This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Dyslipidemia Causes + 5 Tips to Manage It Naturally
September 19, 2017
Dyslipidemia is a group of disorders characterized by changes in plasma lipids or lipoproteins, including two we are familiar with: cholesterol and triglycerides. The goal for adults over 20 years old is to have cholesterol levels that are below 200 milligrams per deciliter (mg/dL). However, nearly 99 million Americans are estimated to have total blood cholesterol levels higher than this “healthy” range, according to the American Heart Association. (1)
The Centers for Disease Control and Prevention (CDC) reports that people with high total cholesterol have approximately twice the risk for heart disease as people with ideal levels. But less than half of adults with high LDL cholesterol are getting treatment to lower their levels and reduce their cardiovascular disease risk. (2)
What are the most common causes of dyslipidemia (high cholesterol or high triglycerides)? These include both genetic factors and lifestyle habits — such as eating a highly-processed diet, taking certain medications, and being very sedentary.
Once dyslipidemia is diagnosed, experts agree that making lifestyle changes to prevent further complications should be priority number one. Natural treatments for dyslipidemia can include:
- Taking steps to lower inflammation levels
- Improving your diet, regularly getting enough exercise
- Managing sources of physical and emotional stress
What about drugs used to treat dyslipidemia? Lipid-lowering drugs, while now prescribed to millions of adults, are not considered a good treatment option for many people. Plus they can potentially cause a number of side effects. But when a patient with dyslipidemia has a higher risk for developing cardiovascular disease, their doctor might feel that the good outweighs the bad when it comes to the drugs’ effects. When needed — and after other treatment approaches have failed to help — someone with dyslipidemia might need one or more medications to prevent disease progression, especially coronary heart disease.
What Is Dyslipidemia?
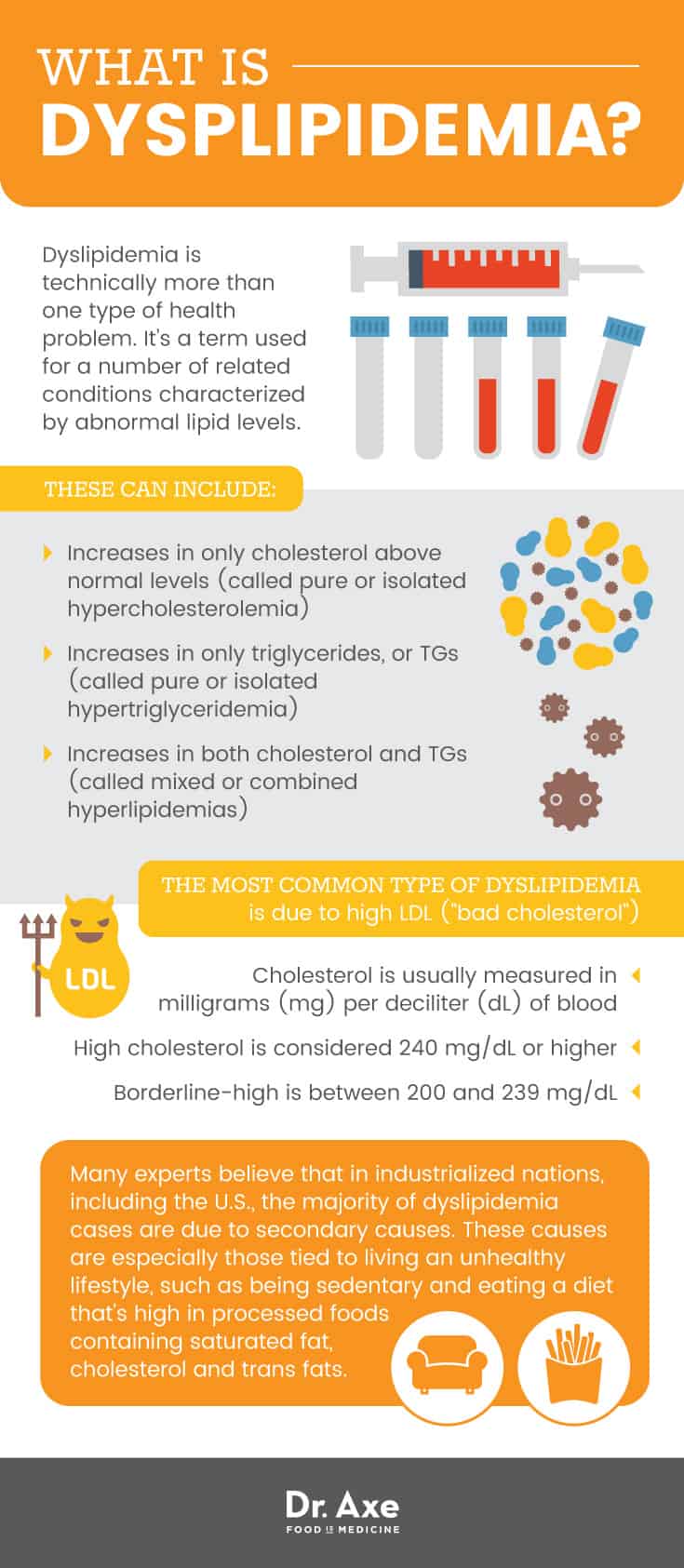
The definition of dyslipidemia is “elevation of plasma cholesterol, triglycerides (TGs), or both, or a low high-density lipoprotein level.” (3) Dyslipidemia is also sometimes called hyperlipidemia. This refers to high cholesterol. Dyslipidemia is a known risk factor of cardiovascular disease (CVD). It can contribute to heart problems — including the development of atherosclerosis (or hardening of the arteries), among others — which are the leading cause of death in the United States. Some studies have found that treatment of dyslipidemia can reduce the risk of heart disease by about 30 percent or more over a five-year period. (4)
Dyslipidemia is technically more than one type of health problem. It’s a term used for a number of related conditions characterized by abnormal lipid levels. These can include:
