This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Dysphagia Causes and Symptoms + 6 Natural Treatments
February 14, 2017

Swallowing is a very complex process. Some people lose their ability to swallow. Dysphagia, or difficulty swallowing, is fairly common among aging adults. It can lead to malnutrition, dehydration, aspiration pneumonia and even death. In the United States, dysphagia affects 300,000 to 600,000 people yearly. Age-related changes in swallowing physiology, as well as age-related diseases, are factors that can lead to the development of dysphagia in the elderly. (1)
There are several natural treatment methods for dysphasia, ranging from postural adjustments, to dietary changes and oral-motor exercises. If you are suffering from dysphagia, it’s smart to know your treatment options. Then you can work with a speech pathologist to decide which ones are right for you.
What Is Dysphagia?
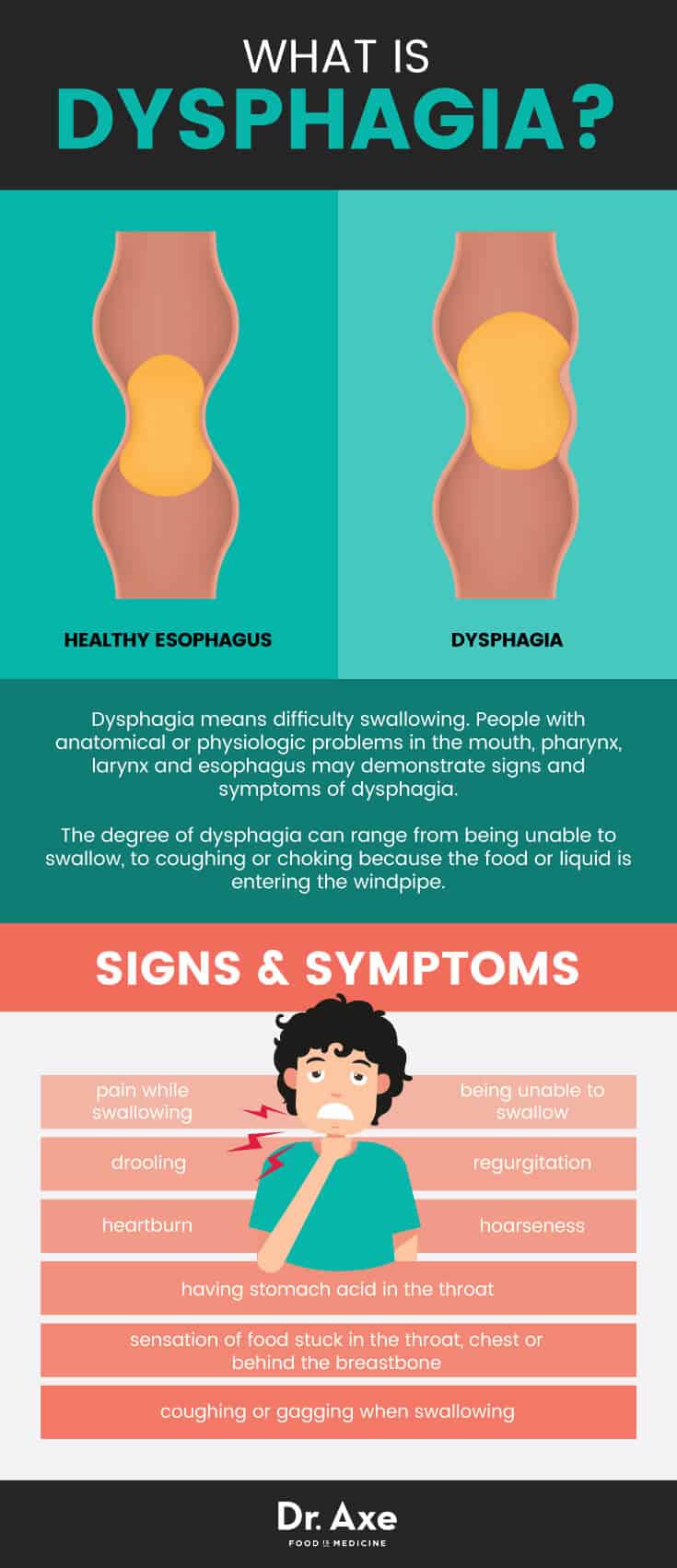
Dysphagia means it’s difficult to swallow. People with anatomical or physiologic problems in the mouth, pharynx, larynx and esophagus may show signs and symptoms of dysphagia. In addition, dysphagia contributes to many negative health status changes, including an increased risk of malnutrition and pneumonia.
When you swallow, food or liquid moves from the mouth, down the back of the throat, through the esophagus and into the stomach. People with dysphagia have trouble with any stage of this normal swallowing process.
