This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
C. Diff Infection: Causes, Symptoms & 8 Natural Treatments
June 26, 2019

According to the Centers for Disease Control and Prevention in the United States, a Clostridium difficile infection (also commonly known as C. diff) is currently one of the leading drug-resistant threats to our population. A 2015 CDC study reveals that C. difficile was behind nearly 500,000 infections among patients in the United States in just one year. Can C. diff lead to death? Unfortunately, yes. Of those half a million, around 15,000 people died as a direct result of their C. difficile infections. Of those deaths, over 80 percent were among Americans 65 years old or over.
What’s the biggest risk factor when it comes to C. diff? One word: antibiotics. The CDC clearly states, “Patients who take antibiotics are most at risk for developing C. difficile infections.” According to the CDC, people on antibiotics are 7 to 10 times more likely to get C. diff while on the drugs and during the month after.
It used to be considered a major health problem mainly experienced by older members of the population put on antibiotics while in a hospital or nursing home. However, recent research has shown that there is a rising incidence of C. diff infection among younger and healthier individuals. Is C. diff serious? In recent years, C. diff is proving itself to be a more common and more difficult to treat, serious colon infection.
A recent study published in the Annals of Internal Medicine also found that reoccurring cases of C. diff are becoming even more of a problem than first time cases of C. diff and in addition to antibiotic usage, C. diff is being linked the use of proton-pump inhibitors (commonly taken for acid reflux) and corticosteroids.
So exactly what is C. diff, what are the most common C. diff symptoms, is C. diff contagious and what is the best natural C. diff treatment? We’re about to discuss all this and more!
What Is C. Diff?
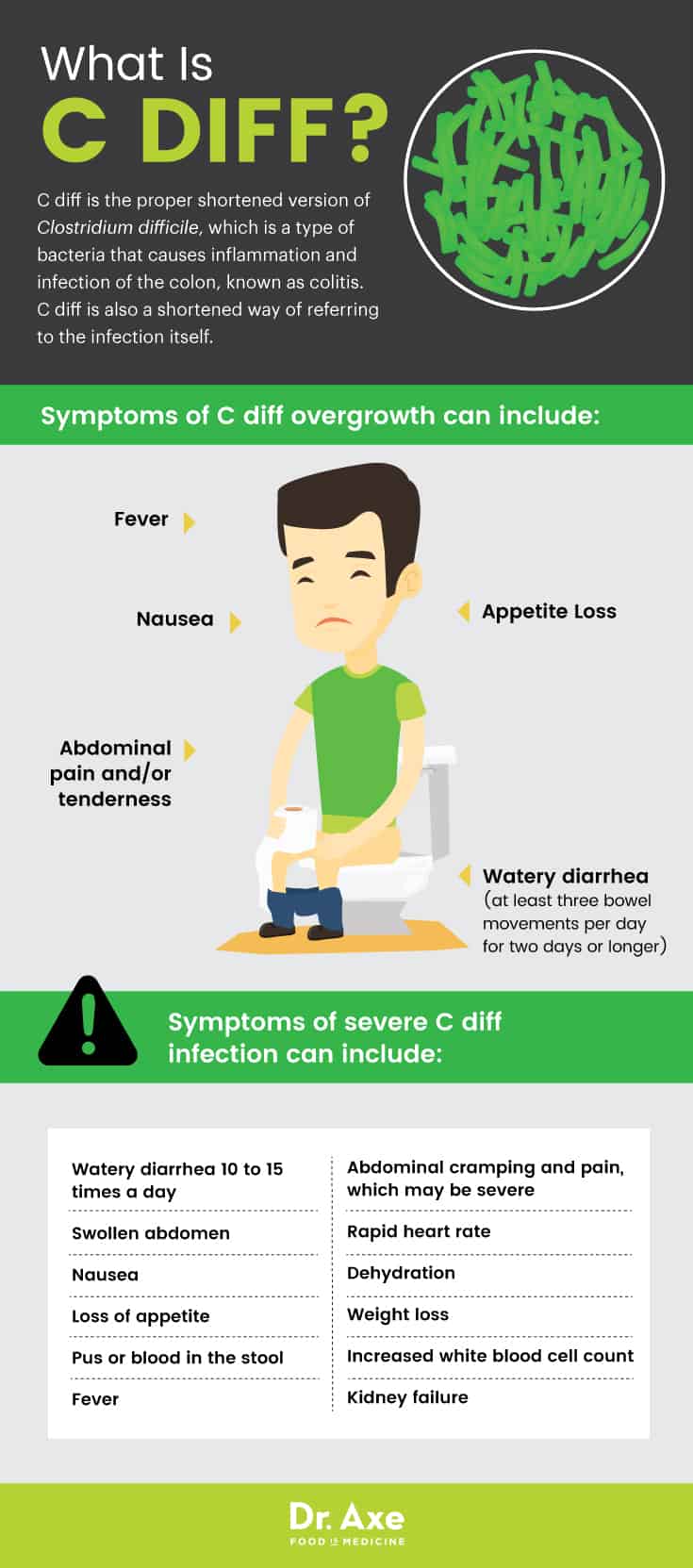
C. diff (sometimes mistakenly shortened to “c dif” or “cdif”) is the proper shortened version of Clostridium difficile [klo–strid–ee–um dif–uh–seel] (C. difficile), which is a type of bacteria that causes inflammation and infection of the colon, known as colitis. C. diff is also a shortened way of referring to the infectious colitis itself. Clostridium difficile colitis is the full name for the colon infection caused by C. diff bacterium. This strain of bacteria can cause symptoms in the body ranging from diarrhea to life-threatening cases of C. diff colitis or C. diff infection.
