies and citrus fruits), help strengthen veins, fight inflammation and improve arterial health. Vitamin E is known to help prevent blood clots, acts like a natural blood thinner and is tied to heart health. Vitamin C is a powerful anti-inflammatory and beneficial for skin health.
- Natural diuretics. Doctors sometimes use diuretic pills to help increase urination and reduce water retention or swelling. You can get the same effect safely by consuming things like fresh herbs (parsley, cilantro, basil), fennel, dandelion greens, cucumber, asparagus and celery.
- Magnesium-rich foods. Blood pooling, blood pressure problems and leg cramps (like restless leg syndrome) are warning signs of deficiencies in electrolytes like potassium and magnesium. To overcome these symptoms, increase intake of things like leafy greens, avocado, bananas, cruciferous veggies and sweet potatoes.
- Spicy foods. Foods with spices, such as cayenne pepper or curry, help heat up the body and get blood flowing, adding to healthy circulation and even appetite/weight control.
- Wild-caught fish. Fish and seafood like wild salmon, mackerel, anchovies, sardines and tuna provide omega-3 fatty acids, which are important for proper blood flow.
- Apple cider vinegar (ACV). ACV improves circulation in the vein walls and is an effective anti-inflammatory. Many people find that using ACV along with witch hazel on varicose veins helps lower swelling and improves their appearance within just a few weeks.
5. Natural herbs
Bilberry and horse chestnut, two plants that are thousands of years old and popular folk remedies, have been found to be both effective and safe for treating varicose veins. Both have been studied for chronic venous insufficiency that causes pain, ankle swelling, feelings of heaviness, itching and nighttime leg cramping.
They’re also beneficial for lowering water retention, circulatory problems, swelling, diarrhea, PMS cramps and other skin-related conditions.
The fruit of the bilberry plant can be eaten or made into extracts or tea. The horse chestnut tree (sometimes called buckeye) produces seeds, leaves, bark and flowers that can be found in extract, cream/lotion, tea or capsule form.
Look for horse chestnut seed extract standardized to contain 16 percent to 20 percent aescin (escin), the active ingredient. Horse chestnut should be taken in doses around 100 milligrams once daily.
Taking bilberry in doses of about 160 milligrams, twice daily, is recommended.
In addition, you can combine these with butcher’s broom (200 milligrams daily), grape seed extract (200 milligrams daily) and vitamin E (400 IU daily) to help boost blood flow, protect veins and achieve natural blood-thinning effects safely.
Increasing intake of rutin, a type of bioflavonoid, also may protect the walls of veins and help them work better. Bioflavonoids help relieve swelling, aching and pain from varicose veins and can be found in grape seed, pine bark, cranberry, hawthorn, blueberry and other plants that provide antioxidants like vitamin C.
6. Elevating your legs
Raising your legs above heart level for 15-20 minutes can promote blood flow and relieve swelling. Elevating the legs is a conservative management strategy for varicose veins, aiming to alleviate symptoms by reducing venous pressure and peripheral edema.
A 2019 article in American Family Physician noted that conservative treatments for varicose veins include leg elevation, which can help alleviate symptoms such as a heavy, achy feeling and itching or burning sensations that worsen with prolonged standing. Similarly, a 2008 review listed leg elevation among conservative treatment options for varicose veins, aiming to reduce symptoms and prevent complications.
Another 2019 article in FP Essentials discussed chronic venous insufficiency, noting that leg elevation can relieve symptoms such as leg pain and heaviness, which are associated with varicose veins.
7. Compression socks
Compression stockings are commonly used to manage varicose veins by applying graduated pressure to the legs, which promotes venous return and reduces venous pressure. These specially designed socks improve circulation and reduce vein swelling.
A 2020 study analyzed the impact of compression stocking therapy on the varicose vein wall, finding improvements in endothelial function and reductions in inflammation, oxidative stress and coagulation markers. This suggests that compression stockings may positively influence the vein wall’s health.
8. Stay hydrated
Drinking plenty of water helps maintain healthy blood circulation. Better blood circulation is among the top ways for how to get rid of varicose veins.
9. Massage, naturopathy and dry brushing
Massaging the legs or using a dry brush can stimulate circulation and reduce fluid retention.
A study from 2013 investigated the effects of manual lymphatic drainage (MLD) on patients with chronic venous disease (CVD), which often encompasses varicose veins. The findings indicated that MLD improved clinical stages, hemodynamic parameters and quality of life in these patients.
