This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Gingivitis Symptoms and How to Get Rid of Gum Disease
December 5, 2024

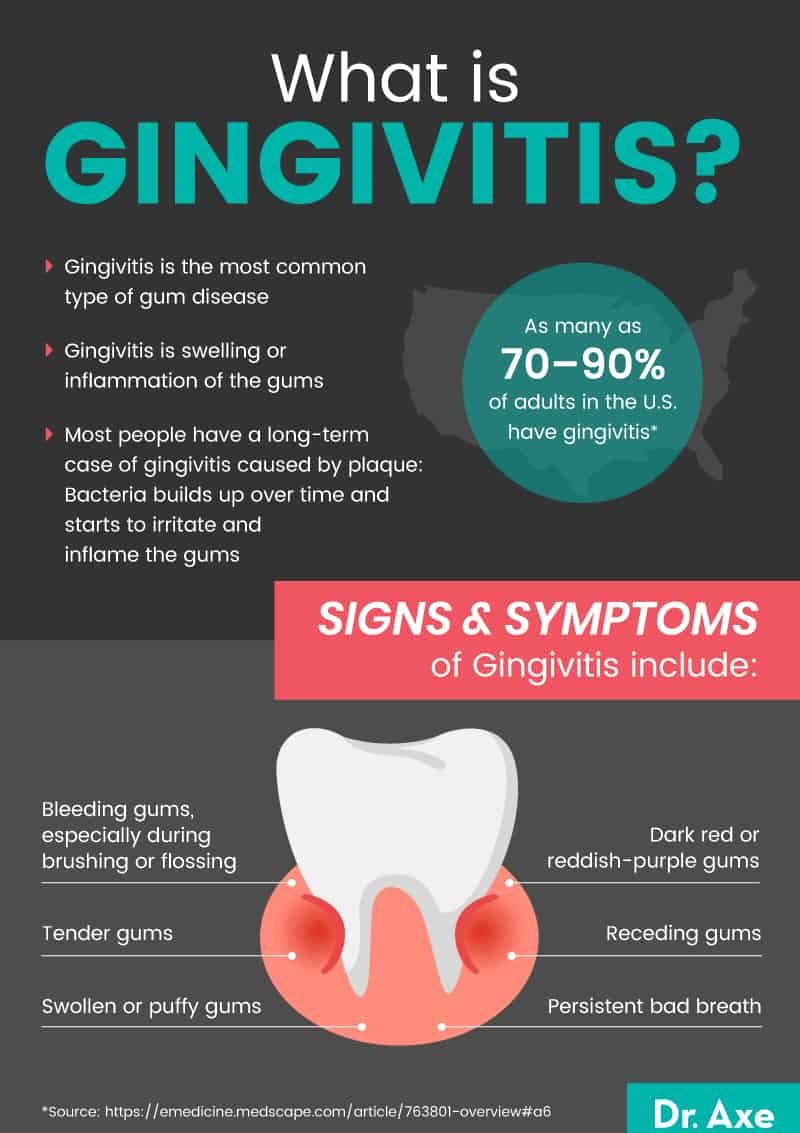
Gingivitis is the most common type of gum disease. It is rare in children but often starts during puberty or early adulthood, and it can come and go throughout life.
According to the Centers for Disease Control and Prevention and the National Institutes of Health, more than 40 percent of U.S. adults have some form of gum disease, including gingivitis.
In most people, it is caused by a buildup of plaque on the teeth and gumline. The good news is it’s usually treatable and can be prevented using natural remedies and proper oral hygiene.
What is gingivitis?
Gingivitis is swelling or inflammation of the gums. It is classified by how it looks, its cause and how long it lasts.
Different types of gingivitis include:
- Ulcerative
- Hemorrhagic
- Necrotizing
- Purulent
- Drug-induced
- Hormonal
- Nutritional
- Infectious
- Plaque-induced
- Acute (short-term)
- Chronic (long-term)
Most people who deal with it have long-term gingivitis caused by plaque. This means that bacteria aren’t properly cleared from the mouth.
The bacteria builds up over time and starts to irritate and inflame the gums.
When plaque and poor hygiene are the problem, the condition can lead to inflammatory gingival enlargement or gingival hyperplasia — meaning a swelling or overgrowth of the gums. Other types of gingival enlargement are caused by medication, health conditions, hormone imbalances or rare genetic conditions.
Gingivitis starts with mild swelling but can get worse over time, causing lesions, mouth pain, tooth loss and other signs of advanced gum disease.
The progression of periodontal disease is:
- Gingivitis — Gums are red, swollen and bleed easily.
