This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Prevent Seizures Naturally: 3 Ways to Manage Epilepsy Symptoms
May 7, 2017
According to the Epilepsy Foundation, epilepsy (which means the same thing as “seizure disorders”) is the fourth most common neurological disorder in the world. It affects people of all ages and cultures. (1) 65 million people worldwide currently have epilepsy, including 3 million children and adults living in the U.S. About one in 26 people in the United States will develop epilepsy at some point in their lifetime, with 150,000 new cases diagnosed every year.
Epilepsy is not just one condition, but a term for a spectrum of neurological disorders that share common symptoms. Seizures, the hallmark of epilepsy, occur when there’s a sudden change in the way that brain cells communicate with each other. These communication changes cause abnormal signals and temporary changes in sensations, behaviors, motor control, movement and consciousness.
Although a lot remains unclear about the causes of seizures due to epilepsy, triggers seem to include certain environmental influences, experiencing a recent brain injury, and genetics/a family history of seizures. Treatments for epilepsy always depends on the severity of symptoms and an individual’s response to different treatment approaches. Typically symptoms of epilepsy are managed through use of anti-seizure medications along with lifestyle changes, such as following a keto diet.
What is Epilepsy?
The Epilepsy Foundation states that epilepsy is widely misunderstood by much of the public, especially the fact that “seizures and epilepsy are not the same.” (2) A seizure is “a disruption of the electrical communication signals between neurons in the brain.” While a seizure is a single neurological event affecting the nervous system, epilepsy is the chronic disease that causes recurrent, unprovoked (also called reflexive) seizures. Seizure disorder is a broader term that includes both single seizure episodes and several different types of epilepsy. According to the National Institute of Neurological Disorders and Stroke, “Having a single seizure as the result of a high fever (called febrile seizure) or head injury does not necessarily mean that a person has epilepsy.” (3)
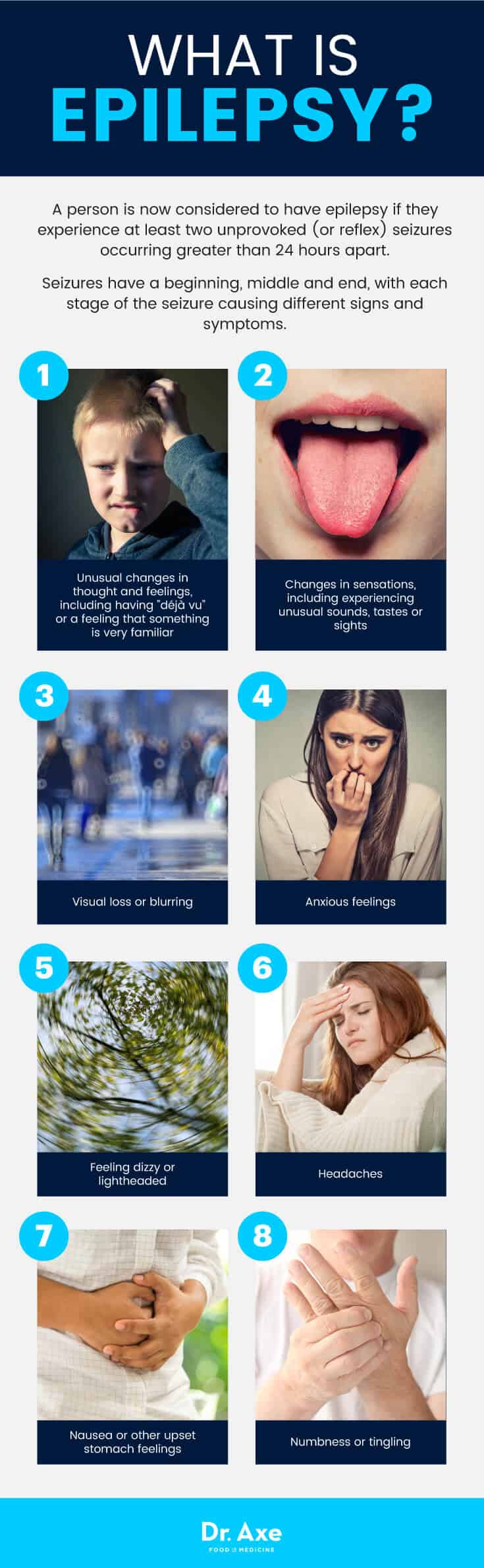
The definition of epilepsy is “A disease characterized by an enduring predisposition to generate epileptic seizures and by the neurobiological, cognitive, psychological, and social consequences of this condition.” The definition of epilepsy has changed over the past several decades. This change is due to some controversy over how to diagnose patients correctly. A person is now considered to have epilepsy if they experience at least two unprovoked (or reflex) seizures occurring greater than 24 hours apart.
