This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Chronic Venous Insufficiency Causes Leg Pain & More (+ 8 Natural Ways to Relieve CVI Symptoms)
May 27, 2018

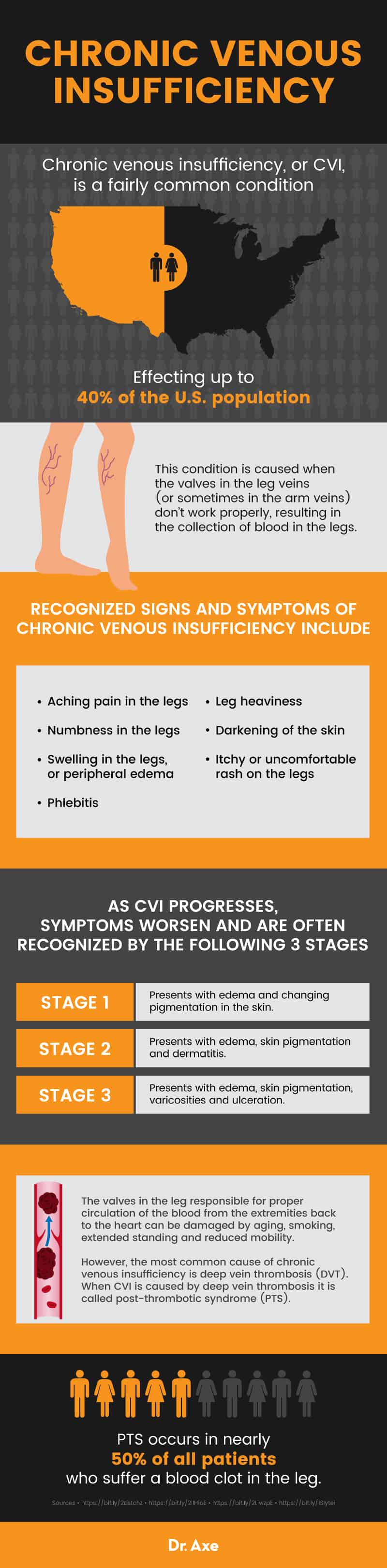
Chronic venous insufficiency, or CVI, is a fairly common condition effecting up to 40 percent of the U.S. population. This condition is caused when the valves in the leg veins (or sometimes in the arm veins) don’t work properly, resulting in the collection of blood in the legs. (1)
As the blood continues to pool in the extremities, it creates pressure within the veins, prohibiting the blood to properly flow back up to the heart. While more common in women — especially after multiple pregnancies — it can occur in anyone, at any age.
Symptoms of chronic venous insufficiency can include swelling in the legs or ankles, a feeling of tightness in the calves, varicose veins and leg ulcers. If this condition remains untreated, serious conditions including blood clots or a pulmonary embolism can occur.
Underlying factors that may increase your risk for developing CVI include obesity, a sedentary lifestyle, a previous injury or trauma to a leg and a job that requires you to spend lots of time on your feet. (2)
Chronic venous insufficiency treatment includes exercise and compression therapy, and, depending on the severity of the case, medical intervention including medications, surgery and chronic venous insufficiency endogenous laser treatments may be necessary. Natural treatments for this condition aim to increase circulation, improving the symptoms.
What Is Chronic Venous Insufficiency?
As the name suggests, chronic venous insufficiency, or CVI, is a condition that occurs when the valves in the veins of the legs aren’t working sufficiently to return blood to the heart, causing the blood to begin to pool in the legs. (3)
The term chronic venous insufficiency relates to a number of conditions within the venous system. Chronic venous insufficiency and varicose veins are closely linked, with varicose veins being both a symptom and a risk factor of CVI. (4)
As CVI progresses, symptoms worsen and are often recognized by the following three stages: (5)
- Stage 1: Presents with edema and changing pigmentation in the skin.
- Stage 2: Presents with edema, skin pigmentation and dermatitis.
- Stage 3: Presents with edema, skin pigmentation, varicosities and ulceration.
The valves in the leg responsible for proper circulation of the blood from the extremities back to the heart can be damaged by aging, smoking, extended standing and reduced mobility. However, the most common cause of chronic venous insufficiency is deep vein thrombosis (DVT). When CVI is caused by deep vein thrombosis it is called post-thrombotic syndrome (PTS).
