This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Osteopenia: Low Bone Density Risk Factors + 5 Natural Treatments
June 30, 2017
Most of us don’t ever think of our bones as being “living tissue.” But the cells, nerves, blood vessels and minerals that make up our bones are, in fact, always renewing themselves. It’s estimated that around 10 million people living in the U.S. alone currently have osteoporosis, and somewhere between three to five times this amount (an estimated 34–54 million people) have osteopenia, characterized by weak bones and a higher risk for fractures.
What does it mean when you have low bone density? Bones are made up of calcium and other minerals that help keep them strong, or “dense.” We need healthy bone density to support our body weight, protect our internal organs and to help us move. Throughout our lives a process of bone-building and bone-breakdown is always taking place. Lifestyle factors like your diet, level of exercise, body weight and use of medications can impact this process. Research suggests that due to factors like changes in exercise habits, nutrient intake, and sunlight exposure, half of all women and one-quarter of all men over the age of 50 will suffer from some type of bone injury in their lifetime due to osteopenia or osteoporosis.
In the earlier stages of your life, the strength of your bones may be something you mostly take for granted. That is until something happens to them. Here’s something surprising about weak bones: research shows that most fractures occur in people with osteopenia, rather than osteoporosis. Several studies found that between 55–80 percent of all fractures affect men or women who were not considered to have osteoporosis at the time, but rather weaker-than-normal, or even normal, bones. (1, 2) To protect yourself from a fracture or bone disorder as you age, it’s key to eat a nutrient-dense diet and keep up with other healthy habits, such as doing weight-bearing exercises.
What Is Osteopenia?
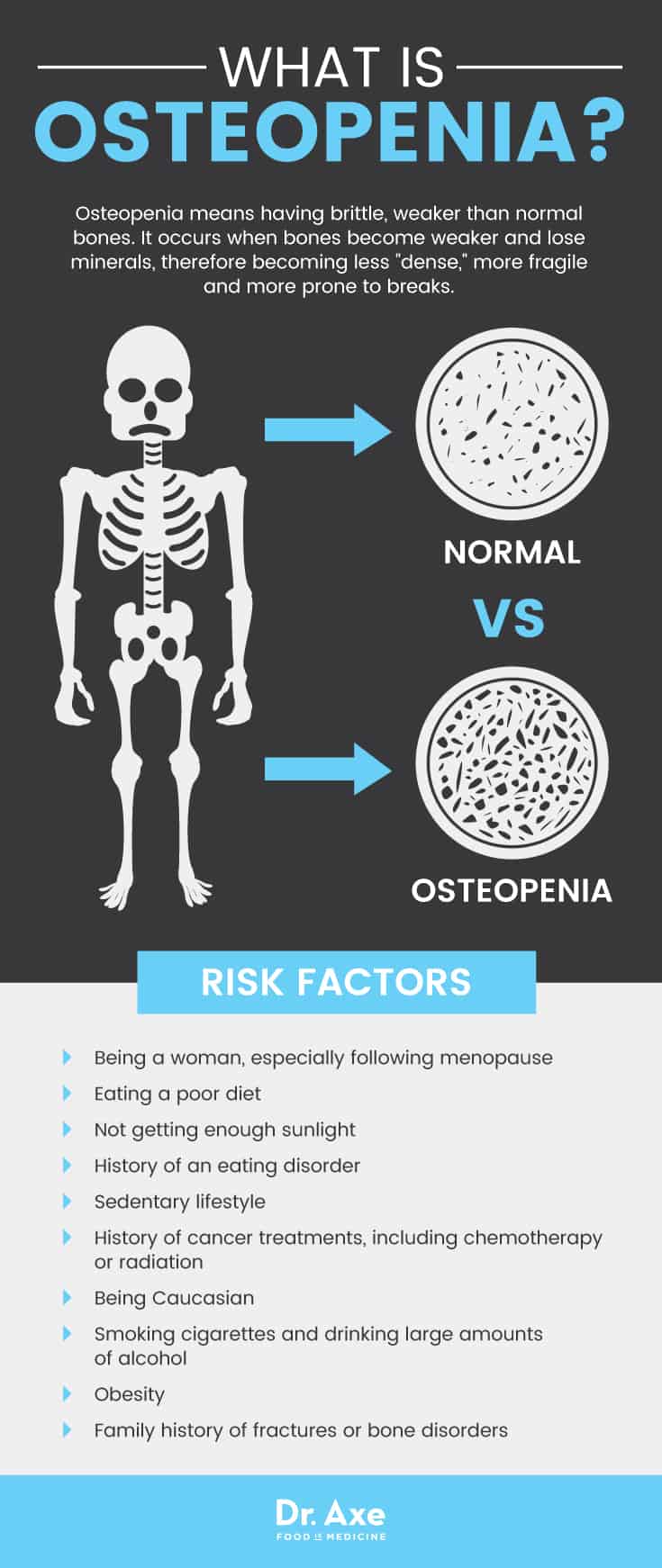
Osteopenia is a condition characterized by lower than normal bone density. In other words, it means having brittle, weaker than normal bones. Is osteopenia a disease? When bone density is not low enough to be classified as osteoporosis, but is not high enough to be considered within a normal range, someone is diagnosed with osteopenia. (3) Osteopenia is more of a relative state or disorder than a disease; it’s really a warning sign that the condition may progress and become worse with time if it’s left untreated.