The bacteria can be found in human intestines as well as in soil, water and animal feces. Does everyone have C. diff? It’s estimated that up to 3 percent of adults and 66 percent of babies harbor the bacteria without it being symptomatic. For humans, the large intestine normally contains many good bacteria that keep it healthy. For people with C. diff in their intestines, they may not have any issue if the good bacteria keeps the Clostridium difficile in check. However, a C. diff infection can occur when the balance of bacteria in the body gets thrown off, most commonly by taking antibiotics. When you take antibiotics, it not only kills off the bad bacteria causing your sickness, it also kills off the vital good bacteria that is key to gut health as well as overall health! Some experts also believe that antibiotics can trigger the C. diff bacteria to release the toxins that can be so damaging to the colon.
How long is a person contagious with C. diff? There is no exact answer to this question because it depends on the person, their line of treatment and how well the body fights off the infection. What we do know for sure is that the spores of C. diff (from an infected person’s stool) can last a very long time. Research shows that C. difficile spores can be shed to the environment by both asymptomatic and symptomatic patients and may survive for up to five months on inanimate surfaces. So how contagious is C. diff? It’s quite contagious if you come in contact with a person or surface that contains the infectious spores.
Common Signs and Symptoms of C. Diff
Many people have Clostridium difficile living in their intestines and the bacteria doesn’t cause any problems for them. When kept in check by other good bacteria, C. diff may not cause any symptoms at all. However, when something (most often antibiotic usage) throws off the balance of bacteria in the body, this is when a problem can occur and C. diff can start growing rapidly.
What is the typical C. diff incubation period? Three days is considered to be the median incubation period of C. difficile. According to Mayo Clinic, “Signs and symptoms usually develop within five to 10 days after starting a course of antibiotics, but may occur as soon as the first day or up to two months later.”
What are the first signs of C. diff? The most common initial symptoms of an infection are mild abdominal cramping and tenderness along with diarrhea (C. diff stool appearance is watery) that occurs three or more times per day for two or more days. Why does this happen? C. difficile bacteria can release toxins that attack the lining of the colon by not only destroying cells, but also creating patches of inflammatory cells that cause watery diarrhea.