The degree of dysphagia can range from being unable to swallow, to coughing or choking because the food or liquid is entering the windpipe. If you can’t swallow your saliva, food may get stuck in your throat or you may drool. (2)
Signs and symptoms associated with dysphagia may include:
- pain while swallowing
- being unable to swallow
- regurgitation
- sensation of food stuck in the throat, chest or behind the breastbone
- drooling
- hoarseness
- heartburn
- having stomach acid in the throat
- coughing or gagging when swallowing
Dysphagia is associated with nutritional deficits, especially following a stroke, and increased risk of pneumonia. Many patients regain their ability to swallow spontaneously within the first month following a stroke. However, some patients have difficulty swallowing beyond six months. Difficulties swallowing after a stroke may contribute to malnutrition due to limited food and liquid intake. This may lead the patient to have physical weakness or an altered level of consciousness. (3)
Post-stroke pneumonia is another common infection that affects up to one-third of acute stoke patients. It’s also the leading cause of mortality after stroke. Most stroke-related pneumonias are believed to result from dysphagia and the aspiration of food or liquid. Aspiration pneumonia is a lung infection that develops after you aspirate, or inhale, food or liquid, or when you vomit into your lungs. (4)
Dysphagia Causes and Risk Factors
It’s unclear how prevalent dysphagia is across different settings. But conservative estimates suggest that this condition affects 15 percent of the elderly population. According to the U.S. Census Bureau, in 2010 the population of persons with dysphagia above the age of 65 was 40 million. Dysphagia affects up to 68 percent of elderly nursing home residents, up to 30 percent of elderly admitted to the hospital, up to 64 percent of patients after stroke and 13 to 38 percent of elderly who live independently. (5)
Swallow physiology changes with age. Decrease in muscle mass and connective tissue elasticity results in loss of strength and range of motion. These age-related changes can negatively impact the smooth flow of swallowed materials through the upper aerodigestive tract. Beyond subtle motor changes, age-related decline in oral moisture, taste and smell sharpness may contribute to reduced swallowing ability in the elderly. (6)
While increasing age leads to subtle physiologic changes in a person’s ability to swallow, age-related diseases are major factors in the presence and severity of dysphagia. (7) Neurological conditions typically cause dysphagia. The most common cause is stroke and dementia. Other conditions that can cause swallowing difficulties include:
- Parkinson’s disease
- Traumatic brain injury
- Cerebral palsy
- ALS (Lou Gehrig’s disease)
- Multiple sclerosis
- Progressive supranuclear palsy
- Huntington’s disease
- Myasthenia gravis
Dysphagia is a common symptom in dementia. It’s estimated that up to 45 percent of patients institutionalized with dementia have some degree of swallowing difficulty. (8) Most commonly, patients with dementia exhibit a slowing of the swallowing process, which may increase the time it takes to finish a meal. This can increase the risk for poor nutritional status.
Other causes of dysphagia include a narrowed esophagus, an esophageal tumor, a blockage in the throat or esophagus, GERD, and dry mouth. Food allergies, scar tissue, spasms in the esophagus, pharyngeal diverticula (small pouch that forms in the throat), cancer and radiation therapy are also causes.
Medical Treatment for Dysphagia
Medications — Prescription oral medications or corticosteroids are sometimes used for dysphagia associated with GERD. Medications can also be used to relax the esophagus and reduce discomfort for dysphagia caused by esophageal spasms.
Surgery — Surgery may clear the esophageal path for cases of esophageal tumor, pharyngeal diverticula (pouches in the throat), or achalasia. (9)
Tube Feeding — If swallowing safely and smoothly does not become possible, or if the swallow function does not support nutrition or hydration enough, tube feeding may be needed.
Esophageal Dilation — Esophageal dilation is for people with a tight esophageal sphincter. Your doctor may use an endoscope with a special balloon attached to gently stretch and expand the width of your esophagus or pass a flexible tube or tubes to stretch the esophagus. (10)

6 Natural Treatments for Dysphagia
Treatment for dysphagia depends on the cause of the swallowing disorder. Treatment is not one size fits all. Speech-language pathologists play a central role in the management of patients with dysphagia. Speech pathologists may use a wide range of intervention strategies, including compensatory techniques and rehabilitation techniques. These strategies can include short-term adjustments to the patient, food and liquid changes, or environmental changes. The goal is to maintain nutrition and hydration needs until the patient can do so by herself.
1. Postural Adjustments
Postural adjustments are changes in body and head posture that may be recommended to reduce aspiration or residue. Changes in posture may alter the speed and direction of a food or liquid, and protect the airway to help the patient swallow safely. Studies show that one postural adjustment doesn’t work for all patients.