Having one unprovoked (or reflex) seizure increases the risk that another will occur, especially within the following 10 years. There is still some debate among experts regarding the appropriate time to diagnose someone with epilepsy. After an initial seizure, some doctors wait for a second seizure before diagnosing epilepsy.
Many individuals who have had only one unprovoked seizure have other risk factors that make it very likely that they will have another seizure in the near future. So, certain doctors treat these patients like they are in fact suffering from epilepsy, even though they don’t technically meet the current definition.
The International League Against Epilepsy (ILAE) created the definition of epilepsy stated above in 2005. However, some experts feel that it doesn’t cover important aspects of epilepsy — such as the genetic component of the disease or the fact that some people overcome the condition.
Although epilepsy is a chronic disease, it can be “resolved” for certain individuals. Doctors consider a patient to no longer have epilepsy if they were diagnosed with an age-dependent epilepsy syndrome but then pass the applicable age. Epilepsy is also no longer considered active when a patient remains seizure-free for 10 years during a time when they had not been taking seizure medications to control symptoms for the previous 5 years.
Common Signs and Symptoms of Epilepsy & Seizures
Not only does epilepsy cause various types of seizures, which range widely in terms of the frequency that they occur and also their severity, but epilepsy can also increase the risk for other health problems in some cases. Seizures typically cause symptoms that include loss of awareness/consciousness, changes in moods and emotion regulation, loss of motor and muscle control, and convulsing or shaking. This can sometimes lead to falls, injuries, accidents, emotional/mood changes, complications during pregnancy or other secondary problems.
Seizures have a beginning, middle and end, with each stage of the seizure causing different signs and symptoms. Every patient experiences seizures differently. Not every person will have a clear separation between different stages, or every type of symptom described below.
Signs that a seizure may be starting:
- Unusual changes in thought and feelings, including having “déjà vu” or a feeling that something is very familiar
- Changes in sensations, including experiencing unusual sounds, tastes or sights
- Visual loss or blurring
- Anxious feelings
- Feeling dizzy or lightheaded
- Headaches
- Nausea or other upset stomach feelings
- Numbness or tingling
Symptoms of the “middle stage” of a seizure (called the ictal phase):
- Loss of awareness, unconsciousness, confusion, forgetfulness or memory lapses
- Hearing unusual sounds or experiencing strange smells and tastes
- Loss of vision, blurry vision and flashing lights
- Hallucinations
- Numbness, tingling or electric shock-like feelings
- Mood changes, especially anxiety/panic, which can accompany a racing heart
- Difficulty talking and swallowing, and sometimes drooling
- Lack of movement or muscle tone, tremors, twitching or jerking
- Repeated movements of the hands, lips, eyes and other muscles
- Convulsions
- Losing control of urine or stool
- Increased sweating
- Change in skin color (looks pale or flushed)
- Difficulty breathing normally
Symptoms at the end of or after a seizure (called the postictal phase):
- Sleepiness and confusion, which might go away quickly or linger for several hours or longer depending on the patient
- Confusion, memory loss, feeling fuzzy, light headed or dizzy
- Difficulty completing tasks, talking or writing
- Mood changes including feeling depressed, sad, upset, anxious or scared
- Headaches and nausea
- It’s possible to experience injuries if the seizure ends in falling, such as bruising, cuts, broken bones or head injury
- Feeling very thirsty and having a strong urge to go to the bathroom
Causes of Epilepsy and Risk Factors
In most cases (about 60 percent of the time) the exact cause of epilepsy remains unknown. Being either a child, or over the age of 60, puts someone at the greatest risk for seizures and epilepsy. Experts know that seizures caused by epilepsy are due to abnormal disturbances in electrical activity of the central nervous system (brain, neurons and spinal cord). It’s believed that some of the reasons that someone might develop epilepsy include: (4)
- Due to a brain injury
- Brain conditions that contribute to damage, including tumors, dementia or a stroke
- Genetics and a family history of seizures/epilepsy
- Abnormal brain development during infancy or in the womb. Reasons for this can include infection in the mother, poor nutrition during pregnancy, oxygen deficiency or cerebral palsy.
