This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
5 Natural Degenerative Joint Disease Treatments That Work
January 8, 2016

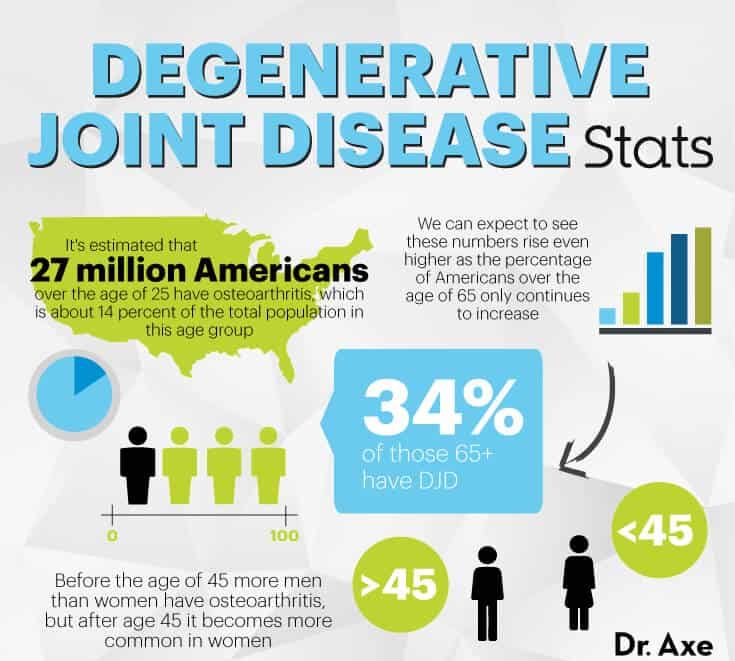
Unless you’re a hermit or ardent loner, you probably know somebody — or several somebodies — dealing with degenerative joint disease (DJD). Also known as osteoarthritis, an estimated 27 million Americans over the age of 25 have DJD, which is about 14 percent of the total population in this age group. (1)
Even worse, about 34 percent of those 65-plus have DJD. And because it develops in older people more frequently, we can expect to see these numbers rise even higher as the percentage of Americans over the age of 65 only continues to increase.
So what is degenerative joint disease, and can this common form of arthritis be naturally treated? Let’s take a look at how diet and lifestyle can help manage DJD.
What Is Degenerative Joint Disease (DJD)?
Degenerative joint disease is a progressive disorder that attacks the body’s cartilage, which is the hard tissue that covers up the end of bones and meets the joints, allowing bones to move.
DJD is believed to be the most common form of arthritis there is by far and the primary cause of joint pain in adults, usually affecting older people and slowly getting worse as they continue to age.
The terms degenerative joint disease, degenerative arthritis, and osteoarthritis (sometimes called osteroarthrosis) are often used interchangeably. Both are essentially the same type of disorder that results in cartilage (tissue between your bones) wearing down over time and causing a lot of bone and joint pain in the process. Osteoarthritis is degenerative in nature because it worsens as time goes on, and unfortunately there isn’t a known “cure” at this time to stop it from progressing or to reverse the damage already done. (2)
You can develop osteoarthritis symptoms all over your body, in any joints, but it usually affects the spine (upper and lower back), neck, hips, knees and hands (especially the ends of the fingers and thumbs) most significantly. Symptoms of osteoarthritis/degenerative joint disease usually include: (3)
- joint pain, which can worsen at times and “come and go” in terms of how painful it feels
- stiffness (especially in the morning after getting out of bed)
- trouble moving, which worsens as the disease progresses
- more pain, inflammation and limitations as time goes on (in some people it progresses quickly, but for most it takes years for symptoms to become very bad — early on joints might only ache after exercise, but then they can become more noticeable any time of day)
- trouble doing everyday tasks like bending over, getting dressed, walking, reaching, squatting (especially if you have osteoarthritis in the knees) or performing certain physical tasks as part of work (although for some people osteoarthritis is relatively mild, and they can go about their days pretty normally) (4)
- if DJD affects your hips, you might feel pain in the groin, inner thigh, buttocks or the knees
- if DJD affects your joints, you might develop small bone spurs on your knuckles and your fingers can become enlarged, achy, stiff and numb
- DJD in the spine can cause numbness in the neck and a stiff lower back
- you might hear the sound of bones rubbing against each other when the disease becomes severe
- as a side effect of the ongoing pain and mobility/job limitations, depression, trouble sleeping, feeling hopeless and weight changes can sometimes also develop
Natural Degenerative Joint Disease/Osteoarthritis Treatment
While it might not be possible to totally cure degenerative joint disease once it’s developed, there are a lot of natural osteoarthritis treatment options available that can make a big impact. These include: exercising and staying active, preventing weight gain and maintaining a healthy body weight, eating an anti-inflammatory diet, and treating pain using physical therapy, sauna treatments, massage therapy and essential oils. All of these help lower severity of symptoms and slow progression of the disease so more cartilage is spared.