Symptoms of an overgrowth of C. diff can include:
- Watery diarrhea (at least three bowel movements per day for two days or longer)
- Foul-smelling stool (What does C. diff smell like? C. diff poop is known to have a very strong odor)
- Appetite loss
- Nausea
- Fever
- Abdominal pain and/or tenderness
With a C. diff infection, the colon becomes inflamed, which is medically referred to as colitis. Sometimes the colon become even more damaged by the release of toxins from the the overgrowth of the C. diff bacteria. If this happens, the colon can develop patches of raw tissue that may bleed or pus, which is called pseudomembranous colitis. There are also a greater number of symptoms and more severe symptoms if a Clostridium difficile infection escalates to this level. Most of the time, pseudomembranous colitis is caused by C. diff.
Symptoms of a severe C. diff infection can include:
- Watery stool 10 to 15 times a day
- Abdominal cramping and pain, which may be severe
- Swollen abdomen
- Nausea
- Loss of appetite
- Pus or blood in the stool
- Fever
- Rapid heart rate
- Dehydration
- Weight loss
- Increased white blood cell count
- Kidney failure
How serious is a C. diff infection? With severe cases, it’s common for people to become so dehydrated (from c. diff diarrhea) that they need to go to the hospital to prevent further complications such as kidney problems. A C. difficile infection can also cause a toxic megacolon, which means the colon dilates, cannot release gas or stool and can potentially rupture as a result. A toxic megacolon can lead to death if emergency surgery does not occur promptly. Another possible complication of c. difficile colitis is bowel perforation (a hole in the large intestines that allows dangerous bacteria to escape), which can cause a dangerous infection called peritonitis.
Does having a past infection make a person immune? Unfortunately, it does not … You can be re-infected with the C. diff bacteria or dormant spores.
Causes and Risk Factors
What causes C. diff? A C. diff infection is caused by C. difficile bacteria, which can be found in several common places, including human and animal feces as well as soil, air and water. The bacteria can also be found in some foods such as processed meat. The human intestines have somewhere around 100 trillion bacterial cells and up to 2,000 different kinds of bacteria. Much of this bacteria is good because it keeps possibly problematic bacteria in check and guards the body against infection. According to Mayo Clinic, “A small number of healthy people naturally carry the bacteria in their large intestine and don’t have ill effects from the infection.”
So when does C. diff bacteria become problematic and also symptomatic? It’s when C. diff is not kept under control and begins to overgrow. Antibiotics are the most common reason this can occur, since antibiotics not only kill the bacteria they are aiming to kill, but also all the good bacteria as well. Antibiotics that most commonly lead to this type of infection include fluoroquinolones, penicillins, cephalosporins and clindamycin.
Is C. diff contagious? Spores from the C. diff bacteria are passed in the feces and then can spread to food, objects and surfaces when infected individuals do not thoroughly wash their hands after going to the bathroom. If you touch something that has been contaminated with the C. diff spores, you may end up unintentionally and unknowingly swallowing the C. diff bacteria. Hospitals and long-term care facilities are especially problematic because healthcare workers can unintentionally spread C. diff between patients if they do not properly wash their hands after caring for each patient. The other tricky fact about C. diff spores is they can live on objects and surfaces outside of the body for weeks or even months.
C. diff causes and risk factors include:
- Antibiotic use (absolutely the #1 risk factor), especially a broad-spectrum antibiotic or any antibiotic used for an extended period of time
- Hospitalization
- Living in a nursing home or extended-care facility
- Gastrointestinal tract surgery
- Abdominal surgery that requires moving the intestines aside
- Living in a nursing home or extended-care facility
- Colon health issues, such as inflammatory bowel syndrome or colorectal cancer
- Having a weakened immune system
- Previous C. diff infection
- Being 65 years of age or older
Some studies have also shown that stomach acid-reducing drugs, especially proton pump inhibitors (or PPIs), may likely play a role in the recurrence of C. diff infections.
