This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Restless Leg Syndrome Symptoms, Causes & Treatments
August 22, 2016

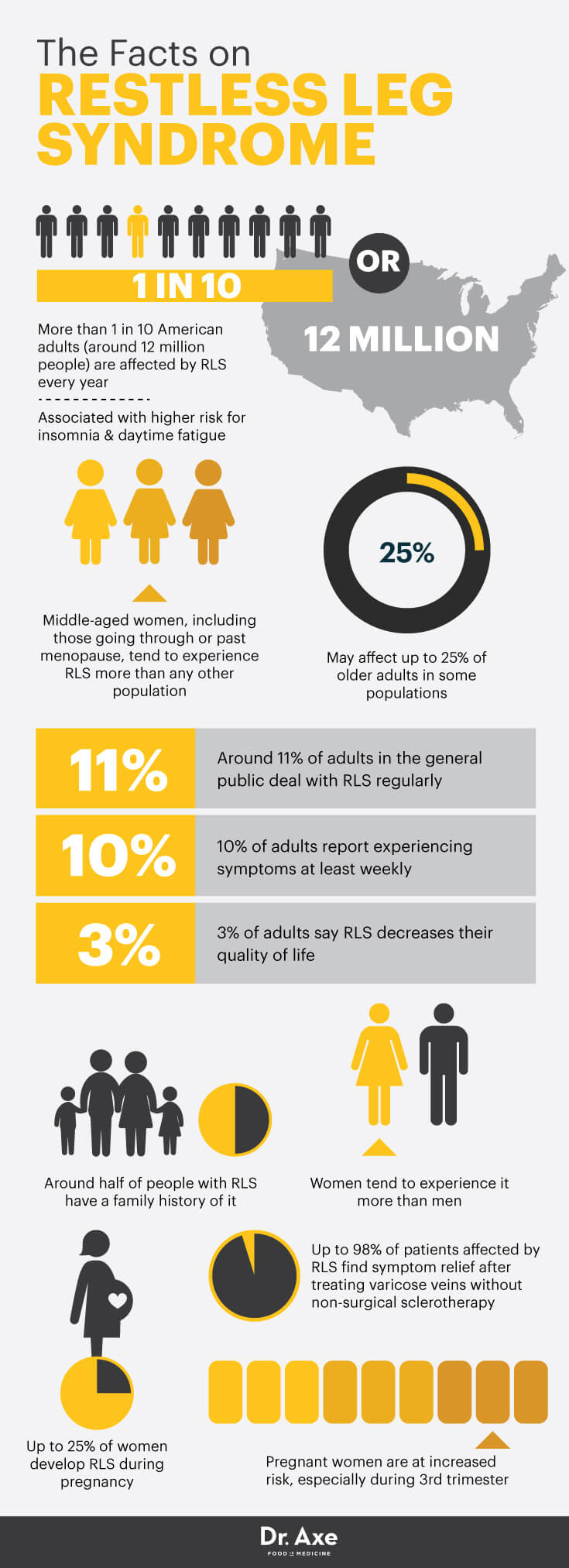
It’s estimated that restless leg syndrome (RLS) affects more than one in 10 American adults every year (around 12 million people). (1) RLS is a condition characterized by uncomfortable feelings in your legs, giving you a strong urge to move them in order to find relief. Because symptoms tend to get worse overnight, RLS is associated with a higher risk for insomnia and daytime fatigue, plus increased use of sleep-aid medications, alcohol and caffeine.
Middle-aged women, including those going through or past menopause, tend to experience RLS more than any other population. Most people describe the symptoms of restless leg syndrome — which can include experiencing jittery sensations, tingling, burning and aching in one or both legs — as more annoying than actually painful. Some people equate the sensations associated with RLS as “the feeling of bugs crawling up your leg.” In other words, although it’s not very dangerous long term, RLS causes some downright unpleasant side effects.
The desire to quickly get RLS sensations to stop makes people twitch, jiggle or move their legs throughout the night, leading to poor sleep. The worst part is that moving the legs usually doesn’t help RLS symptoms stay away for long — they usually return pretty quickly, and the cycle continues.
What causes RLS, and what can you do about it? Experts believe that RLS tends to run in families, is tied to poor diet and increased stress, and is likely made worse by a lifestyle that raises inflammation and the risk for nutrient deficiencies. The good news is that restless leg syndrome isn’t likely to cause long-term problems, although dealing with it can still be very tough. Natural ways to treat restless leg syndrome include improving your diet, exercising, stretching and setting up a nightly routine to relax before bedtime.
