This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Gut-Brain Connection: How It Works + How to Support It
April 4, 2025
You’ve probably used the phrases: “I have butterflies in my stomach,” “I have a gut feeling about this,” and “there’s a pit in my stomach.” Have you ever wondered why so many of these sayings involve our brains and tummies? The answer is the gut-brain connection.
As it turns out, your nervous stomach isn’t such a coincidence. In fact, the more we learn about the human gut, or the gut microbiome, the more it’s clear that it really is our “second brain.”
You’re probably already aware that leaky gut syndrome is linked to serious conditions and diseases. Turns out, science is discovering that the connection between our guts and our emotions is just as strong.
What is the gut-brain connection?
The gut and brain are in constant communication, influencing everything from mood and cognition to digestion and immunity. This complex relationship, known as the gut-brain connection, is a growing area of scientific research.
It sheds light on how gut health affects mental well-being and how stress, anxiety and neurological conditions can impact digestive function.
The gut-brain connection refers to the bi-directional communication between the gastrointestinal (GI) system and the central nervous system. This communication happens through multiple pathways, including the vagus nerve, the enteric nervous system (ENS), and biochemical signaling via neurotransmitters and hormones.
Role of the vagus nerve
The vagus nerve is one of the primary pathways connecting the gut and brain. It sends signals in both directions, allowing the brain to influence gut function and vice versa.
Studies have shown that stimulating the vagus nerve can improve mood and reduce symptoms of depression and anxiety.
Role of the enteric nervous system, your “second brain”
The ENS is often referred to as the “second brain” because it contains more than 100 million neurons that regulate digestion independently of the brain. The ENS plays a crucial role in gut motility, enzyme secretion and inflammatory responses, which can impact overall health.
The microbes in the gut play a significant role in human body function. The gut microbiome is responsible for everyday functions, including digestion and the nutrient absorption.
The gut and brain work in a bi-directional manner, which means that gut health can impact stress, anxiety, depression and cognition.
Scientific studies have shown that the gut is home to the ENS. Separate from the central nervous system, the ENS is made up of two thin layers with more than 100 million nerve cells in them, more than the spinal cord.
These cells line the gastrointestinal tract, controlling blood flow and secretions to help the gastrointestinal tract digest food. They also help us “feel” what’s happening inside the gut, since this second brain is behind the mechanics of food digestion.
While the second brain doesn’t get involved in thought processes like political debates or theological reflection, studies have suggested that it does control behavior on its own. Researchers believe this came about to make digestion more efficient in the body.
Instead of having to “direct” digestion through the spinal cord and into the brain and back, we developed an on-site brain that could handle things closer to the source.
Because this second brain is so complex, scientists aren’t convinced that it was designed as just a way to aid in digestion. So while it isn’t capable of thoughts, it does “talk” to the brain in major ways.
How the gut microbiome affects the brain
Your gut is home to trillions of microbes, including bacteria, fungi and viruses. Collectively known as the gut microbiome, these microorganisms play a vital role in digestion, immune function and neurotransmitter production.
Microbiome and neurotransmitter production
Gut bacteria help produce key neurotransmitters, like serotonin, dopamine and gamma-aminobutyric acid (GABA), which influence mood, cognition and stress response. In fact, about 90 percent of serotonin, the “feel-good” neurotransmitter, is produced in the gut.
Inflammation and mental health
An imbalanced gut microbiome can lead to chronic inflammation, which has been linked to mental health disorders, such as depression, anxiety and cognitive decline. Certain gut bacteria can release inflammatory molecules that disrupt brain function and increase the risk of neurodegenerative diseases, like Alzheimer’s and Parkinson’s.
Impact of stress on gut health
Just as gut health affects the brain, stress and emotional health impact digestion. Chronic stress can:
- Alter gut motility, leading to constipation or diarrhea
- Increase gut permeability (“leaky gut”), allowing harmful substances to enter the bloodstream
- Disrupt the balance of gut bacteria, reducing beneficial strains and promoting harmful ones
Practicing stress management techniques, such as mindfulness, deep breathing and exercise, can help restore balance in the gut and support mental well-being.