- Increases in only cholesterol above normal levels (called pure or isolated hypercholesterolemia).
- Increases in only triglycerides, or TGs (called pure or isolated hypertriglyceridemia).
- Increases in both cholesterol and TGs (called mixed or combined hyperlipidemias).
The most common type of dyslipidemia is due to high LDL (also called “bad cholesterol”) levels, which is sometimes genetically inherited (called familial hyper-cholesterolemia). But it also can be caused by unhealthy habits or other diseases. Many times no symptoms are present, but complications can still occur.
Low levels of HDL “good cholesterol“ is another component of dyslipidemia, in addition to having high triglycerides. These conditions have similar causes to high LDL cholesterol (genetics, poor diet, obesity, medication use, etc.)
What exactly are lipids?
Lipids are fat molecules that are soluble, non-polar organic solvents and insoluble in water. (5) Lipids found inside the human body are classified into eight categories: fatty acyls, glycerolipids, glycerolphospholipids, sphingolipids, sterol lipids, prenol lipids, saccharolipids, and polyketides.
- The underlying issue contributing to dyslipidemia is abnormal lipid metabolism. Lipid metabolism is essential for survival and includes the biological processes called dietary lipid absorption, lipogenesis, and lipolysis.
- Lipid molecules have many roles in the body, so they are essential for life and not inherently bad. We actually need a certain amount of cholesterol for our health not to suffer.
- Lipids help with functions such as: providing energy storage, signal transduction, building cellular structures, production of hormones and steroids, activating enzymes, supporting brain function, and absorbing other dietary lipids and fat-soluble vitamins, including vitamins A, D, E and K.
- Cholesterol and triglycerides are carried around the body within lipoproteins.
- The types of lipids that are associated with dyslipidemia include fatty acids, cholesterol, phospholipids, triglycerides and plant sterols. When levels of these lipids fall outside of the “normal range” then dyslipidemia is diagnosed.
Lipid absorption takes place when fats are consumed from the diet. Lipogenesis occurs in the liver and in adipose tissue (body fat) and includes the processes of fatty acid and triglyceride synthesis. Both of these are regulated by changes in diet along with fluctuating levels of glucose, insulin and glucagon. Lipolysis is the hydrolysis of triglycerides to fatty acids and glycerol. The process is stimulated by beta-adrenergic molecules and suppressed by insulin.
The role of dysfunctional lipid metabolism in causing dyslipidemia is one reason why eating a healthy, anti-inflammatory diet that has a balance of fatty acids is so important for resolving the problem.