What Is Restless Leg Syndrome?
Restless legs syndrome is defined as a common neurological sensorimotor disorder characterized by an urge to move the legs during periods of rest or inactivity. The International Restless Legs Syndrome Study Group considers there to be four mandatory clinical features to establish a diagnosis of RLS: (2)
- The urge to move the legs, usually due to uncomfortable and unpleasant sensations in the legs
- Symptoms that begin or worsen during periods of rest or inactivity (including when sleeping, lying or sitting)
- Symptoms that are partially or totally relieved by movement
- Symptoms that become worse in the evening or nighttime
According to a report published in the Journal of Clinical Sleep Medicine, RLS is believed to be highly under-diagnosed, and some research shows it might affect up to 25 percent of all older adults in some populations. In the general public, around 11 percent of adults deal with RLS regularly, 10 percent report experiencing at least weekly symptoms and 3 percent say RLS greatly decreases their quality of life. (3)
What Causes Restless Leg Syndrome?
Who gets restless leg syndrome, and what are the common risk factors? Although children or teens can sometimes develop restless leg syndrome during development, puberty or growth spurts, it’s most common in middle-aged to older adults. Common factors contributing to RLS development include:
- Genetics: It’s believed that RLS runs in families, and some studies have found that around half of people with the condition have family histories of RLS.
- Gender: Women tend to experience RLS more than men, which experts believe is due to hormonal influences.
- Anemia or iron deficiency: RLS is also very common in patients undergoing dialysis for end-stage renal disease.
- Other nutrient deficiencies including magnesium deficiency or folate deficiency.
- Varicose veins: It’s now believed that varicose veins in the legs, unhealthy veins with valves that fail or leak blood backward into the legs, can cause RLS symptoms for many patients. The National Sleep Foundation reports that certain studies have found up to 98 percent of patients affected by RLS find some symptom relief after treating varicose veins in their legs with non-surgical sclerotherapy. (4)
- Chronic medical conditions affecting the kidneys or lungs: This can include obstructive lung disease or kidney disorders that cause electrolyte imbalances.
- Pregnancy: Studies show that pregnant woman are at an increased risk of having RLS, especially during their third trimesters, although it usually goes away shortly after delivery. Up to 25 percent of women develop RLS during pregnancy.
- Use of medications containing estrogen: This includes birth control pills or hormone replacement therapy used to manage menopause symptoms.
- Autoimmune disorders or diabetes: These can contribute to kidney problems, malnutrition, anemia, neurological problems or nerve damage. Among diabetics, it’s common to develop symptoms of neurology (nerve damage) that can lead to RLS.
- ADHD: Attention deficit hyperactivity disorder (ADHD) has been found to be common in children and adults with RLS.
- Cognitive disorders, including Parkinson’s disease.
Signs and Symptoms of Restless Leg Syndrome
Symptoms of restless leg syndrome tend to get worse during the night when someone is sleeping, but they can also occur during the daytime when the person is awake. Sitting for long periods, laying down or staying in one sedentary position usually makes symptoms worse.
The most common restless leg syndrome symptoms include:
- Sensations in the legs that are described as creeping, crawling, jittery, burning or aching. Most of the time, sensations are felt deep inside the calf muscles or in the feet, thighs and even arms.
- A strong urge or feeling that you need to immediately scratch, move, jiggle or stretch the legs in order to make sensations stop.
- Temporary relief from symptoms when you move the legs (although this usually only lasts briefly).
- Involuntary leg twitches and jerks, similar to having a cramp (called periodic limb movements). Leg twitches caused by night cramps are among the most commonly reported periodic limb movements due to RLS.
- Getting poor sleep due to feeling uncomfortable and waking up often. For many people, RLS symptoms start soon after they fall asleep and persistent intermittently throughout the night, resulting in interrupted sleep, insomnia, and daytime drowsiness or fatigue.
One of the biggest problems associated with RLS is that it disturbs normal sleep and can lead to many complications associated with chronic fatigue and under-sleeping. It also causes many people to turn to prescription sleep-aid or pain-reducing medications, which pose a high risk for addiction, dependency and side effects.