- An imbalance of nerve signaling chemicals called neurotransmitters, or changes in the brain channels that allow for normal cellular communication
- Infectious diseases that damage parts of the brain, such as meningitis, AIDS and viral encephalitis
- Use of drugs or high fevers can also cause seizures (which are not always tied to epilepsy). There’s some evidence that factors like high amounts of stress, anxiety, nutrient deficiencies or electrolyte imbalances, alcohol use and withdrawal effects may contribute to seizures in some cases. (6)
Conventional Treatments for Epilepsy
Conventional treatment for epilepsy depends on the patient’s condition and is always individualized by the patient’s team of physicians. Not every seizure or sign of epilepsy necessarily warrants treatment. What distinguishes single seizures from epilepsy is that patients with epilepsy may require chronic treatment (such as with antiepileptic medication or surgery). A single, isolated seizure is treated by identifying and managing the trigger (such as head injury or fever). (7)
Medications for Epilepsy:
Epilepsy can be diagnosed through testing including measurement of electrical activity in the brain and brain scans such as magnetic resonance imaging (MRI) or computed tomography. Some patients only experience mild epilepsy seizures, so they often choose to avoid taking medications in order to avoid unwanted side effects. While treatments have come a long way, still about one in three patients with epilepsy live with uncontrollable seizures because no available treatment effectively works for them.
For those who do respond well to medication treatments, a number of options, including anti-seizure drugs, are now available. Most medications are taken in pill form by the mouth to help control seizures due to neurological changes, sometimes in different combinations of 2–3 pills taken together. It can be a difficult process for patients with epilepsy to learn which types of drugs (or drug combinations) work best to control symptoms, since it differs from person to person.
Anti-seizure medications pose the risk for certain side effects, which can sometimes be very problematic. These can include:
- Fatigue
- Dizziness, instability, loss of coordination and confusion
- Weight gain
- Mood changes
- Skin rashes
- Speech problems
Surgery To Prevent Seizures:
When side effects due to anti-seizure medications become very bad, or the medications don’t work well enough to help the patient experience improvements in quality of life, other methods of controlling seizures will be used, including surgery or the treatments described below, such as the ketogenic diet and vagus nerve stimulation.
Surgery is most appropriate and effective when a patient’s seizures occur in parts of the brain that can removed or “cut” without causing interference with normal functions like motor function, speech or language, vision and hearing. Surgery can prevent seizures from spreading and worsening by isolating the area of the brain they impact. This involves removing a small part of the patient’s brain or making several cuts in certain neurons (this is called multiple subpial transection surgery). Surgery is typically a last resort option and very serious, due to risk for complications such as changes in mood regulation, learning, thinking or other cognitive abilities.