Signs & Symptoms of Dyslipidemia
How serious is dyslipidemia, and what types of symptoms might it cause?
There’s a range of hyperlipidemia disorders that adults can develop, some more serious than others. When dyslipidemia is mild, someone might not have any symptoms at all (they are asymptomatic). But others have a much more severe case that can be life-threatening and require immediate and ongoing care.
When symptoms of dyslipidemia do occur, the person often also suffers from other diseases/disorders related to dyslipidemia. These include: vascular disease, coronary artery disease (CAD), stroke, and peripheral arterial disease. Symptoms can include:
- Abdominal pain, nausea and vomiting.
- Eruptive xanthomas (lesions of small red or yellow capsules), most commonly on the feet, knees, elbows, the back or buttocks.
- Muscle and bone pains.
- Memory loss, confusion and other neurological problems in severe cases.
- A white, creamy appearance to retinal arteries and veins.
- Neuropathy.
- In some cases symptoms associated with heart disease or even strokes, such as chest pains, difficulty breathing, numbness and tingling in the arms.
Dyslipidemia is more likely to lead to complications when someone has other cardiovascular disease risk factors. These risk factors can include a history of hypertension (high blood pressure), metabolic syndrome, obesity, diabetes, and family history of premature coronary heart disease (CHD).
Complications due to dyslipidemia can include:
- Higher risk for heart disease. Hyperlipidemia, the condition that refers to elevated plasma atherogenic lipids and lipoproteins, can result in the formation of plaque inside the arteries (atherosclerotic plaques), which contributes to the development of atherosclerosis and coronary artery disease (CAD).
- Having low plasma levels of anti-atherogenic HDL-cholesterol (sometimes called “good cholesterol”) is associated with higher risk for heart disease.
- When triglycerides are very elevated, higher risk for pancreatitis and hepatosplenomegaly.
Dyslipidemia Causes & Risk Factors
The underlying causes of dyslipidemia are both genetic (considered primary causes) and lifestyle-related (considered secondary causes).
Many experts believe that in industrialized nations, including the U.S., the majority of dyslipidemia cases are due to secondary causes. These causes are especially those tied to living an unhealthy lifestyle, such as being sedentary and eating a diet that’s high in processed foods containing saturated fat, cholesterol and trans fats.
Contributing factors that can lead to dyslipidemia can include one or more of the following:
- Genetic inheritance. Certain gene mutations can cause overproduction or defective clearance of triglycerides, high LDL cholesterol, or underproduction/excessive clearance of HDL cholesterol.
- Other existing medical conditions that interfere with normal lipid levels, such as diabetes, vascular disease or obesity.
- Poor diet, such as one high in processed foods, fast foods, trans fats, and saturated fat or cholesterol from unhealthy sources. Trans fats are polyunsaturated or monounsaturated fatty acids to which hydrogen atoms have been added. Despite correlation with a number of health problems, they are still used in many processed foods to help improve texture, shelf life and flavor.
- A sedentary lifestyle with too little activity and exercise.
- High alcohol consumption.
- Kidney or liver disease.
- Hypothyroidism.
-
Use of certain medications/drugs including: thiazides, beta-blockers, retinoids, highly active antiretroviral agents, cyclosporine, tacrolimus, estrogen and progestins, and glucocorticoids.
- Cigarette smoking or use of tobacco/nicotine.
- Using anabolic steroids.
- HIV infection.
- Nephrotic syndrome.
Diabetes is considered a “significant secondary cause” of dyslipidemia. This is because research shows that a high percentage of diabetic patients — especially those with type 2 diabetes — have a combination of high TG, high small, dense LDL fractions, and low HDL cholesterol. Those who have “diabetic dyslipidemia” are at high risk of developing complications when their disorder is not well-controlled. For example, complications are more likely if risk factors persist, such as increased caloric intake, lack of physical activity, and high amounts of exposure to toxins or stress.
Conventional Treatment for Dyslipidemia
The goal of treatment for dyslipidemia is preventing progression of diseases including: atherosclerotic cardiovascular disease (ASCVD), acute coronary syndromes, stroke, transient ischemic attack, or peripheral arterial disease.