Impact on depression
The gut microbiome appears to play a role in depression. The microflora has proved to benefit mental health by enhancing the microbiome content in our GI systems.
Researchers have learned that healthy gut microflora transmits brain signals through pathways that are involved in brain neuron formation and behavioral control. They also proved that inflammation affects the brain and how someone thinks, which explains why more than 20 percent of inflammatory bowel disease patients exhibit depressed behaviors.
One study illustrated how the gut and brain are connected through studying the effects of probiotics on patients with irritable bowel syndrome and depression. Researchers found that twice as many patients saw improvements from depression when they took a probiotic as compared to the other patients who took a placebo.
Again, with an improvement of the gut came an improvement of mental well-being. Patients in this study took the probiotic Bifidobacterium longum NCC3001 daily.
Studies have shown that patients with inflammatory diseases are prone to depression. The theory is that a dysregulation of the pathways involved in the gut-brain axis is responsible for this phenomenon.
Research has indicated that inflammation leads to depression, and depression worsens cytokine responses, so it’s really just a vicious cycle.
Impact on anxiety
Research has revealed that stress is intimately tied to our guts, thereby proving the gut-brain connection.
We know that gut health influences anxiety and the body’s response to stress as part of the brain-gut connection.
Our bodies respond to stress with a “fight or flight system,” related to our cortisol levels and which we know is ruled by the hypothalamic-pituitary-adrenal axis.
When something scary or worrying happens, like someone unexpectedly jumping in front of you, you have a physical reaction: Your palms might get sweaty, and you might feel your heartbeat quicken.
Typically, if you’re in a stressful situation that is then diffused, your body goes back to normal. However, if you’re constantly stressed, your body is stuck in that fight-or-flight phase over an extended period of time.
The critical part is that our bodies are unable to distinguish between physical and mental stress. Thus your body responds the same way if a bear shows up in your home as it does when you realize you hate your job; it tries to combat the stress.
This constant state of stress causes chronic inflammation. The body reacts to the stress as a type of infection and tries to overcome it.
Because inflammation is at the root of many diseases, this exposure to prolonged stress can have serious consequences for your health, ranging from high blood pressure to autoimmune disorders.
The types of bacteria found in the gut, “good bacteria,” play a role in how our immune responses are regulated.
How diet influences the gut-brain connection
A nutrient-rich diet supports a healthy gut microbiome and brain function. Key dietary components include:
- Prebiotic foods: Fiber-rich foods, like bananas, onions, garlic and asparagus, feed beneficial gut bacteria.
- Probiotic foods: Fermented foods, like yogurt, kefir, sauerkraut and kimchi, introduce beneficial bacteria to the gut.
- Healthy fats: Omega-3 fatty acids, found in salmon, flaxseeds and walnuts, reduce inflammation and support brain function.
- Polyphenols: Antioxidant-rich foods, like berries, green tea and dark chocolate, support gut health and cognitive function.
- Amino acids: Protein sources, such as lean meats, eggs and legumes, provide essential building blocks for neurotransmitters.
Role of exercise and sleep
Regular physical activity promotes gut motility and microbial diversity, while quality sleep helps regulate the gut microbiome and reduce inflammation. Poor sleep has been linked to an imbalance in gut bacteria, which may contribute to mood disorders and cognitive impairment.
Natural ways to improve your gut-brain connection
While there’s still much to uncover about the mystery of the gut and all it affects, we are sure of a few things you should do to improve your gut-brain connection.
1. Avoid ultra-processed foods
For starters, a whole foods-based diet leads to a gut with a much different makeup than one that’s been fed mainly refined and processed foods. Even worse, ultra-processed foods (like white bread, chips and snack cakes) make up nearly 60 percent of the average American’s diet.
The added sugar found in these foods, often disguised as different types of artificial sweeteners, are responsible for a variety of health conditions, from obesity to type 2 diabetes to migraines.
2. Consume probiotics and fermented foods
Eating probiotic-rich foods, like kefir and sauerkraut, can also cause your gut and mood to thrive. Probiotics are good bacteria that primarily line your gut and are responsible for nutrient absorption and supporting your immune system.