Conventional Treatment for Restless Leg Syndrome
If you suspect you might have RLS, visit your doctor to talk about your symptoms, risk factors and medical history. Your doctor will likely want to rule out other health problems, discuss your sleep habits, use of medications, and perform tests to check if you might be anemic, diabetic, or suffering from any nutrient deficiencies that can affect the nerves and muscles.
Today, the most commonly used medications to help control RLS include:
- Dopaminergics to help control the amount of movement in the legs. These include the drugs pramipexole, ropinirole, carbidopa or levodopa.
- Sleep medications, including benzodiazepines, to help people fall and stay asleep (although these haven’t been shown to fully work for many people and can cause various side effects).
- In some cases, strong painkillers to reduce wakefulness and act like a tranquilizer, such as codeine.
- Medications to help control nerve damaged caused by diabetes.
- Medications used to control side effects of epilepsy or cognitive disorders, such as Parkinson’s.
The National Institute of Neurological Disorders and Stroke states that medications are usually helpful for a period of time, but no single medication effectively manages RLS for all individuals. In addition, medications taken regularly may lose their effect over time, making it necessary to change medications periodically, and they can become addictive. (5)
Keep in in mind that the Restless Leg Syndrome Foundation reports that certain medications used to control common health conditions can also contribute to symptoms of RLS or make them worse. These include: (6)
- Antihistamines (like Benadryl) found in many cold, allergy and over-the-counter sleep aids
- Drops used to treat high blood pressure
- Anti-dizziness, anti-nausea medications (including meclizine, Compazine, Phenergan and Reglan)
- Antidepressants (including Elavil, Prozac, Lexapro and Effexor)
- Psychiatric medications that are used to treat bipolar disorders, schizophrenia and other serious disorders (such a haloperidol and phenothiazines)
Natural Treatments for Restless Leg Syndrome
Treatment for restless leg syndrome should focus first and foremost on correcting any identified underlying problems that are causing the disorder, whether it’s diabetes, anemia or a treatable autoimmune disorder. For many people with moderate cases of RLS, lifestyle changes, such as improving their diets, managing stress and practicing nightly bedtime routines, can all help lower RLS symptoms dramatically.
1. A Healthy Diet to Rule Out Deficiencies and Normalize Blood Sugar Levels
Vitamin or mineral deficiencies have been linked to restless leg syndrome and disorders that contribute to its symptoms, including diabetes and anemia. Here are foods that can help ease RLS symptoms, plus those to avoid that might make it worse:
Best Foods for Restless Leg Syndrome:
- Be sure to consume plenty electrolytes from whole foods, including those high in magnesium, potassium and calcium, in order to avoid an electrolyte imbalance. Sources include leafy green veggies, avocado, beans, bananas, sweet potatoes, raw dairy products (such as cultured yogurt), nuts and seeds.
- Balance blood sugar levels by consuming only unprocessed, 100 percent whole grains. Good choices are ancient grains (in moderation), including rolled oats, quinoa, buckwheat, wild rice and amaranth.
- Protein sources are usually good sources of iron and B vitamins. Strong choices include grass-fed beef, pasture-raised poultry, wild-caught fish, beans and lentils.
- Healthy fats help balance blood sugar and can lower inflammation tied to RLS. Sources include coconut or olive oil, avocado, seeds, nuts, and wild seafood containing omega-3 fats.
Foods that Can Make Restless Leg Syndrome Worse:
- Added sugar or artificial sweeteners
- Caffeinated drinks and alcohol
- Trans fats or refined oils
- Processed carbohydrates and grains
Other dietary and supplemental changes that can help treat restless leg syndrome naturally include:
- Avoiding too much alcohol, which can interfere with sleep — also try reducing or eliminating caffeine
- Quitting smoking
- Taking magnesium supplements to help prevent magnesium deficiency (a very common problem among people who are very stressed or eating poor diets)
2. Rule Out Anemia and Consume Enough Iron
If an underlying vitamin deficiency, including iron deficiency, is found to be the root cause of RLS or making it worse, supplementing and improving your diet can help. Consume plenty of foods high in iron, along with those high in B vitamins including folate. Foods high in iron include organ meats like liver, beans and lentils, spinach and leafy greens, sardines, grass-fed beef, and lamb.