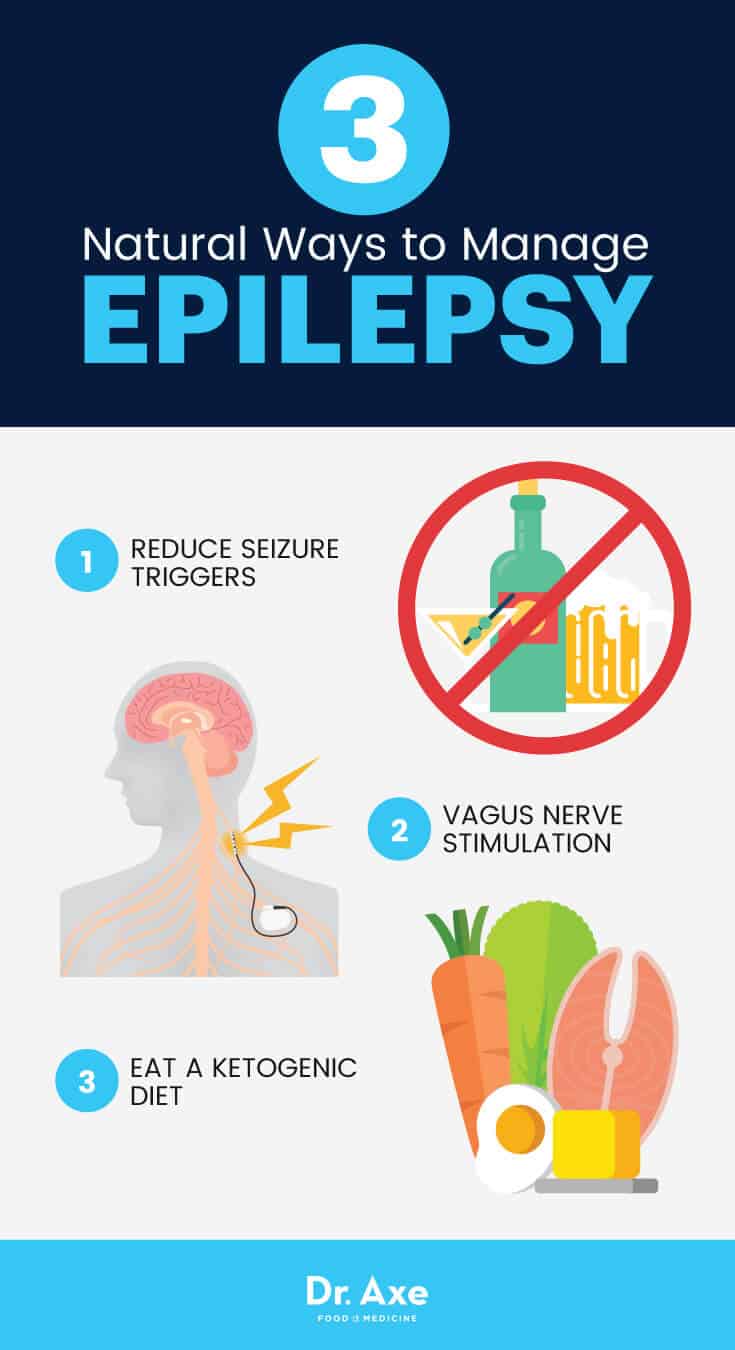
3 Natural Ways to Manage Epilepsy
1. Reduce Seizure Triggers
It’s not always possible to prevent a seizure from happening. But, there are certain steps you can take to help lower the odds by managing your individual triggers.
Some common seizure triggers to be aware of include:
- Increased in physical or emotional stress, anxiety, fatigue and lack of sleep: Try to find ways to relieve stress and make sure to get enough sleep (seven to nine hours per night for most adults).
- Use of alcohol or drugs, or side effects from quitting either of these.
- Changing or skipping medications, especially anti-seizure medications that are needed: Always take medications as directed, otherwise you might risk a seizure.
- Being overstimulated by lights, loud noises, television, or screens like televisions, electronics and computers: Take breaks from screen time. Work on finding a balance between work and “play” to reduce mental strain and fatigue.
- Experiencing hormonal imbalances or changes, such as during pregnancy, puberty or menopause: Eat a healthy diet, get enough rest and control stress to make these transitions easier.
2. A Ketogenic Diet
A ketogenic diet has been used since the 1920s by doctors to help control their patients’ seizures, especially those affecting children with epilepsy. Ketogenic diet treatment consists of eating a very low-carb diet, consuming high amounts of fat in order to fuel the body, and reducing protein intake to only low to moderate amounts. About 65-80 percent of calories come from sources of fat and up to 20 percent from protein. The remaining from carbs (only about five-10 percent of daily calories).