Your doctor can help diagnose you with dyslipidemia, or rule the condition out, by measuring your blood levels of different lipids. A “total lipid profile” is determined by measuring lipid and lipoprotein concentrations in the blood, typically after a 12-hour fast. Plasma lipids and lipoprotein concentrations usually measured to test for dyslipidemia include: total cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides. Depending on if your symptoms point to any other disorders, your doctor may also want to measure levels of fasting glucose, liver enzymes, creatinine, thyroid-stimulating hormone (TSH), and urinary protein.
What Qualifies as High Cholesterol?
According to the Merck Manual website:
There are no numeric definitions of dyslipidemia; the term is applied to lipid levels for which treatment has proven beneficial. Proof of benefit is strongest for lowering elevated low-density lipoprotein (LDL) levels … evidence is less strong for a benefit from lowering elevated triglycerides and increasing low high-density lipoprotein (HDL) levels.
Cholesterol is usually measured in milligrams (mg) of cholesterol per deciliter (dL) of blood. High cholesterol is considered total cholesterol levels of 240 mg/dL or higher. Borderline-high is between 200 and 239 mg/dL. Treatment is usually recommended when one or more of these risk factors apply:
- LDL cholesterol above 70 to 80 mg/dL (1.81 to 2.07 mmol/L) for people who have CVD and have multiple major risk factors.
- Very high TG levels (>500 to 1000 mg/dL or 5.65 to 11.3 mmol/L), especially if combined with LDL cholesterol or low HDL cholesterol levels, or a strong family history of heart disease.
- LDL level above 100 mg/dL (2.59 mmol/L) in people with diabetes.
Medications Used to Treat Dyslipidemia:
Treatments for dyslipidemia will usually include lifestyle changes — such as making dietary changes and increasing exercise — sometimes along with taking several drugs to treat very high cholesterol or triglyceride levels, when needed. The American Heart Association (AHA) guidelines recommend using drug treatment for certain groups of patients who are at high risk for heart disease after discussion of contributing factors and the benefits of statin therapy.
- For high LDL cholesterol, medications that may be used include: statins, bile acid sequestrants, ezetimibe, niacin, and possibly others. Statins are recommended for four groups of patients, with any of the following: diagnosed ASCVD; LDL cholesterol ≥ 190 mg/dL; with an age between 40 to 75 AND LDL cholesterol 70 to 189 mg/dL; and an estimated 10-year risk of ASCVD that is greater than 7.5 percent.
- For high TGs, medications can include niacin, fibrates, omega-3 fatty acids, and sometimes others.
- While increasing HDL cholesterol levels might be helpful for some people, this isn’t always necessarily the case. HDL levels do not always predict cardiovascular risk and don’t always need to be treated. For example, when someone has a genetic disorder that causes low HDL levels, they are not necessarily at any greater risk of developing cardiovascular disorders if they don’t have other risk factors or poor lifestyle habits.
- If a patient has the type of dyslipidemia called chylomicronemic that is causing acute pancreatitis, then they may need to be hospitalized or treated with insulinization.

5 Natural Management Tips for Dyslipidemia
1. Eat an Anti-Inflammatory Diet
Dietary intervention is usually the mainstay treatment for patients with dyslipidemia. Some doctors will recommend their patients work on losing weight in a healthy way if they are overweight or obese. But no matter what a person’s weight is, if they have dyslipidemia, they should always focus on making dietary improvements.
While opinions differ in regards to how much fat/cholesterol someone with dyslipidemia should include in their diet, most authorities such as the National Heart, Lung, and Blood Institute’s (NHLBI), recommend the following dietary changes: (6)
- Limiting intake of dietary saturated fats to about 7 percent or less of total calories. It’s advised that people with dyslipidemia limit cholesterol intake to below about 200 milligrams per day.
- Getting between 25–35 percent of the day’s total calories from combined sources of fat.
- Limiting sodium intake to 2,400 milligrams a day.
However, in my opinion, one of the things you should focus on most is avoiding processed foods that increase cholesterol due to how they cause inflammation. Healthy fats should not be feared. But rather the emphasis should be on including high-quality sources as part of a balanced diet.