3. Limit gluten intake and avoid allergens
For many people, limiting gluten also can have a positive effect on their gut microbiomes. The traditional methods of soaking, sprouting and souring grains in order to make them digestible and nutritious have been abandoned for a fast and convenient method of mass producing food, and our guts have taken the brunt of it.
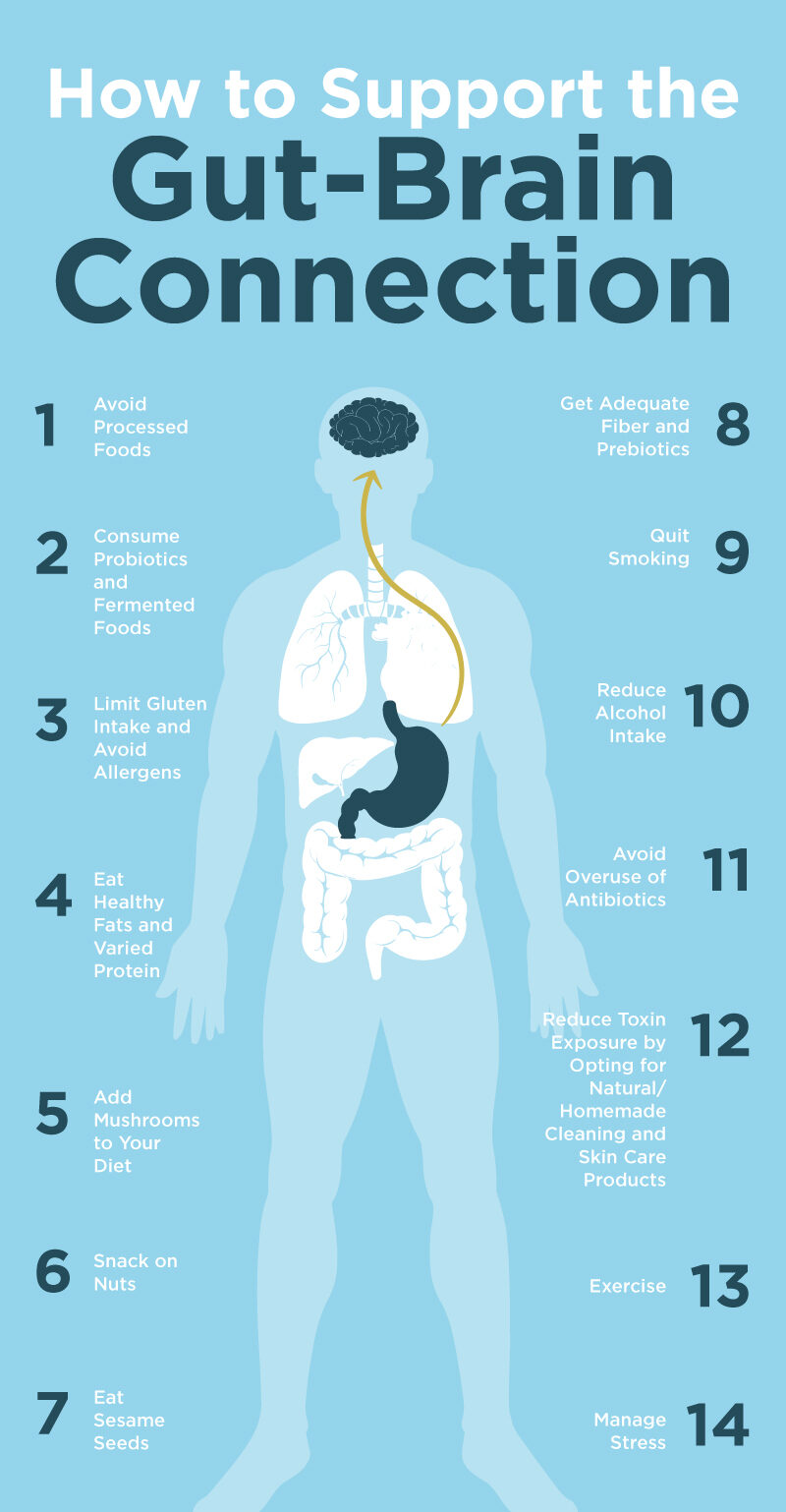
4. Eat healthy fats and varied protein
Healthy fats are essential for brain development.