Osteopenia occurs when bones become weaker and lose minerals, therefore becoming less “dense,” more fragile and more prone to breaks. Bone mass, or bone mineral density, is the amount of mineral content in your bones (or the mineral concentration). Women are much more likely to develop osteopenia and osteoporosis than men. However, both sexes can certainly develop the condition. Women naturally have lower bone density to begin with compared to men. Plus certain reproductive hormones, especially estrogen, affect the rate at which bone mass is created or lost.
Osteopenia vs. Osteoporosis:
- According to the National Osteoporosis Foundation, the definition of osteoporosis is “A bone disease that occurs when the body loses too much bone, makes too little bone, or both.” Osteoporosis means “porous bones.” It’s characterized by large spaces and holes inside the bones’ tissue structure. (4)
- The World Health Organization (WHO) considers osteoporosis to be anything more than 2.5 standard deviations away from normal bone density values. As a comparison, osteopenia is considered “bone density between 1.0 and 2.49 standard deviations (SD) below what would be expected in the average young man or woman,” according to the Better Bones Foundation. (5)
- Having osteopenia puts someone at a greater risk for developing osteoporosis down the road. Typically, osteopenia will occur earlier in life, such as in someone’s twenties or thirties. Then it may progress into osteoporosis years later.
- Having either osteopenia or osteoporosis can make it more likely that bone fractures or breaks will occur. For example, fractures can occur from falling or slipping or when playing sports or exercising. Or, in severe cases, they can occur due to common movements like rolling an ankle when walking, bumping into something, sneezing, etc.
Osteopenia Signs & Symptoms
Many people with osteopenia have no symptoms at all and aren’t aware of their condition. When they do occur, some of the most common osteopenia signs and symptoms include:
- Suffering from one or more bone fractures or breaks. When a bone break occurs, it’s most likely to affect someone’s hip, ankle, the spine or a wrist.
- Dealing with bone pains and other aches that affect tissues near the bones, including the joints.
- Trouble exercising normally due to pains or injuries.
When osteopenia progresses to osteoporosis, symptoms can include losing height/shrinking, due to weakening of the vertebrae (the bones of the spine). Other symptoms of osteoporosis are:
- All of the osteopenia symptoms mentioned above.
- Poor posture, including a stooped or hunched back.
- Limited mobility, reduced range of motion and trouble with everyday tasks due to pain. Many people with severe bone loss need help from an aid or loved one to do things like cook, get around, etc. This can lead to psychological changes such as depression, loss of hope, social isolation, etc.
Osteopenia Causes & Risk Factors
The risk for developing osteopenia and osteoporosis goes up considerably as someone gets older, typically beginning around middle age (in someone’s 30s or 40s). However, some people can start losing bone density at an earlier age, such as people who eat a diet low in key nutrients like calcium; those who chronically under eat or diet; or people who have a history of an eating disorder.
Aging is associated with an increased risk for bone disorders because the rate at which new bone mass is created starts slowing down as someone gets older. After about the age of 30, the time when most people have reached “peak bone density,” both men and women slowly start losing some of their bone density every decade. This is why it’s so important to build strong bones through someone’s teens, 20s and 30s; having a strong skeletal system in the earlier stages of life helps to delay weakening of the bones in older age.