Other than managing intake of certain types of fats, diet-related changes to help lower cholesterol and triglycerides include:
- Eliminating foods like: refined vegetable oils, potato chips and other snacks cookies and sugary treats, bacon and processed meats, most low-quality conventional dairy products and refined grains.
- Increasing intake of fiber, especially soluble fiber, from high-fiber foods like: leafy green veggies; beans and legumes; artichokes; chia and flax seeds; nuts like almonds and walnuts; sweet potatoes and squash; avocado, berries, apples, pears and other fruits.
- Replacing processed carbohydrates — those made with refined grains and sugar — with complex carbohydrates. Examples include ancient whole grains, whole fruit, beans, legumes and starchy vegetables.
- Avoiding foods and drinks with concentrated sugar and alcohol, such as soda/soft drinks, packaged desserts, sweetened dairy products, etc.
- Having wild-caught fish two to four times per week to increase intake of omega-3 fatty acids. This includes fish like wild salmon, herring, sardines, trout, halibut or tuna.
- Eating an amount of calories that helps you maintain an ideal range of body weight based on your height and build.
If you have low HDL cholesterol (the kind most consider to be the “good cholesterol”), you may be able to increase your level by eating foods that are high in healthy fats, such as: real dark cocoa, grass-fed beef, eggs and fish.
2. Get Enough Appropriate Exercise
To help with reducing inflammation, regulating hormones and possibly reaching a healthier weight, regular physical activity is almost always recommended. Regular exercise can lower high LDL cholesterol in some people and also helps maintain ideal body weight. And certain studies have found triglyceride concentrations can decrease by about 30 percent after someone follows a regular exercise program. (7)
People with dyslipidemia who are mostly sedentary will usually need to start slowly and increase their exercise load gradually as their body adjusts. Aiming to start with about 30–60 minutes of moderate exercise per day, such as walking, swimming or biking, is a good jumping-off point. Lifting weights, dancing and doing yoga or pilates are other options. Working with a personal trainer can also be very helpful if you’re dealing with some limitations and are not sure how to begin.
3. Treat Contributing Health Conditions (Including Diabetes)
Treatment for dyslipidemia should always include correction of underlying health issues that increase risk for serious diseases, such as high blood pressure (hypertension) and diabetes. Lifestyle changes are considered the first step towards recovering from these types of common health problems. Changes can include exercising, eating a healthy diet, using medications or supplements if they might be helpful, and limiting exposure to toxins.
4. Limit Alcohol, Tobacco & Drug Use
Quitting smoking, not drinking high amounts of alcohol, and not using any recreational drugs are important to prevent progression. These habits can contribute to other health problems, such as diabetes, liver or kidney problems, along with increasing inflammation, which all make dyslipidemia worse.
5. Use Supplements, if Helpful
- Fish oil — Has anti-inflammatory effects that may help prevent problems such as high blood pressure or high cholesterol, which are related to heart disease.
- CoQ10 — May help regulate blood pressure.
- Garlic — May help to normalize blood pressure levels.
- Lipoid acid — An antioxidant that offers protection against LDL oxidation and hypertension. Also helps with recycling of other antioxidants in the body, including vitamins C, E and glutathione. (8)
- Fiber supplements such as psyllium husks (although you may get similar results from eating a high fiber diet) — Helps to lower cholesterol levels and protect the heart. May also help with digestion and preventing over-eating.
Final Thoughts on Dyslipidemia
- Dyslipidemia is a group of conditions characterized by elevated lipid levels, including elevated cholesterol and triglycerides.
- People with dyslipidemia are at greater risk for atherosclerosis, coronary artery disease and peripheral arterial disease.
- Causes of dyslipidemia include eating a highly processed/poor diet with excessive dietary intake of saturated fat, cholesterol, and trans fats; a sedentary lifestyle; genetic (familial) abnormalities related to lipid metabolism; existing health conditions, including diabetes, kidney disease or liver disease; smoking and high alcohol consumption; and use of certain medications.
- Natural treatments for dyslipidemia can include improving your diet; regularly getting enough exercise; and managing sources of physical and emotional stress that contribute to increased inflammation.
Read Next: Health Coaching: Skills, Training + Benefits of Working with One
[webinarCta web=”hlg”]