- Periodontal pockets — Plaque begins to form below the gum line, gums recede and pockets form.
- Periodontitis — The chronic presence of plaque, tartar and attending bacterial infection destroys the gum and bone structure that supports the teeth and may result in them becoming loose and needing removal.
Is gingivitis contagious?
Yes and no.
According to the American Academy of Periodontology (AAP), the bacteria that cause gingivitis can be spread by kissing, sharing utensils or another exchange of saliva.
However, actually developing gingivitis depends on additional factors, such as how well you clean your teeth. The AAP recommends not sharing toothbrushes or eating utensils with someone who has signs of gum disease.
Causes and risk factors
The most common cause of gingivitis is a buildup of plaque (food and bacteria) on the teeth. The bacteria and the toxins they release then infect and irritate the gums, making them tender and swollen.
Risk factors for gum disease include:
- Poor oral hygiene
- Being 60 or older
- Smoking or chewing tobacco
- Having a genetic risk
- Stress
- Low immunity (for example, in people with HIV/AIDS)
- Taking certain drugs, such as some birth control pills, antidepressants and heart medications
- Clenching or grinding your teeth
- Teeth that fit together poorly
- Crooked teeth
- Mouth appliances that fit poorly, such as braces or dentures
- Pregnancy
- Having another disease, such as heart disease, cancer, diabetes or rheumatoid arthritis
- Poor diet
- Obesity
- Hormonal changes, such as during puberty, menopause or menstrual cycle
- Nutritional deficiencies, such as vitamin C deficiency, vitamin D deficiency and vitamin B12 deficiency
- Broken fillings
Symptoms
Healthy gums are firm, taut and light pink. They fit tightly around your teeth and extend in between the very tops of your teeth.
Signs and symptoms of gingivitis include:
- Swollen or puffy gums
- Tender gums
- Dark red or reddish-purple gums
- Receding gums
- Bleeding gums, especially during brushing or flossing
- Bad breath that doesn’t go away
- Soft gums
- Gums that are away from your teeth
- Loose teeth
- Malocclusion, aka teeth that don’t line up as they used to
- Pus between teeth and gums
- Pain during chewing
- Sensitive teeth
Do not ignore the signs or symptoms of gum disease — they could be a warning sign for other serious problems.
Gum disease is associated with many health problems affecting the whole body, including heart disease and diabetes.
Conventional treatment
If you have signs or symptoms of gum disease, schedule an appointment with your dentist. Your dentist can diagnose you with gingivitis.
During your appointment, the dentist or hygienist will clean your teeth and show you the best way to brush and floss. The dentist may also recommend these conventional gingivitis treatments, such as:
- Regular dental cleanings (at least once every six months)
- Antibacterial mouthwash
- Retainers or orthodontics to align teeth properly
- Repair or replacement of dental appliances
- Treatment of other health conditions
- Over-the-counter anti-inflammatory medicine
In cases where gingivitis has progressed to more serious gum disease, you may need other medications, a deeper physical cleaning of your teeth and gums, or even dental surgery.
How do you reverse gingivitis?
Thankfully, conventional treatments can effectively reverse gum disease in many cases. You can kick-start the reversal of gingivitis with a professional dental cleaning and proper hygiene at home.
In many cases, these two steps are enough to reverse gingivitis and lead to healthier gums. In tough cases, your dentist can give extra tips for how to get rid of gingivitis.
For example, you may need to get your blood sugar under control if you also have diabetes.
How long will it take to reverse gingivitis?
Provided your teeth have been professionally cleaned of plaque and you are following proper hygiene techniques, you should see less bleeding and gum tenderness within just one to two weeks.
However, if you have more serious gum disease or other complicating factors, such as pregnancy or an illness, you may not see much improvement until your other issues are addressed.
In addition, you must continue good oral hygiene your whole life to keep gingivitis from returning.
Natural remedies
Many home remedies for gingivitis are easy to do and can be incorporated into whatever conventional treatment plan your dentist gives you. However, if you are taking medications, or if you have a health condition or illness, speak to your physician before stopping or starting any supplements, new diets or other treatments for your gingivitis.
Here are some natural gingivitis treatment options:
1. Use natural mouthwash
Homemade mouthwash options can be helpful in fighting the bacteria that cause plaque and gum disease. They may also relieve gum swelling and tenderness.
Try the following options for homemade natural mouthwash to try to treat your gingivitis symptoms:
- Make homemade mouthwash with essential oils.
- Shake the container to mix the oils with the water. Swish a small amount around in your mouth for 30 seconds. Spit it out.