Another study examined the combined effect of yoga and naturopathy on uncomplicated varicose veins. The results suggested that this combination reduced blood pressure and inflammatory markers, indicating potential recovery in endothelial tissue inflammation within the microvascular system of varicose vein patients.
10. Avoid prolonged sitting or standing
Changing positions frequently prevents blood from pooling in the veins. A 12-year prospective study of the Danish population found that prolonged standing at work increased the risk of hospitalization due to varicose veins by 1.75 times for men and 1.82 times for women, accounting for over one-fifth of all cases among the working-age population.
Another study among Korean workers revealed that prolonged standing at work was significantly associated with an increased risk of varicose veins and nocturnal leg cramps in both men and women. Further research on employees working in prolonged standing or sitting postures showed that 83.4% of those in standing positions and 59.4% in sitting positions exhibited evidence of chronic venous disorders, indicating a higher risk associated with prolonged standing.
Minimizing prolonged static postures may help prevent further progression and alleviate symptoms associated with varicose veins. For individuals with existing varicose veins, it is advisable to incorporate regular movement and avoid extended periods of immobility to manage symptoms and potentially slow disease progression.
11. Non-restrictive clothing
A 2019 article published in American Family Physician recommended wearing non-restrictive clothing as part of conservative treatment options for varicose veins, aiming to reduce peripheral edema and alleviate symptoms.
Another study published all the way back in 1975 observed a low prevalence of varicose veins among a population in New Guinea, noting the absence of factors such as tight clothing that are postulated to be important in other populations.
These findings imply that avoiding tight clothing, which may impede proper blood flow, could be beneficial in managing varicose veins. However, more targeted research is needed to establish a direct causal relationship between non-restrictive clothing and the improvement or prevention of varicose veins.
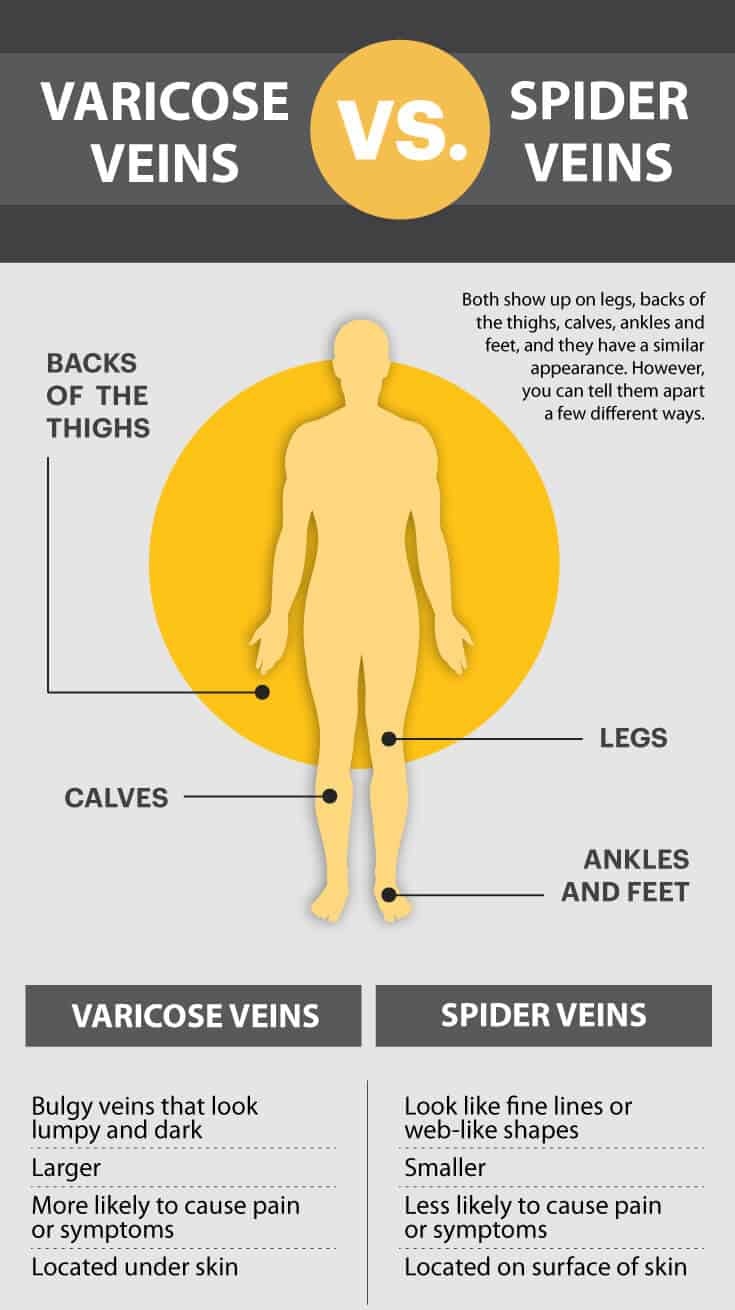
Varicose veins vs. spider veins
While people often use these terms interchangeably, these two skin conditions are actually somewhat different. Their appearances are not exactly the same, although their causes are somewhat similar.