Natural C. Diff Treatment (Plus, the C. Diff Diet)
Can C. difficile go away on its own? According to some medical doctors, the infection can go away on its own and sometimes people are less likely to have a recurrence if not treated. However, even mild C. diff symptoms mean that your system is clearly off and could use a boost. If you’re wondering how to treat C. diff at home, there are a lot things you can do to help fight off this intestinal infection. The following are some of the natural approaches, including an anti-C. diff diet, that can really help to fight an infection.
1. Stop Antibiotics Whenever Possible
Natural as well as conventional C. diff guidelines include stopping any antibiotic medications you are currently taking. Even the CDC recommends that one of the first things you want to do when you find out you have a C. diff infection is to stop taking any antibiotics you are currently on “whenever possible.” These antibiotics are killing off the good bacteria in your body, and this is exactly what C. diff bacteria wants; they want the good bacteria decreased so they can overgrow and take over. Stopping other antibiotics can provide noticeable improvement in C. diff symptoms, especially diarrhea, quite quickly. Be sure to consult with your healthcare practitioner before stopping medications, however.
2. Load Up On Good Bacteria
Should you take probiotics when you have C. diff? Probiotics can help so much that both conventional and natural health experts will recommend taking probiotic supplements if you have a C. diff infection. There has been mixed evidence that certain strains of probiotics — namely Lactobacillus and Saccharomyces species — may be particularly helpful.
While trying to fight off (as well as avoid) a C. diff infection, one of the most important things you can do is to make sure you’re putting probiotic or “good bacteria” into your system on a daily basis since too much bad bacteria is what got you in trouble in the first place. Taking a high-quality probiotic supplement regularly is an excellent idea, especially if you currently are or recently have been on antibiotics.
Can probiotics get rid of C. diff? They can help majorly in both supplement and food form. You can get a lot of probiotic from your diet if you eat probiotic-rich foods that will help to balance your intestinal flora and fight C. diff. Some top probiotic foods to consume regularly are raw apple cider vinegar, fermented vegetables (sauerkraut, kimchi and kvass) as well as probiotic beverages (kombucha and coconut kefir). To get the most out of apple cider vinegar, make sure you buy a raw variety with the “mother” intact, which means it still contains all its beneficial compounds, including probiotics. Does apple cider vinegar cure C. diff? Not necessarily, but it can certainly help to boost the good bacteria that is key to any anti-C. difficile diet.

3. Avoid or Reduce Certain Foods
What foods should be avoided with C. diff? According to the C. Diff Foundation, avoiding the following foods can be helpful when fighting an infection:
- Dairy products, which have been known to cause additional gastrointestinal upset … Lactose intolerance has also been known to occur during a C. diff infection.
- Greasy, fatty foods and processed foods that are not easy on the digestive system and may lead to more diarrhea
- Some foods that are definitely healthy but may cause extra bloating, gas and discomfort such as cruciferous veggies (like broccoli and cabbage), onions, beans, nuts, seeds and whole grains
- Raw fruits and veggies (Cook them to reduce the likelihood of bloating effects)
- Processed fat-free foods like olestra, which have been known to cause more bloating and increased bouts of diarrhea
- Spicy foods, which are known to increase symptoms
- Large quantities of caffeine since caffeine has diuretic effects, can bother the GI tract and lengthen recovery from infection
The C. Diff Foundation states, “No two bodies are created nor respond alike, making diets a very individualized program,” which is so important to remember and why it’s wise to pay attention to your body and how it reacts to what you eat when you have an infection (and in general). Be sure to consult with your healthcare provider about an appropriate C. diff diet for you.