The primary goals of all degenerative tissue disease/osteoarthritis or arthritis treatments are to lower inflammation/swelling, control pain, improve mobility and joint function, help maintain a healthy weight so you put less pressure on fragile joints, and to improve your mood — so you’re better able to handle the stress of battling a degenerative disease.
1. Stay Active
While most people with osteoarthritis usually have joint pain and some movement limitations, many find that they feel better and experience less symptoms overall when they keep moving. In fact, exercise is considered one of the most important treatments for degenerative joint disease. Like the old saying goes, “Move it or lose it.” In other words, the more you strengthen and stretch your body parts, the better intact they’ll stay into older age.
Exercise is important for lowering inflammation, increasing flexibility, strengthening muscles (including the heart), boosting circulation and supporting a healthy body weight. It helps keep joints and bones strong and limber, improve heart health/cardiovascular fitness, extend the range of motion of joints, and move synovial fluid throughout the body better. Plus, let’s not forget about the mental benefits of exercise. Getting regular exercise is a powerful way to lower stress, improve your mood, control stress hormones like cortisol and help you sleep better.
Because every DJD patient is different in terms of physical abilities and pain level, the amount and form of exercise prescribed depends on each person’s specific condition and how stable the joints are. You want to ideally do a combination of three types of exercises for osteoarthritis: (5)
- strengthening exercises targeted at improving strength in muscles that support effected joints — such as knee strengthening exercises
- aerobic activities to improve blood pressure, circulation and inflammation
- range-of-motion activities to keep joints flexible and help you become more comfortable with daily movements
Some of the most beneficial, and least painful, types of exercise include walking, swimming and water aerobics. If exercise is painful at first or you’re just beginning to become more active, your doctor and/or physical therapist can recommend specific types of exercise that would be safest and most helpful. Start slowly and find ways to sneak more fitness into your day while you build up resilience and strength.
2. Lower Inflammation and Support Cartilage with a Nutrient-Dense Diet
Research suggests that a poor diet increases inflammation and might increase enzymes that destroy collagen and other proteins important for maintaining healthy tissue. Cartilage is about 65 percent to 80 percent water, and the remainder is made up of three components: collagen, proteoglycans and chondrocytes.
Collagen is a type of fibrous protein that acts as the body’s natural “building blocks” for skin, tendons, bone and other connective tissues. Proteoglycans interweave with collagen to form mesh-like tissue that allows cartilage to absorb shocks and vibrations, while chondrocytes mostly produce cartilage and help it stay intact as we get older.
Some of the ways you can help the body hold on to precious cartilage and lower inflammation is to load up on all sorts of natural anti-inflammatory foods. These provide essential fatty acids, antioxidants, minerals and vitamins that support the immune system, lower pain, and help with healthy tissue and bone formation.
Focus your diet around these foods as much as possible:
- fresh vegetables (all kinds): Aim for variety and a minimum of four to five servings per day
- whole pieces of fruit (not juice): three to four servings per day is a good amount for most people
- herbs, spices and teas: turmeric, ginger, basil, oregano, thyme, etc., plus green tea and organic coffee in moderation
- probiotic foods: yogurt, kombucha, kvass, kefir or cultured veggies
- wild-caught fish, cage-free eggs and grass-fed/pasture-raised meat: higher in omega-3 fatty acids and vitamin D than farm-raised varieties and great sources of protein, healthy fats, and essential nutrients like zinc, selenium and B vitamins. Vitamin D has been shown to help support arthritis patients, so consider adding in more raw dairy if possible too. (6)
- healthy fats: grass-fed butter, coconut oil, extra virgin olive oil, nuts/seeds
- ancient grains and legumes/beans: best when sprouted and 100 percent unrefined/whole
- Bone broth: contains collagen and helps maintain healthy joints
Limit or eliminate these foods that promote inflammation:
- Refined vegetable oils (like canola, corn and soybean oils, which are high in pro-inflammatory omega-6 fatty acids)
- Pasteurized dairy products (common allergens) and conventional meat, poultry and eggs, which contain added hormones, antibiotics and omega-6s that contribute to inflammation
- Refined carbohydrates and processed grain products and added sugars (found in the majority of packaged snacks, breads, condiments, canned items, cereals, etc.)