PTS occurs in nearly 50 percent of all patients who suffer a blood clot in the leg. It is imperative after a DVT to follow all of your physician’s recommendations, including the use of compression therapy to help prevent chronic venous insufficiency from developing. (6)
Signs and Symptoms
Recognized signs and symptoms of chronic venous insufficiency include: (7)
- Aching pain in the legs and calves
- Numbness in the legs
- Swelling in the legs, or peripheral edema
- Leg heaviness
- Darkening of the skin
- Itchy or uncomfortable rash on the legs
- Phlebitis
Causes and Risk Factors
Chronic venous insufficiency can be caused by a variety of factors and recognized risk factors include: (2, 3)
- Deep vein thrombosis or previous blood clots
- Pelvic tumors
- Vascular malformations
- Obesity
- Pregnancy
- Varicose veins
- Family history
- Injury, trauma or surgery of the leg
- High blood pressure
- Lack of exercise
- Standing for long periods
- Smoking
- Phlebitis
- Being over 50
- Being female
Conventional Treatment
Before treatment can begin, your medical team will take your medical history and conduct an imaging test called a duplex ultrasound. This ultrasound allows your physician to examine the structure of the veins in your legs and allows them to monitor the flow of blood. This test will show which veins or valves are compromised and not performing optimally. (2)
Additional tests may include: (8)
- CT scan
- MRI
- Blood tests
- Venograms
Chronic venous insufficiency treatment guidelines are based on your overall health, medical history, symptoms and what stage of CVI you are in.
Treatment recommendations may include:
- Compression socks
- Regular exercise
- Aspirin
- Sclerotherapy, a chemical injection into the veins
- Endovenous laser ablation
- Radiofrequency ablation
- Surgical interventions including ligation or vein stripping
As a special note for chronic venous insufficiency endogenous laser treatments: This is considered a minimally invasive procedure and is commonly used for varicose veins and venous ulcers. However, this procedure is not without risk. The Cleveland Clinic cites bruising, pain, and — the most concerning — the development of a blood clot. (9)
Natural Ways to Manage Chronic Venous Insufficiency
1. If you smoke, quit
Smoking doesn’t just affect your lungs, it damages virtually every organ in the body and your blood vessels. Quitting smoking and avoiding secondhand smoke can help reverse heart and blood vessel damage, according to the NIH’s National Heart, Lung and Blood Institute. (10)
Quitting smoking isn’t easy. Smoking is an addiction that encompasses both physical and mental barriers. Research shows that several mind-body practices can help you quit smoking, reduce cravings and improve mental outlook. Consider yoga, meditation, guided imagery, tai chi and hypnosis, and find the right combination that eases your withdrawal symptoms and helps you kick the nicotine habit for good. (11, 12, 13, 14)
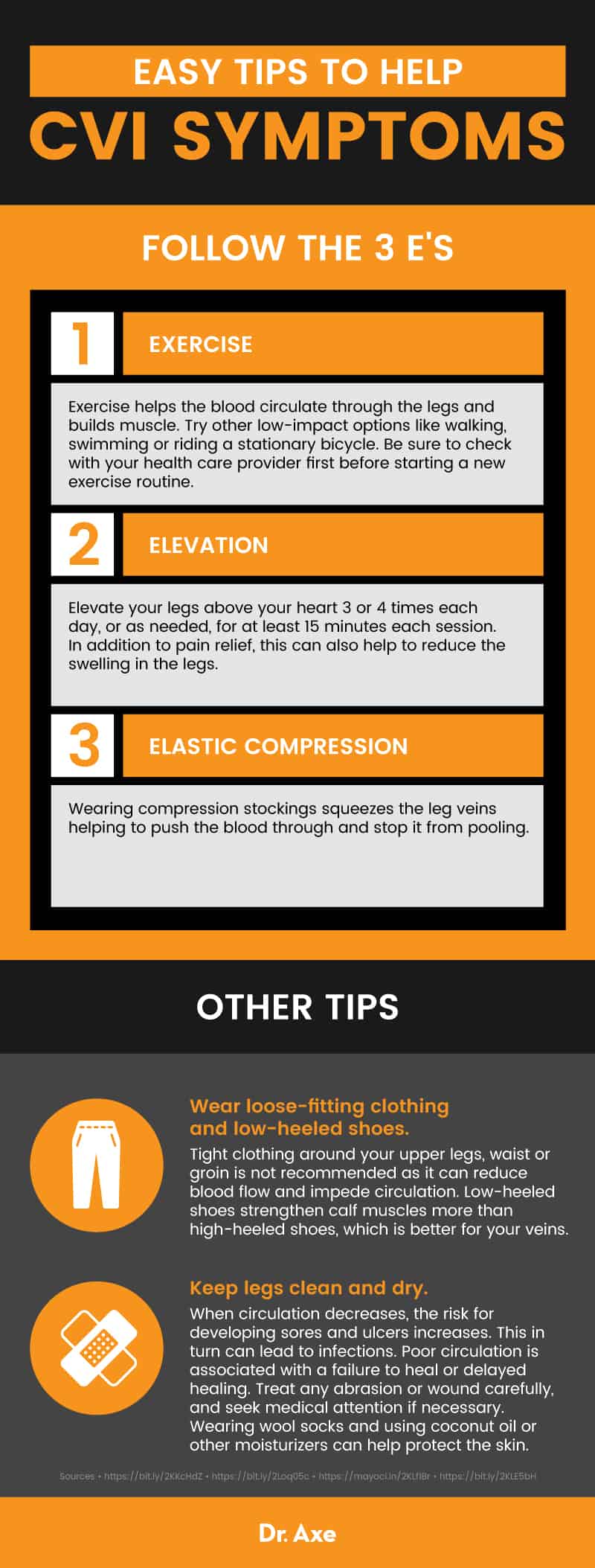
2. Start exercising
Poor circulation in the legs is the hallmark of chronic venous insufficiency. Exercise helps build muscle that promotes better circulation and helps to pump blood from the legs back up to the heart. According to the Cleveland Clinic, walking is particularly helpful for encouraging circulation in the legs for those with CVI. (3)
In addition to walking, other chronic venous insufficiency exercises that may help build leg muscles include low-impact exercise like riding a stationary bike, swimming and ankle exercises using elastic-like bands. (15)
3. Elevate legs three to four times daily
According to UC Davis Vascular Center, many patients with pain due to CVI can experience immediate pain relief when they elevate their legs. The goal is to elevate your legs above your heart three or four times each day, or as needed, for at least 15 minutes each session. In addition to pain relief, this can also help to reduce the swelling in the legs, making them feel less “tight.” (16)