4. Thorough Hand Washing
If you have a Clostridium difficile infection, you’ll want to do what you can to prevent the spread of the infection to others and also to avoid your own reinfection with C. diff. Thorough hand washing with soap and warm water for 30 to 40 seconds is one of the most important precautions to take if you have an infection or you want to avoid an infection. When washing your hands, make sure to get in between the fingers, the tops of hands and thumbs. Once you’re done washing, dry hands thoroughly with a clean, dry towel. It’s also ideal to turn off the sink faucets with a clean towel. Proper hand washing has been shown to be more effective than alcohol-based hand cleansers. (17)
When I recommend hand washing, I am never suggesting using antibacterial soaps, not even when it comes to C. diff. Even the FDA will tell you that you should pass on the antibacterial soap (which only increases antibiotic-resistant bacteria) and just use good old soap and water.
5. Shut the Lid
Another smart habit to get into if you want to prevent reinfection or the spread of C. diff is to close the lid of the toilet before you flush. I know you may not be able to do this in public restrooms, but at home, make sure to always close the lid before you flush. This can greatly decrease C. diff bacteria from finding their way to all kinds of surfaces and objects in the bathroom. In general, it’s just a really helpful practice to get into for sanitary and health purposes.
6. Consume Natural Antibiotics
If you’re looking for ways to get more natural antibiotics in your diet to fight off C. diff, here are some of the top natural bacteria killers you may want to consider when trying to fight off invaders like C. diff naturally:
Manuka honey: Not only has Manuka honey been shown to be a really powerful antibacterial agent, research has also shown its ability to reduce inflammation in the colon.
Raw garlic: Garlic inherently has antimicrobial, antiviral and anti-fungal properties. For general health promotion for adults, the WHO actually recommends incorporating garlic into your life on a daily basis in one of the following forms: two to five grams (about one clove) of fresh garlic, 0.4 to 1.2 grams of dried garlic powder, two to five milligrams of garlic oil, 300 to 1,000 milligrams of garlic extract or other formulations that are equal to two to five milligrams of allicin. Onions are great too.
Oil of Oregano: Research has shown that the oregano essential oil “may be an effective treatment against dangerous and sometimes drug-resistant bacteria.” Oregano oil is extremely strong, so it is best used under the guidance of a natural health expert. When taken internally, oregano oil always needs to be diluted with water or mixed with coconut oil. You can also incorporate dried and fresh oregano herb into your diet.
7. Fecal Transplant (Surgical)
The CDC website states, ” Transplanting stool from a healthy person to the colon of a patient with repeat C. difficile infections has been shown to successfully treat C. difficile. These “fecal transplants” appear to be the most effective method for helping patients with repeat C. difficile infections. This procedure may not be widely available and its long-term safety has not been established.”
I know this may sound really out there, but this process called a fecal transplant is actually both a conventional and holistic approach to reoccurring C. diff infections. What exactly is a fecal transplant? It’s basically a procedure that takes the fecal matter (stool) from a healthy donor, mixes it with a liquid solution, strains it and then puts it into the colon of another patient using an enema, colonoscopy or endoscopy. A recurrent C. diff infection (typically at least three or more) is actually one of the top health concerns that warrants such a transplant. On average, fecal transplantation is said to result in a 91 to 93 percent success rate, while some studies have even shown a 100 percent success rate when fresh fecal microbiota is used.
8. Fecal Transplant (Oral)
If you’re suffering from reoccurring C. difficile infections, there is a less invasive fecal transplant option. Recently, successful fecal transplants have been performed by encapsulating healthy freeze-dried fecal matter and having patients ingest the capsules. A 2017 study published in The American Journal of Gastroenterology found that just one administration of the capsules to 49 patients with reoccurring C. diff resulted in 88 percent of the patients achieving “clinical success,” which was said to be no recurrence of a C. diff infection over a two month time period.
Diagnosis
A person is diagnosed with C. diff based on medical history, signs and symptoms along with test results. A diagnosis of C. difficile is often suspected if someone has recently (within the last two months) taken antibiotics or when C. difficile symptoms (especially watery diarrhea) begin a few days after a hospitalization.