In general, postural adjustments are intended to be short-term treatments that are used to reduce the chances of aspiration. Specific postures include head tilt, head rotation, chin tuck, side lying and head back. A speech pathologist works with her patient to decide what posture change would be best. (11)
2. Swallow Maneuvers
Swallow maneuvers address different physiologic swallowing problems. Examples of swallow maneuvers include supraglottic swallow (hold breath, swallow and then gently cough), super supraglottic swallow (hold breath, bear down, swallow and then gently cough), and effortful, or hard swallow (swallow harder). (12) A speech pathologist would recommend these techniques.
3. Thickened Liquids
Hospitals and long-term care facilities frequently use thickened liquids as an intervention. They have an effect in helping to control the speed, direction, duration and clearance of chewed food. There’s varying results in studies done to find what thickened liquid works best.
For example, a study published in the Journal of Speech, Language, and Hearing Research sought to identify which of three treatments for aspiration was most successful for patients with dementia or Parkinson’s disease. The results showed that immediate elimination of aspiration on thin liquids occurred most often with honey-thickened liquids, followed by nectar-thickened liquids and then chin-down posture, but patient preference was best for chin-down posture followed closely by nectar-thickened liquids. (13)
In general, the thicker the viscosity, the slower the liquid moves, which makes it easier to swallow. Typically the least viscous liquid is used for mild dysphagia. Increasingly thicker liquids are used to manage more severe forms of the condition. Research shows thickened liquids can risk of dehydration. Thickened liquids make patients feel full and they are flavorless, which gives patients little motivation to drink. (14)
4. Exercises for the Tongue, Lips and Jaw
These oral-motor exercises are designed to increase range of movement. This helps with speech and swallow functioning. The treatments include stimulation to, or actions of, the lips, jaw, tongue, soft palate, pharynx, larynx and respiratory muscles. Oral-motor treatments range from passive to the more active, depending on the patient’s condition. Range of motion exercises assist with structural or tissue damage. Resistance exercises strengthen the muscles. Resistance exercises involve pushing against a spoon or tongue depressor to create resistance. Falsetto exercises are used to increase tongue base retraction. (15)
5. Diet Modifications
Dietary modification is a key part of dysphagia management. Modifying the texture of food may make it safer to swallow. This may include changing the thickness of liquids, chopping or pureeing solid foods. Eating smaller, more frequent meals can be helpful as well. Changing the taste and temperature of food can also make it easier to swallow and more enticing to eat.
Sometimes specific volumes of food per swallow may help patients to stimulate a swallow response — this is considered a feeding strategy. When dealing with diet modifications, speech pathologists or nurses often consult with a dietician to ensure that the patient is meeting her nutritional needs. (16)
6. Acupuncture
Although more research is needed, studies suggest that acupuncture can help people who have difficulty swallowing due to a stroke. This is especially true when acupuncture is used together with conventional stroke rehabilitation. (17)
One trial involving 66 patients suggests that there is a therapeutic effect of acupuncture for dysphagia after acute stroke. In the acupuncture group, 12 out of 34 participants recovered to normal feeding (35 percent), and in the control group, 7 out of 32 patients recovered to normal feeding (22 percent). Although this isn’t statistically significant, it does indicate that acupuncture was helpful for some stroke patients. (18)
Precautions
It is important to see your doctor if you are having difficulty swallowing or if you’re unable to swallow. If you aren’t able to breath because of food obstruction, get emergency help immediately.
To seek medical attention for dysphagia, you may want to see the following specialists:
- Otolaryngologist — treats problems in the ear, nose and throat
- Gastroenterologist — treats problems of the digestive system
- Neurologist — treats problems of the brain, spinal cord and nervous system
- Speech-Language Pathologist — evaluates and treats swallowing problems
Final Thoughts
- Dysphagia means difficulty swallowing. People with anatomical or physiologic deficits in the mouth, pharynx, larynx and esophagus may demonstrate signs and symptoms of dysphagia.
- Symptoms of dysphagia include pain while swallowing, inability to swallow, regurgitation, feeling like food is stuck in the throat, coughing and gagging.
- A number of factors can cause Dysphagia. Some include neurological conditions, physiological changes in a person’s ability to swallow, dementia, dry mouth, GERD, narrowed esophagus, cancer and radiation therapy.
- Treatment for dysphagia depends on the cause of the swallowing disorder. Treatment is not one size fits all. Speech-language pathologists play a central role in the behavioral management and treatment of patients with dysphagia.
- Some treatment techniques for dysphagia include postural adjustments, swallow maneuvers, thickened liquids, oral-motor exercises, diet modifications and acupuncture. For people who are unable to swallow, if these forms of therapy aren’t helping, a feeding tube may become necessary.