Also consider taking a multivitamin that includes iron and B vitamins. However, it’s important not to take very high doses without being monitored, since taking high amounts of one nutrient can disturb your body’s ability to use other minerals. If symptoms become worse or others start to appear, talk to your doctor to talk about being monitored.
3. Warm Baths with Epsom Salts
Epsom salt can pretty much be found at any drugstore, is very affordable, and acts like a natural anti-inflammatory and muscle soother when added to a soothing, warm bath. Epsom salt has a long history of use in treating muscle spasms, pain and even magnesium deficiency because of its chemical formula (containing magnesium sulfate, MgSO4), which is broken down into magnesium, sulfur and oxygen.
The most common recommendation is to soak the entire body in warm water containing one to two cups of Epsom salt for at least 20 minutes. A half-cup of Epsom salt can also be added to a large pan of warm water for a 20-minute lower leg and foot bath. Not only does the salt help soothe the legs, but heat itself also relaxes muscles and has positive effects on RLS pain or tingling.
4. Essential Oils and Massage Therapy
You can either visit a massage therapist for a professional massage or perform simple massage maneuvers to your own legs at home to soothe uncomfortable or painful areas. When at home, consider applying essential oils to affected areas of the legs, trunks or arms, including cypress essential oil, rosemary, lavender or cedarwood oils. Many essential oils have natural antispasmodic qualities, which help inhibit problems associated with spasms, cramps and muscle pulls. They can also help you relax before bed and get better sleep.
5. Exercise and Stretching
Studies show there are certain exercises that can help alleviate restless leg syndrome symptoms and that being more physically active in general is helpful for reducing symptoms. One 2006 study found that a combination of moderate aerobic exercise and lower-body resistance training performed at least three times a week helped significantly lower RLS symptom severity. Many patients experienced around a 50 percent reduction in symptoms over the course of six weeks. (7)
One thing to point out, however, is that vigorous, very strenuous exercise and not allowing yourself enough rest between workouts might worsen symptoms, so be careful to take breaks and avoid overtraining.
Stretches you can perform to help reduce RLS symptoms include: (8)
- Calf stretches, such as lunging
- Forward bending to stretch hamstrings
- Quad stretches performed by standing on one leg, folding the other leg and pulling it behind you
- Hip stretches done by sitting on the ground with the legs bent and open like a book
- Stretching the heel against a flat wall by bending the toes and foot back toward you
- Getting up and moving legs after you’ve been sitting for a long time
6. Prioritizing Sleep and Managing Stress