- Other mouthwash essential oil options include lemongrass, aloe vera, sage and guava leaf oils.
- Make a saltwater rinse. A saltwater rinse can kill bacteria and help get food out of your mouth. It can also speed the healing of your gums.
- Mix ½ to ¾ teaspoon of salt into a glass of warm water.
- Swish the mouthwash around in your mouth for 30 seconds, then spit it out.
- Do this at least two or three times each day.
2. Brush and floss correctly
Follow the American Dental Association’s guide to proper mouth cleaning:
- Brush at least twice each day using a soft-bristled brush. Replace the brush every three to four months.
- Hold the brush at a 45-degree angle to your teeth and gums.
- Gently push the brush back and forth in short strokes.
- Clean all areas of your teeth. Tilt the brush vertically to brush the inside surfaces of your front teeth.
- Floss every day to remove food and bacteria that get stuck between your teeth.
- Use 1.5 feet of floss, and wrap the ends around your middle fingers.
- Slide it in between your teeth, and hold it in a “C” shape.
- Saw back and forth and side to side as you pull up.
3. Consider oil pulling
If you have difficulty flossing or find it too painful at first, you can consider oil pulling. Some believe it is more effective than flossing.
To do oil pulling, follow these steps:
- Mix about a tablespoon of coconut oil and, if you like, several drops of food-grade essential oil, such as clove or peppermint oil.
- Swish it in your mouth for 10 to 20 minutes.
- Spit it out.
- Rinse your mouth with water or saltwater.
- Brush as normal.
- Repeat the oil pulling three to five times per week.
Arimedadi oil can also be used. It was found to be as effective as a chemical mouthwash at killing plaque and improving gum health in a study of 45 people with gingivitis.
4. Ask about dietary supplements
A well-balanced diet may supply you with enough vitamins and minerals to have good oral health. However, some people may not obtain enough of certain vitamins or nutrients from their diets.
Vitamins to include in your diet either via eating or through supplements include:
- Vitamin A
- Vitamin B complex
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
Other available supplements that may be useful for improving oral health include:
- Lycopene
- Melatonin
- Calcium
- Magnesium
- Iron
- Zinc
5. Try topical applications
Although natural topical gingivitis treatments may be hard to find, they have been found to be effective at fighting plaque and bacteria in formal studies. You can make your own or consult your dentist or a natural medicine specialist for tips on making an oral gel or paste.
Please note that there is little research looking at the safety of most of these options. Do not swallow any of these gels or pastes.
In addition, always use high-quality, food-grade oils, herbs and spices in preparation of your natural remedies for gum disease.
- Clove rub. Clove has anti-inflammatory properties and effectively fights plaque. You can make a topical rub by mincing a teaspoon of cloves and applying them to your gums with a damp cotton ball. Rub the cloves gently against your gums, let the spice sit for about a minute and then rinse your mouth out with water.
- Turmeric gel. In a study of 40 adults, turmeric gel applied to the gums was found to be effective in preventing plaque and gingivitis. This is likely due to its anti-inflammatory qualities. Please note that the study participants also did manual plaque control, such as cleaning their teeth with toothbrushes, floss, picks or other manual techniques.
- Aloe vera gel. In a survey of traditional herbal healers in Cameroon, aloe vera gel was reported as a specific treatment for gingivitis. It is prepared from the plant leaves and rubbed on the gums.
- Neem gel. A study in adults who applied a gel with neem (Azadirachta indica) leaf extract found that after six weeks the gel was at least as effective at reducing plaque and bacteria as a standard chemical mouthwash.
- Black cumin gel. There is some research in people with gum disease supporting the use of oral chips (inserted into gum pockets by a dentist) with the active ingredient in black cumin working to treat gingivitis.
6. What to eat and what not to eat
In general, you definitely want to eat a healthy diet loaded with healing foods. These are some choices that can specifically help fight gum disease, such as:
- Wild-caught fish – Salmon, mackerel and sardines contain omega-3 fatty acids like DHA that help reduce inflammation. Research has shown that a higher intake of DHA is associated with a lower prevalence of periodontitis.
- Fresh vegetable juices – Loaded with helpful essential nutrients and enzymes.
- Chewing gum with xylitol – Some studies point toward the ability of xylitol to help prevent the buildup of bacteria and dental plaque in the mouth. (19)
- Raw vegetables and apples – Raw veggies like celery and carrots, as well as apples, can help naturally clean teeth. Of course, they’re not a replacement for real teeth-cleaning methods, but when you consume them, they are known to be cleansing.