Risk factors for developing osteopenia or osteoporosis include:
- Being a woman, especially following menopause: Certain hormonal changes take place during and after menopause that can contribute to low bone density, such as a decrease in estrogen levels, which help to support strong bones. Estrogen plays an important role in maintaining healthy, strong bones; however, the body produces little estrogen naturally after menopause. Bone density commonly decreases quickly in the first few years after menopause. This is why having strong bones going into menopause is crucial.
- Eating a poor diet: Low intake of foods that provide calcium, along with vitamin D deficiency, are two major contributing factors. Calcium deficiency can affect anybody but is more common among people who avoid all dairy products (such as vegetarians or vegans), eat few fresh vegetables, and consume lots of processed foods. Estrogen levels can also be lower than normal in people who eat a restrictive, low calorie diet.
- Not getting enough sunlight exposure: The best way to prevent vitamin D deficiency is to expose your bare skin to sunlight for about 15–20 minutes every day if possible. Spending most of your time indoors and avoiding the sun may mean that your body isn’t making the vitamin D it needs to help maintain bone mass.
- A history of an eating disorder, female athletic triad, or under-eating for many year: When someone doesn’t consume enough calories or nutrients from their diet the bones can suffer due to there not being enough minerals present in the body to support maintenance of bone mass. This can happen in both men and women, although it occurs in women much more often. Low body fat also interferes with hormone production and can cause decreases in hormones such as estrogen, causing similar effects to menopause in women.
- A sedentary lifestyle or not enough exercise: Exercise, especially “weight-bearing” types, helps bones to maintain their strength.
- Using medications that can weaken bones: Certain medications can interfere with mineral levels in the body, such as calcium, potassium and magnesium. Medications that may increase your risk for osteopenia include steroids such as cortisone and prednisone, asthma treatments, thyroid medications, certain birth control pills (Depo-Provera®), proton pump inhibitors (PPIs), and selective serotonin reuptake inhibitors (SSRIs).
- A history of cancer treatments including chemotherapy or radiation
- Being Caucasian: Research suggests that Caucasians (especially women) develop bone disorders more often than African Americans, Hispanics or Asians do.
- Smoking cigarettes and drinking large amounts of alcohol
- Being obese: Obesity can impact hormone production and also contribute stress to already weak bones.
- Having a family history of fractures or bone disorders.
Conventional Treatment for Osteopenia
How is osteopenia diagnosed? Doctors typically perform a bone mineral density (BMD) test using a special machine to measure bone density and determine if the bones are weaker than expected depending on the patient’s age.
Can osteopenia be cured or reversed, and if so, what’s the best ways to treat it? Doctors commonly use medications to help prevent and treat bone disorders in people diagnosed with osteoporosis by slowing down the loss of bone mass and helping to build new bone. If you have osteopenia, but not osteoporosis, you may not need any treatment and should be working on slowing down the disease’s progression naturally. While they might be helpful, drugs for bone disorders still aren’t usually a total “cure” as the condition tends to worsen with age. Several classes of medications that may be used to slow progression of bone disorders include:
- Bisphosphonate medications, which include alendronate, ibandronate, risedronate and zoledronic acid. One common brand name is Fosamax®.
- Anabolic medications, usually the kind called teriparatide.
- Antiresorptive medications, including calcitonin, estrogen therapy/hormone therapy and an estrogen agonist/antagonist. These may also be called selective estrogen receptor modulators (SERM).
While taking hormone replacement therapy drugs, including birth control pills, is sometimes recommended to protect bones, there is a lot of debate over whether this is actually helpful or effective. Some research has found that while hormone replacements might help slow down loss of bone mass, they don’t help to build bone mass back up in younger people. Using these drugs may be like applying a “Band-Aid®” to an underlying problem, such as a poor diet, without fixing the real root cause. And once you stop taking these drugs the effects stop working, which doesn’t make them a long-term solution.