- Trans fats/hydrogenated fats (used in packaged/processed products and often to fry foods)
3. Maintain a Healthy Body Weight
Carrying excess body weight puts strain on joints that are already delicate. (7) Osteoarthritis patients who are overweight should try to reach a healthy body weight in a realistic way, using a well-balanced diet and adding in more movement. This should be viewed as a long-term lifestyle change, not a quick-fix diet that’s very low in calories and will likely result in nutrient deficiencies that are needed to limit further injuries.
4. Get Enough Rest/Relaxation
When you don’t get enough sleep, downtime and relaxation in your life, your joints and muscles have a harder time repairing themselves, while your stress hormones, body weight and inflammation all tend to rise. You need to get enough sleep every night (seven to nine hours usually) in order to relieve joints from stress, keep stress hormone levels balanced, regulate your appetite and repair damaged tissue. Learn to recognize your body’s signals, and know when to stop or slow down and take a break, so you avoid becoming anxious, overexerted and run-down.
5. Control Pain Naturally
Dealing with pain can be one of the hardest things about battling degenerative joint disease, since it takes away from your quality of life, ability to do your job well and independence. Many doctors prescribe anti-inflammatory medications (like NSAIDs) or even surgery to dull pain if the situation becomes bad enough, but you can also use non-drug pain-relief techniques that are just as effective. Some popular complementary and alternative therapies that help fight pain include:
- Acupuncture: Studies show that patients receiving acupuncture normally have less pain than patients in placebo control groups. Acupuncture is proven to help lower symptoms of back and neck pain, muscle aches and joint stiffness, osteoarthritis, and chronic headaches. (8)
- Massage therapy: A professional massage can help improve circulation, bring blood to sensitive areas, relax the mind and lower stress.
- Reflexology: Reflexology has been used for hundreds of years to stimulate the nervous system and help the body handle stress, fatigue, pain and emotional problems.
- Infrared sauna treatments: Both heat and cold (or both together, used at different times) can be useful for loosening up joints and muscles and lowering swelling or pain. (9) At home you can use warm towels, ice packs, hot packs or a hot shower to reduce pain. Also consider trying infrared saunas, which are a type of sauna that uses heat and light to help relax the body by creating heat and causing you to sweat and release stored toxins. They’ve been shown to lower pain and are believed to have a parasympathetic healing effect, which means they help the body handle stress better.
What Causes Osteoarthritis/DJD?
People with DJD don’t maintain enough healthy cartilage as they age, which means movement becomes more painful as bones rub closer to one another, instead of being blocked by the slippery substance that’s supposed to act as a buffer between the bones. We need cartilage to help bones “glide” and also to absorb vibrations or shocks we experience when we move around, which is why most people with degenerative joint disease find it hard to go about normal day-to-day activities.
When the disease progresses enough, bones rub together in a way that causes inflammation, swelling, pain, loss of mobility and sometimes changes to the shapes of joints.
Here’s a quick overview of how joints work. Joints are the point where two or more bones are connected, and they’re made up (in most cases) of the following parts: cartilage, joint capsule (tough membrane sacs that enclose all the bones), synovium (located inside the joint capsules and responsible for secreting lubricating synovial fluid) and synovial fluid (buffers and lubricates the joints and cartilage). (10)
In people who don’t suffer from DJD or other forms of joint damage (like rheumatoid arthritis), their joints are encased in smooth cartilage and lined with synovial fluid that helps with the “sliding” of cartilage against bones, bones against muscles and muscles against connective tissues.
In severe cases of degenerative joint disease, joints start to become smaller and also to change shape while small deposits of bone (osteophytes, which are sometimes also called bone spurs) can also form around the edges of the joints where they shouldn’t be. The main problem with bone spurs is that at any time they can break off from the cartilage they grow on and make their way into the space where the joints are, further causing pain and complications.