Olive oil, for instance, includes a high amount of antioxidants that protect your cells from damage. It also helps improve memory and cognitive function, and it works as an anti-inflammatory.
Avocado benefits range from protecting your heart to helping with digestion, and it’s also a great pick for improving your mood.
In addition, high-protein foods, both from animals and plants, have been found to support and enhance the gut-brain connection.
5. Add mushrooms to your diet
The shiitake mushroom contains plenty of vitamin B6. Because vitamin B6 impacts the production of serotonin and neurotransmitters, healthy B6 levels are associated with a positive mood and reducing stress naturally.
6. Snack on nuts
Have a small handful of nuts, like almonds, cashews, walnuts and Brazil nuts.
Why? Research shows they’re full of serotonin, a feel-good chemical that’s in short supply when you’re depressed.
7. Eat sesame seeds
Sesame seed benefits stem from tyrosine, an amino acid that boosts the brain’s dopamine levels. It kicks the feel-good hormone into high gear while balancing out the others.
8. Get adequate fiber and prebiotics
Increasing fiber and prebiotic intake can significantly enhance the gut-brain connection.
Fiber and prebiotics promote the growth of beneficial gut bacteria, which produce short-chain fatty acids (SCFAs) like butyrate. SCFAs help maintain the integrity of the gut barrier and reduce inflammation, which is crucial for proper gut-brain communication.
A diet rich in fiber and prebiotics has been associated with improved cognitive function and reduced risk of neurological disorders.
9. Quit smoking
Smoking cessation can have a positive impact on the gut-brain axis because smoking alters the gut microbiome composition, reducing beneficial bacteria and increasing potentially harmful ones.
Quitting smoking allows the gut microbiome to recover, potentially improving gut barrier function and reducing inflammation. Improved gut health after smoking cessation may contribute to better mental health outcomes and reduced risk of neurological disorders.
10. Reduce alcohol intake
Reducing alcohol consumption can significantly benefit the gut-brain connection since chronic alcohol use disrupts the gut microbiome balance and increases intestinal permeability, leading to inflammation and potential neuroinflammation. Alcohol reduction or abstinence can help restore gut microbiome diversity and improve gut barrier function.
Improved gut health following reduced alcohol intake may lead to better cognitive function and reduced risk of alcohol-related neurological disorders.
11. Don’t overuse antibiotics
Overuse of antibiotics can disrupt the gut microbiota, potentially impairing the gut-brain axis and affecting neurological health. A review in the International Journal of Molecular Sciences indicated that antibiotic-induced gut dysbiosis may lead to cognitive impairments by altering neurotransmitter levels and neuroinflammatory responses.
Another study discussed how antibiotic exposure, particularly during critical developmental periods, can increase the risk of neurodevelopmental disorders by disrupting the gut-brain axis.
12. Reduce toxin exposure
Reducing exposure to environmental toxins can positively influence the gut-brain axis, thereby enhancing neurological health. A study published in 2024 examined the effects of per- and polyfluoroalkyl substances (PFAS) on young adults.
Researchers found that higher PFAS exposure was associated with alterations in gut microbiota and metabolic profiles, leading to increased inflammatory metabolites and decreased anti-inflammatory ones. These changes were linked to reduced kidney function over a four-year period, suggesting that minimizing PFAS exposure could help maintain gut health and prevent related systemic issues.
Furthermore, a review in the International Journal of Environmental Research and Public Health discussed how environmental pollutants like bisphenol A (BPA), chlorpyrifos, diethylhexyl phthalate (DEHP) and PFAS can disrupt the gut microbiome. Such disruptions may impair the bi-directional communication between the gut and brain, potentially leading to neurodevelopmental and neurological disorders.