RLS is tied to an increased risk for insomnia, sleep problems, chronic stress and fatigue. Be sure to work on establishing a nightly bedtime routine to help you relax and stay asleep more easily. Tips for getting better sleep and unwinding at night include stress relievers, such as:
- Avoiding electronics within several hours of bedtime
- Exercising during the day to feel more sleepy at night (including yoga, resistance training or walking, which have all been found to be helpful)
- Stretching and doing yoga
- Taking hot baths or showers
- Massaging your legs
- Deep breathing and body relaxation techniques
- Meditation and prayer
- Writing in a journal
- Reading something soothing
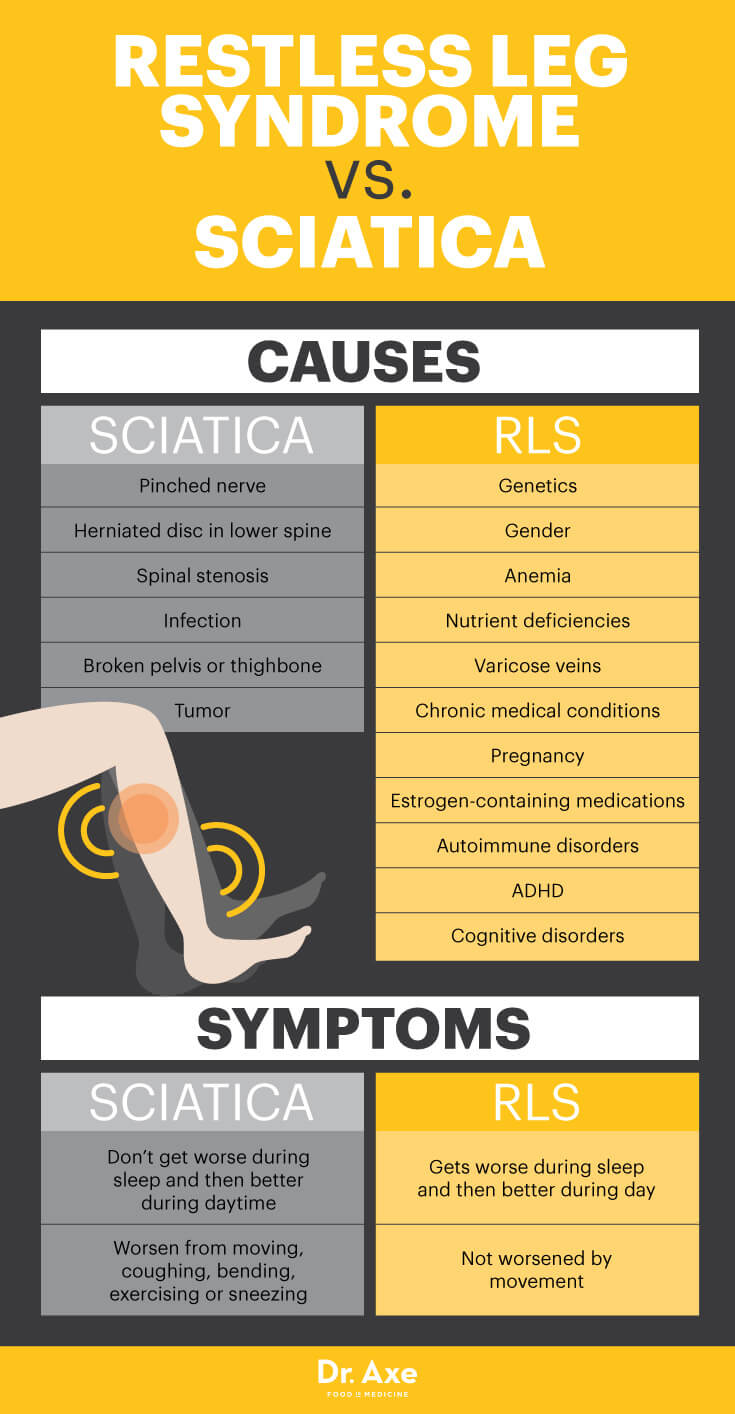
Restless Leg Syndrome vs. Sciatica
- Sciatica, also called sciatic nerve pain, causes pain running down the legs, usually from the lower back all the way to the feet. RLS and sciatic nerve pain are often confused.
- The primary cause of sciatica is a pinched nerve or herniated disc in the lower spine running along the sciatic nerve. Other causes of sciatica are spinal stenosis, infection, a broken pelvis or thighbone, or a tumor.
- According to Harvard Medical School, the biggest difference between these two conditions is that sciatica doesn’t tend to get worse during sleep and then better again during the daytime, like restless leg syndrome usually does. Sciatica symptoms are also usually worsened from moving, coughing, bending, exercising, sneezing and physical activities that tug on the sciatic nerve. (9)
- Some choose pain-reducing medications or even surgery to correct sciatic, but less invasive treatment options can also be very helpful. Treatments for sciatica include chiropractic spinal adjustments or spinal manipulation, stretching, acupuncture, yoga, and massage therapy.
Precautions Regarding Restless Leg Syndrome
For some people, RLS gets worse with age, especially if underlying causes aren’t treated. Most of the time restless legs syndrome won’t lead to a more serious health problem or pose any major risks, but it’s still important to keep an eye on progress of symptoms.
To rule out other health problems and start correcting underlying disorders that cause leg pain, talk to a doctor if you also experience any of the following symptoms, in addition to those associated with RLS:
- Dizziness and signs of low blood sugar
- Fainting
- Forgetfulness and memory loss
- Chronic fatigue that’s severe
- Numbness and tingling in your limbs that’s severe
Final Thoughts
- Restless leg syndrome causes uncomfortable sensations in the legs that interrupt sleep and create an urge to keep moving the legs.
- Causes include anemia, diabetes and diabetic neuropathy, genetics, a sedentary lifestyle, and other medical conditions that cause nerve damage.
- Changing your diet, lifestyle and nighttime behaviors can often help you sleep if you have restless legs syndrome.
- Establish a nightly routine to help you sleep, correct any deficiencies, and stretch or massage the legs often. Consume more foods with magnesium, iron and B vitamins, and reduce caffeine, sugar and alcohol intake to help relieve RLS.