Risk Factors For Degenerative Joint Disease
What are the underlying causes of osteoarthritis? It isn’t fully agreed upon or known at this time, but the disease seems to be caused by a combination of different factors that raise someone’s risk, including: (11)
- older age (it’s most common among people over the age of 65, but anyone can develop DJD) (12)
- being a woman (interestingly, before the age of 45 more men than women have osteoarthritis, but after age 45 it becomes more common in women)
- being overweight or obese
- experiencing any injuries to the joints that lead to malformation
- having a job or regular hobby that puts a lot of stress on the joints or involves repetitive motions
- having certain genetic defects that affect the development of joint cartilage and collagen
- having DJD/osteoarthritis run in your family (you’re more likely to develop this disease if your parents or grandparents also did) (13)
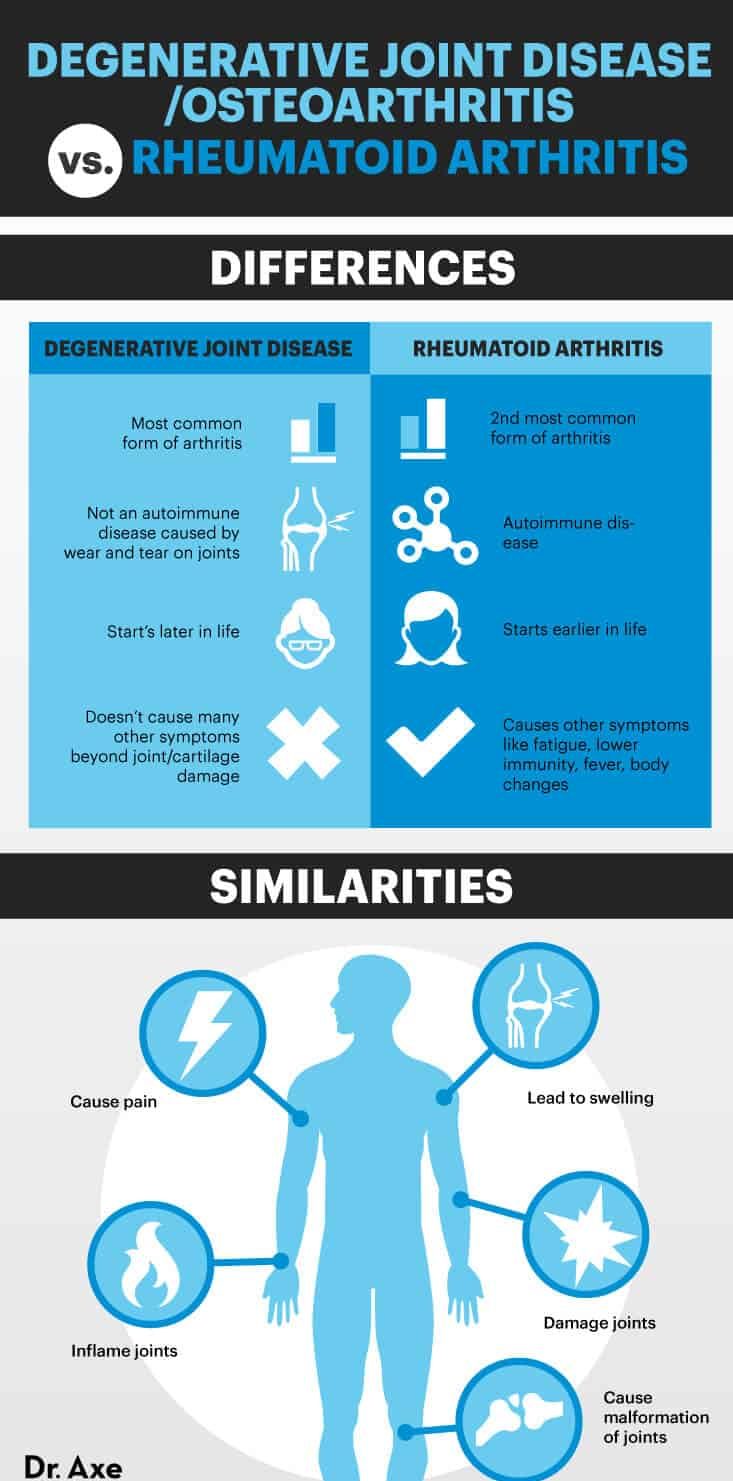
Wondering what makes osteoarthritis different than rheumatoid arthritis (RA)? RA is the second most common form of arthritis after osteoarthritis/degenerative joint disease. RA is considered to be an autoimmune disease because it results from the immune system attacking the body’s own healthy tissues that makes up the joints. Osteoarthritis is caused by mechanical wear and tear on joints and is not classified as an autoimmune disease. (14)
Both DJD and RA lead to pain, swelling, joint inflammation, and eventually joint damage or malformation. Compared to RA, DJD usually starts later in life. Rheumatoid arthritis can begin early in life or during middle age and also usually causes other symptoms beyond just loss of joint/cartilage tissue, including: fatigue, lower immunity, and sometimes fever, changes to skin tissue, the lungs, the eyes or the blood vessels.
Key Takeaways For Degenerative Joint Disease:
- Degenerative joint disease, also called osteoarthritis, is the leading type of arthritis in adults.
- DJD results in decreased cartilage and joint tissue, which leads to joint pain, inflammation and trouble moving.
- It’s caused by a combination of factors: genetics, high inflammation, poor diet, inactivity, repetitive motions and getting older (normal “wear and tear” on the body).
- You can help prevent and treat degenerative joint disease naturally by eating a nutrient-dense diet, staying active, reducing stress, and relieving pain with alternative treatments like acupuncture, massage therapy and heat/cold applications.