Although it’s not entirely clear how the keto diet works for epilepsy, it leads to an increase in ketones in the blood. Increased ketones in the blood are associated with reduced seizure symptoms. During ketosis the body uses fat as an energy source, as glucose from carbohydrate foods is severely limited. This changes the way neurons in the brain seem to work and communicate, helping to control symptoms. (8)
The ketogenic diet is an option mostly for children with intractable epilepsy who use multiple antiepileptic drugs; however, some adults also find improvements by following this dietary approach. It’s been shown to be an effective treatment for seizures associated with glucose transporter protein deficiency syndrome and pyruvate dehydrogenase complex deficiency. There are some potential concerns regarding the diet, including initial side effects due to low carb dieting like fatigue and weakness, strictness and limitations in terms of meal preparation, and “unpalatability” of certain ketogenic foods. Side effects of the ketogenic diet tend to go away within a few weeks. But, it can be an unpleasant transition for some.
People with epilepsy who wish to use this as a primary or complimentary treatment approach can test if they are “in ketosis” (the state of burning fat for fuel) using strips at home and performing a urine test. Patients might also want to work with a dietician for help. This is especially true in the beginning stages during the transition to this way of eating.
3. Vagus Nerve Stimulation
The vagus nerve is the longest cranial nerve that passes through the neck and thorax to the torso/abdomen. It contains fibers that send signals around the body that regulate motor and sensory information. (9)
Vagus nerve stimulation therapy involves implanting a nerve stimulator that is about the size of a silver dollar coin into the patient’s chest. The stimulator connects to the nerve and controls electrical energy flowing to and from the brain. The device is sometimes referred to as a “pacemaker for the brain.” When a patient with epilepsy experiences signs and symptoms that a seizure may be beginning (“auras”) they can activate the stimulator with a magnet that can help prevent the seizure. (10) Researchers have found that this type of therapy doesn’t work for every patient, and medication often still need medication. But, it can still help reduce seizures on average by about 20 to 40 percent.
4. Emergency Care & Preventing Complications
It can be very scary to be with someone who is experiencing a seizure, especially the first time it happens. Experts recommend you take certain steps to reduce falls or other accidents. This way you help keep the person having the seizure as safe as possible:
What To Do If Someone Has A Seizure:
- Call an ambulance or seek medical help.
- Roll the person onto one side and try to place something under their head for padding. If they are wearing anything tight near their neck, loosen their clothing.
- Allow the person to move or shake if they appear to be doing so (don’t try to restrain or hold them).
- Check if they are wearing a bracelet that indicates the condition they are suffering from. Or, look in their wallet for related information (some people with severe epilepsy wear a bracelet to help identify themselves and warn of any allergies or complications)
Precautions Regarding Epilepsy
The first time that a seizure takes place it’s very important to visit a doctor for evaluation and a possible diagnosis. If your doctor diagnoses you with epilepsy, you likely won’t need medical help every time a minor seizure occurs. Even if you’ve been dealing with epilepsy for a while, always seek help from your doctor if you notice any of the following signs and symptoms for the first time:
- Seizure that lasts more than five minutes
- Slow recovery from a seizure
- A second seizure closely following an earlier one
- A seizure during pregnancy, an illness or following a new injury
- Changes in seizure duration and intensity after changing medications
Final Thoughts
- Seizures and epilepsy are often thought to be the same thing. A seizure is actually a single disruption of normal electrical communication signals between neurons in the brain. Epilepsy is the chronic disease that causes seizures.
- Symptoms of epilepsy include changes in perceptions, sensations, moods, emotion regulation, motor control and sometimes other complications due to falls, injury or accidents.
- Prevention and treatments for epilepsy include limiting “triggers” like high amounts of stress or anxiety, over-stimulation and lack of sleep; following a ketogenic diet; vagus nerve stimulation; use of anti-seizure medications and in certain cases, brain surgery to control seizures from spreading.