5 Natural Treatments for Osteopenia
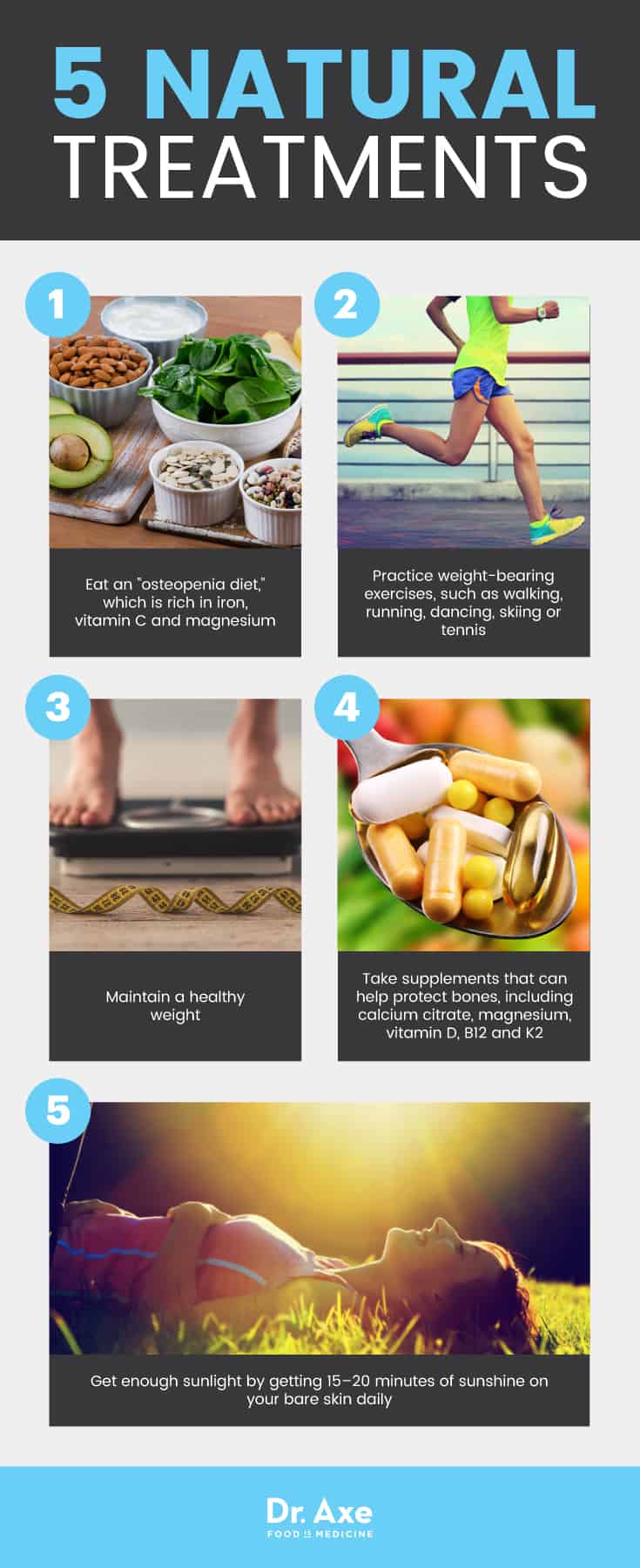
1. Osteopenia Diet
To help you get all the vitamins and minerals you need to build and maintain strong bones, it’s important to eat a varied diet with adequate calories to fuel all your body’s processes. Under-eating for many years, such as to achieve a low body fat percentage or desired weight, can cause osteopenia that results in long-term problems. There are several nutrients that deserve special attention when it comes to supporting bone health, especially calcium and vitamin D.
Other nutrients needed to prevent bone disorders include iron, vitamin C and magnesium. Iron deficiency (anemia) is a risk factor for osteopenia because iron is essential for collagen synthesis and vitamin D metabolism. (6) Vitamin C plays a role in collagen formation. It also helps stimulate the cells that build bones, enhances calcium absorption, and helps vitamin D to work properly. (7)
- Foods that provide calcium include: dairy products like yogurt, kefir or cheese (I recommend, ideally, having raw dairy); salmon or sardines; dark leafy green vegetables; and other veggies like broccoli.
- Magnesium rich foods include: leafy greens like chard or spinach, pumpkin seeds, yogurt or kefir, black beans, cocoa and almonds.
- Sources of vitamin C include: citrus fruits, papaya or guava, berries, peppers, kiwi, broccoli and kale.