How can you find out if you have an intestinal infection like C. diff? Is there a C. diff test? A stool sample test is typically the best way to start figuring out if you have an overgrowth of C. diff bacteria. Additional tests including an X-ray or a CT scan of your colon may be required as well. The interesting thing is that you can be a carrier of C. diff but not actually have an infection of C. diff. So this mean you can test positive and have zero symptoms, but if you test positive and you have symptoms, then you have an active case of C. diff.
Conventional Treatment
Conventional treatment typically includes antibiotics, but more recently, even conventional recommendations now include taking probiotics along with antibiotics to prevent a C. diff infection from happening again. Fecal microbiota transplantation may also be recommended if antibiotics do not help or your infection keeps coming back.
Can you be cured of C. diff? You can get rid of a Clostridium difficile infection. However, for some people, the infection may come back after treatment ends. According to the Agency for Healthcare Research and Quality, out of every 10 people who have had a C. diff infection in the past, as many as three to six people will have it again.
It’s a terrible fact that for some C. diff patients, the infection doesn’t just come back once, but again and again. You can imagine how difficult that must be on a person’s body. When the infection comes back the first time, the same antibiotic is typically used, but if the infection comes back more than once, then stronger antibiotics are employed.
How long does it take to recover from C. diff? This depends upon many factors including the person’s age, health status and course of treatment.
Precautions and Possible Complications
It’s a good idea to get tested for C. diff if you exhibit symptoms, especially if symptoms occur during or after taking antibiotics or after being around someone that you know has a C. diff infection.
What complications can C. diff cause? If the infection worsens, you may become seriously dehydrated, be unable to pass stool and/or experience weight loss. C. diff can also lead to a toxic megacolon, which may require emergency surgery or bowel perforation, which can lead to a dangerous infection called peritonitis. Can C. diff kill you? Rarely, a C. diff infection can lead to a hole in the intestines or sepsis, which can be deadly. In severe cases, surgery may be required to remove the infected part of the colon.
Can you kiss someone with C. diff? It’s usually considered OK to kiss and hug someone with C. diff since the infection is not typically spread through touching, and it also is not spread through the air by things like sneezing or coughing. However, if you visit someone hospitalized with C. diff, you should take some key C. diff precautions, including wearing gloves while in the room and washing your hands before leaving their room. Wearing gloves and practicing good hand washing hygiene is also very important for people who work in hospitals and long-term care facilities.
Always consult your doctor before making any changes to your diet or using any natural supplements, especially if you are pregnant, nursing, being treated for any ongoing health concerns or are currently taking medication.
Final Thoughts
- People who take antibiotics are most at risk for developing C. difficile infections, especially people who take antibiotics for long periods of time or take broad spectrum antibiotics.
- The stools of people with C. diff smell foul, are watery and are passed frequently. A mild case may result in at least three bowel movements per day for two days or longer, while a severe infection can cause watery diarrhea 10 to 15 times a day.
- Conventional and holistic medical experts agree on one of the top ways to treat C. diff: stop taking antibiotics whenever possible once you realize you have a C. diff infection and in general, don’t take antibiotics if you don’t need to.
- However, conventional treatment for C. diff typically and ironically includes taking more antibiotics.
- One of the best ways to prevent initial and re-infection with C. difficile bacteria is to wash your hands thoroughly.
- There are some healthy foods you may want to temporarily avoid while you have C. diff symptoms, while there are some foods (like highly processed ones) that are just a good idea to avoid as much as possible in general.
- There are natural antibiotics found in nature that you can incorporate into your diet that are proven to be highly potent and effective against bacteria like C. difficile.
- Conventional and holistic wisdom also agrees that fecal matter transplants (surgically or orally) are highly effective for patients with reoccurring infections.