Spider veins (telangiectasias) usually look like fine lines or web-like shapes. Some people describe spider veins as “starbust clusters” since they tend to show up as many dark dots concentrated together in one area, mostly on the surface of the skin.
Just like varicose veins, spider veins normally show up on the legs, backs of the thighs, calves, ankles and feet. Spider veins are usually smaller than varicose veins and not as painful or likely to cause symptoms since they’re located on the surface skin layers.
Another similar condition is called reticular veins, which are larger than spider veins but smaller than varicose veins.
Medical varicose veins treatment
For more severe cases, medical intervention may be necessary. The most effective treatments include:
- Sclerotherapy. A minimally invasive procedure where a solution is injected into the vein, causing it to close and fade.
- Laser therapy. Uses laser energy to seal off smaller varicose veins and spider veins.
- Radiofrequency or endovenous laser ablation. Heat-based techniques that close off problematic veins.
- Vein stripping and ligation. A surgical procedure to remove severely damaged veins.
- Foam sclerotherapy. A foam solution is injected into larger veins to block blood flow and shrink them.
- Phlebectomy. A minor surgical procedure where small varicose veins are removed through tiny skin punctures.
Frequently asked questions
How do you fix varicose veins?
Varicose veins can be treated with lifestyle changes (like exercise, weight loss and leg elevation), compression stockings, or medical procedures, such as sclerotherapy, laser treatments or vein surgery.
Do varicose veins go away?
No, varicose veins typically do not go away on their own. They may improve in appearance with treatments, but without intervention, they often get worse over time.
What is the main cause of varicose veins?
The main cause is weakened or damaged valves in the veins, which leads to poor blood flow and vein enlargement.
Can I live normally with varicose veins?
Yes, many people live normally with varicose veins, especially if the veins are mild and not causing major symptoms. However, if symptoms worsen, treatment might be needed.
What is the fastest way to get rid of varicose veins?
Minimally invasive procedures like sclerotherapy, endovenous laser therapy (EVLT) or radiofrequency ablation can quickly and effectively reduce or remove varicose veins.
When should I worry about varicose veins?
You should be concerned if you experience significant pain, swelling, skin ulcers, bleeding, or if a vein feels hard or hot (which could signal a blood clot).
Are varicose veins dangerous?
Most varicose veins are not dangerous, but in some cases, they can lead to complications like blood clots, skin ulcers or bleeding.
Are varicose veins painful?
They can be. Some people feel aching, throbbing, heaviness or burning sensations in the legs, especially after standing or sitting for long periods.
Final thoughts
- Experts believe about 50 percent to 55 percent of women and 40 percent to 45 percent of men in the U.S. suffer from some sort of vein problem, with varicose veins affecting about half of all people 50 years and older.
- Women are at least twice as likely as men to develop varicose veins, but people of any age and race can be affected.
- Wondering how to get rid of varicose veins? Natural varicose veins treatment includes exercise, maintaining a healthy weight, essential oils for balancing hormones, an anti-inflammatory diet, and natural herbs like bilberry and horse chestnut.
- As part of an anti-inflammatory diet, the best foods to eat to treat varicose veins include high-fiber foods, high-antioxidant foods, natural diuretics, magnesium-rich foods, spicy foods, wild-caught fish and apple cider vinegar.
- Just like varicose veins, spider veins normally show up on the legs, backs of the thighs, calves, ankles and feet. Spider veins are usually smaller than varicose veins and not as painful or likely to cause symptoms since they’re located on the surface skin layers.