The authors emphasized the importance of reducing exposure to these contaminants to maintain gut-brain axis integrity and support neurological health.
13. Exercise
Engaging in regular physical activity has been shown to positively influence the gut-brain axis, enhancing both gut microbiota composition and neurological health. A narrative review in Nutrients shared that exercise can increase the diversity and abundance of beneficial gut bacteria, which may contribute to improved mental health outcomes.
Another study published in 2025 indicated that exercise-induced alterations in gut microbiota are associated with reductions in depression and anxiety symptoms, suggesting a pivotal role of the gut-brain connection in mediating these effects.
14. Manage stress
Managing stress effectively can enhance the gut-brain connection, leading to improved gastrointestinal and mental health. Chronic stress is known to disrupt the gut microbiota, contributing to various gastrointestinal disorders and impacting mental well-being.
A systematic review from 2021 suggested that perceived stress and early life stress may impact the gut microbiota in humans. The review also indicated that dietary interventions, such as omega-3 fatty acids and pre- and probiotics, may buffer against the effects of stress on the gut microbiome, although more research is needed.
Another observational study examined the effects of a psychosocial intervention on the gut microbiome and depression symptoms in adults. The findings suggested that stress reduction interventions can lead to beneficial changes in the gut microbiome, which are associated with improvements in depression symptoms.
These studies underscore the importance of stress management techniques, such as mindfulness, therapy and dietary interventions, in promoting a healthy gut microbiome and strengthening the gut-brain axis, thereby enhancing overall well-being.
15. Take colostrum
Components found in colostrum may influence the gut-brain connection. For instance, human milk oligosaccharides (HMOs), abundant in human colostrum, play a crucial role in shaping the neonatal gut microbiome and supporting neurodevelopment.
A narrative review published in 2024 revealed that HMOs influence gut microbiota composition and enhance neurotransmitter production, essential for brain development. For instance, 2′-fucosyllactose fosters beneficial gut bacteria that produce short-chain fatty acids, supporting cognitive development.
Preclinical human and animal studies also have suggested that milk oligosaccharides can support normal microbial communities and behavioral responses during stress.
16. Prioritize sleep
Adequate sleep plays a crucial role in maintaining a healthy gut-brain connection, primarily by influencing the composition and diversity of gut microbiota. Research has relayed that better sleep quality is associated with a more diverse and balanced gut microbiome, which is essential for effective communication between the gut and the brain.
A study published in PLOS ONE found that individuals with higher gut microbiome diversity experienced increased sleep efficiency and total sleep time, along with reduced wake episodes after sleep onset. This suggests that a diverse gut microbiota may contribute to improved sleep physiology.
Another review in Sleep Medicine Reviews discussed the bi-directional relationship between sleep and gut microbiota. It highlighted that sleep deprivation can lead to gut microbiota imbalances, which may negatively affect brain function and behavior. Conversely, maintaining healthy sleep patterns supports a balanced gut microbiome, thereby enhancing the gut-brain axis.
Yet another study examined the interaction between sleep, gut microbiota and brain function in infants. The findings revealed that sleep habits and gut bacterial markers are predictive of behavioral and developmental outcomes, emphasizing the dynamic interplay between sleep quality and the gut-brain connection during early development.
We don’t have all the answers on the gut-mood link just yet, but one thing is certain: Our bodies and minds are much more connected than you believe. Taking care of one part will reap benefits for the rest of you.
By implementing these lifestyle changes, you can potentially improve your gut-brain connection, leading to better overall health and cognitive function. However, it’s important to note that the gut-brain axis is complex, and more research is needed to fully understand the mechanisms and long-term effects of these interventions.
Final thoughts
- The microbes in the gut play a significant role in human body function. They are responsible for everyday functions, including digestion and nutrient absorption, and gut health has a significant impact on mental health. This is known as the gut-brain connection.
- Research has shown that there’s a connection between gut microbiota and mental health disorders like depression and chronic anxiety or stress.
- The key is to improve gut health, which will reduce systemic inflammation and improve mental health thanks to the gut-brain connection.