4. Try butcher’s broom
In a small clinical trial of women with CVI, taking a butcher’s broom supplement was associated with an improvement in symptoms and increases the venous refilling time. Additional studies have shown butcher’s broom has pro-circulation benefits, making it one of the top recommended natural treatments for chronic venous insufficiency. (17, 18)
However, butcher’s broom isn’t for everyone. There is not enough evidence to support using butcher’s broom if you have diabetes or digestive problems. It can interact with a variety of prescription medications, including many prescribed for heart conditions, so in these cases it’s best to check with your doctor before taking it. If you take medication for high blood pressure, certain stimulants, or are pregnant or breastfeeding, don’t take butcher’s broom. (19)
5. Take horse chestnut, 400–600 milligrams, in two doses
Horse chestnut has traditionally been used for treating leg cramps, joint pain and digestive upset. However, systematic reviews of horse chestnut used for the treatment of chronic venous insufficiency indicates that it is safe and effective for relieving symptoms. However, the researchers urge larger clinical trials.
Horse chestnut should never be consumed raw as it is poisonous. Select a high-quality supplement, and if you are pregnant, nursing, have a bleeding disorder, digestive problems, kidney disease, diabetes, latex allergy or are recovering from (or planning) surgery, do not take horse chestnut. Always check with your health care provider before taking this or any new supplement.
6. Take proanthocyanidins 50–100 milligrams two to three times daily
This group of flavonoids known as proanthocyanidins were shown to strengthen the capillaries in clinical trials. In this group, black currant, black tea, grape seed, cranberry, bilberry and green tea showed promise in the treatment of chronic venous insufficiency. In fact, a clinical trial found that 100 milligrams taken three times a day showed relief of symptoms and improvement in just four weeks. (20)
7. Wear loose-fitting clothing and low-heeled shoes
Compression socks are often the first recommended conventional course of treatment for CVI, but wearing tight clothing around your upper legs, waist or groin is not recommended as it can reduce blood flow and impede circulation. And, low-heeled shoes strengthen calf muscles more than high-heeled shoes, which is better for your veins. (21)
8. Keep legs clean and dry
When circulation decreases, the risk for developing sores and ulcers increases. This in turn can lead to infections. Poor circulation is associated with a failure to heal or delayed healing. Treat any abrasion or wound carefully, and seek medical attention if necessary. Wearing wool socks and using coconut oil or other moisturizers can help protect the skin. (22)
Precautions
Left untreated, chronic venous insufficiency can cause serious and potentially life-threatening complications, including: (7)
- Deep vein thrombosis
- Pulmonary embolism
- Sores
- Skin ulcers
- Infection
Final Thoughts
- Chronic venous insufficiency is a relatively common circulation disorder that affects up to 40 percent of the U.S. population.
- It is caused when damaged blood vessels or valves in leg veins prevent the flow of blood back to the heart, resulting in pooling of the blood in the legs.
- Risk factors for CVI include obesity, a sedentary lifestyle, previous injury or leg trauma, a job that requires lots of time on your feet, and a previous DVT.
- Chronic venous insufficiency treatment guidelines are based on your overall health, medical history, severity of symptoms and the stage of CVI you have.
- Natural treatments may help relieve symptoms and improve circulation in your extremities.
Read Next: Top 7 Heart-Healthy Foods + How to Follow a Heart-Healthy Diet