These are some of top foods to avoid if you want to combat gum disease:
- Sugar – Avoiding sugar in your diet is so important for gum health because it feeds bacteria.
- Fruit juice – High-sugar fruit juice can coat the teeth with sugar and feed bacteria in the mouth.
- Ultra-processed foods – These foods can contain a lot of additives and sugar that can promote the growth of bacteria.
- Grains – Grains that are unsprouted and unfermented contain phytic acid, which many experts believe has a negative effect on dental health.
- Hydrogenated oils – Vegetable oil, canola oil, corn oil and soybean oil are all hydrogenated oils that contain trans fat, which is a well-known trigger of systemic inflammation.

How to prevent gingivitis
1. Eat a diet to support oral health
Your diet influences your oral health. Bacteria thrive on sugar in carbohydrates, for example.
By following a diet that supports healthy teeth and gums, you may be able to avoid or even reverse tooth decay as well as gum disease:
- Remove sugar from your diet. Instead, use stevia and raw honey in moderation.
- Avoid phytic acid. It is found in grains, beans, nuts and soy. Instead of avoiding these foods altogether, you can soak and sprout them or do sourdough fermentation to reduce the amount of phytic acid.
- Focus on nutrient-rich foods — particularly foods with fat-soluble vitamins and important minerals. These include foods such as bone broth, meat, fish, eggs, raw and cooked vegetables (especially leafy greens), along with healthy fats, such as coconut oil or avocado. Limit or totally avoid ultra-processed foods and foods with added sugar.
2. Be aggressive about oral hygiene
If you want to prevent gingivitis or keep it from coming back after it has been treated, commit to excellent oral hygiene. You will need to maintain good hygiene for life since gingivitis can become chronic or can come back after treatment.
- Brush after every meal or at least twice per day.
- Consider using a homemade probiotic toothpaste or a baking soda toothpaste or gum rub.
- Floss at least once daily, or do oil pulling three to five times per week.
- Use a mouthwash without alcohol.
- Go to the dentist for a cleaning at least twice each year. Ask your dentist for additional ideas about cleaning your teeth effectively.
- Replace your toothbrush every three to four months or as soon as it shows wear.
- Consider an electric toothbrush to help you remove plaque and tartar more effectively.
- Use a dental pick or special tool to get trapped food and bacteria out from between your teeth.
- Ask your dentist if you may benefit from getting orthodontic work done on your teeth or if any dental appliances you have need to be repaired.
3. Manage your other health conditions
There is a close tie between oral health and your overall health.
For example, people with poorly controlled diabetes are at higher risk of gingivitis. This is because having high blood sugar makes it easier for bacteria to thrive in the mouth, which can lead to gum disease.
Similarly, getting infections, stress and other health problems under control can keep your risk for gingivitis in check.
In addition to getting proper treatment for any diseases you may have, talk with your doctor about your medications. Some drugs make your gums more susceptible to disease.
Do not stop taking a medication without first consulting your physician. However, if you are having repeat problems with gingivitis, it may be worth discussing your prescription options with your doctor.
4. Don’t use tobacco
If you smoke, quit. If you chew tobacco, quit.
Smoking is a key risk factor for developing gum disease. Other than brushing and cleaning your mouth properly, it is likely the most direct way to impact your risk of gingivitis.
Using tobacco can also make it harder to treat your gingivitis successfully.
Precautions
Many herbs and essential oils have antibacterial effects that could be useful in fighting gum disease and plaque. However, few have been studied for human safety in oral hygiene routines.
Do not swallow mouthwash, gum, toothpastes, oil used for oil pulling or other non-food remedies.
Do not start or stop a medication or a dietary supplement without first speaking with your doctor.
If you have symptoms of gingivitis that do not improve after a few weeks of using natural remedies, talk to your doctor or dentist.
Final thoughts
- Gingivitis is a common condition affecting the gums. It is usually caused by the buildup of bacteria and food particles along the gumline. This buildup irritates the gums and can lead to infection, swelling and other problems.
- In many cases, gingivitis can be managed and prevented using natural methods, such as good oral hygiene and a healthy diet.
- Gum disease can lead to or be affected by other health conditions. Get regular dental cleanings, and talk to your doctor if you suspect more is at play than just gingivitis.
- Ways to help keep your gums healthy include using homemade mouthwash, brushing and flossing daily and correctly, oil pulling, certain supplements, topical applications, and eating a healthy diet loaded with anti-inflammatory foods.
- You can help prevent getting gingivitis in the first place by eating a diet that supports the oral microbiome, being aggressive about oral hygiene, managing other health conditions that could affect the mouth and avoiding tobacco products.