- Collagen protein: collagen is one component of bone that helps to build its framework and provide a flexible structure that can withstand pressure. Collagen is found naturally in things like bone broth or can be taken in protein powder form or supplement form.
- And foods that supply iron (which can help to prevent anemia) include: grass-fed meats like beef, bison and lamb, chicken or turkey, fish, eggs, nuts, seeds, spinach, kale and chard.
Overall, aim to consume an alkaline diet that helps protect bones. This means eating lots of veggies, fruit, sea vegetables and plant foods. It’s also best to lower the amount of sodium in your diet by eating more unprocessed/whole foods. It also helps to avoid things like: deli meats, fast foods, fried foods, canned goods, salty condiments or sauces, frozen meals, etc. In addition, try to limit your intake of sugary products, sweetened drinks, alcohol and caffeine.
2. Practice Osteopenia Exercises
To help maintain skeletal strength, it’s important to stay active, including throughout older adulthood. Exercise helps your body reduce the decline in bone mass associated with aging. It has many others benefits, too, such as contributing to hormone balance and a healthy body weight. Exercise is needed to keep muscles strong. It also helps with coordination and balance. This can prevent slips or falls that wind up causing serious fractures or injuries.
Weight-bearing exercises are the most beneficial for your bones, although this term often confuses people. Weight-bearing exercises include any type that “forces you to work against gravity” and that you practice with an upright posture. This way your bones and muscles must support your body weight. (8) Examples include running, walking, dancing, skiing or tennis. Aim to do weight-bearing exercises at least 3–4 times per week for about 30–60 minutes at a time. Or, ideally, do them even more often. It’s also very beneficial to do weight training exercises — using your body weight, free weights or resistance cables/bands — about three times per week for 30 minutes.
3. Take Supplements That Can Help Protect Bones
- Calcium — It’s best to obtain calcium from foods in your diet. However, you can take a supplement if know you’re not getting enough. Most adults need about 1,000 milligrams daily. Choose calcium citrate, which the body absorbs best.
- Vitamin D — Experts recommend that people who have a history of deficiency, elderly adults, those who never spend time outside, and people with dark skin take a vitamin D supplement daily. While dosage recommendations vary a bit, most experts recommend taking about 1,000 IU of vitamin D per day. Older adults who may have trouble synthesizing enough via their skin may need higher amounts.
- Magnesium — Magnesium is a mineral your body requires for proper calcium metabolism. Aim to get between 300–500 milligrams daily.
- Vitamin B12 — This is especially smart for the elderly (who may have a hard time with vitamin B12 digestion due to stomach acid changes) and vegetarians and vegans who likely don’t consume enough from their diets.
- Vitamin K2 — You need vitamin K2 to form a protein that’s critical for bone formation. Take a high quality vitamin K2 supplement or eat more vitamin K-rich foods. When supplementing, take about 100 micrograms daily.
4. Maintain A Healthy Weight
Obesity can increase inflammation and contribute to hormonal changes that damage bones. Maintaining a healthy weight makes it easier to exercise and stay active into older age. Other ways to help reduce inflammation include: quitting smoking, getting enough sleep, controlling stress and not over-consuming alcohol.
5. Get Enough Sunlight
Vitamin D helps improve calcium absorption. It’s best to obtain it via natural sunlight. To allow your body to make enough vitamin D to protect your bones, aim to get 15–20 minutes of sunshine on your bare skin daily.
Precautions Regarding Osteopenia
If you’re at a high risk for osteopenia or osteoporosis, talk to your doctor about having a bone density test. No matter the current state of your bone health, you can work toward preventing fractures or complications by following the advice above. Your doctor can tell you if you need a supplement and what amount will give you the best chance of reversing the problem.
Final Thoughts on Osteopenia
- Osteopenia is a condition characterized by lower-than-normal bone density. It precedes osteoporosis and causes brittle, weaker than normal bones that are more likely to fracture or break.
- Risk factors for osteopenia include: being a woman following menopause; dieting or calorie restriction; eating disorders; taking medications that interfere with mineral absorption; anemia; smoking cigarettes; too little exercise; obesity and a family history.
- Natural treatments and prevention include: eating a nutrient-dense diet with enough calcium and vitamin D; getting enough exercise; maintaining a healthy weight; not smoking; and preventing vitamin D deficiency by getting adequate sunlight exposure.








