This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Myasthenia Gravis & Symptom Management
January 1, 2018

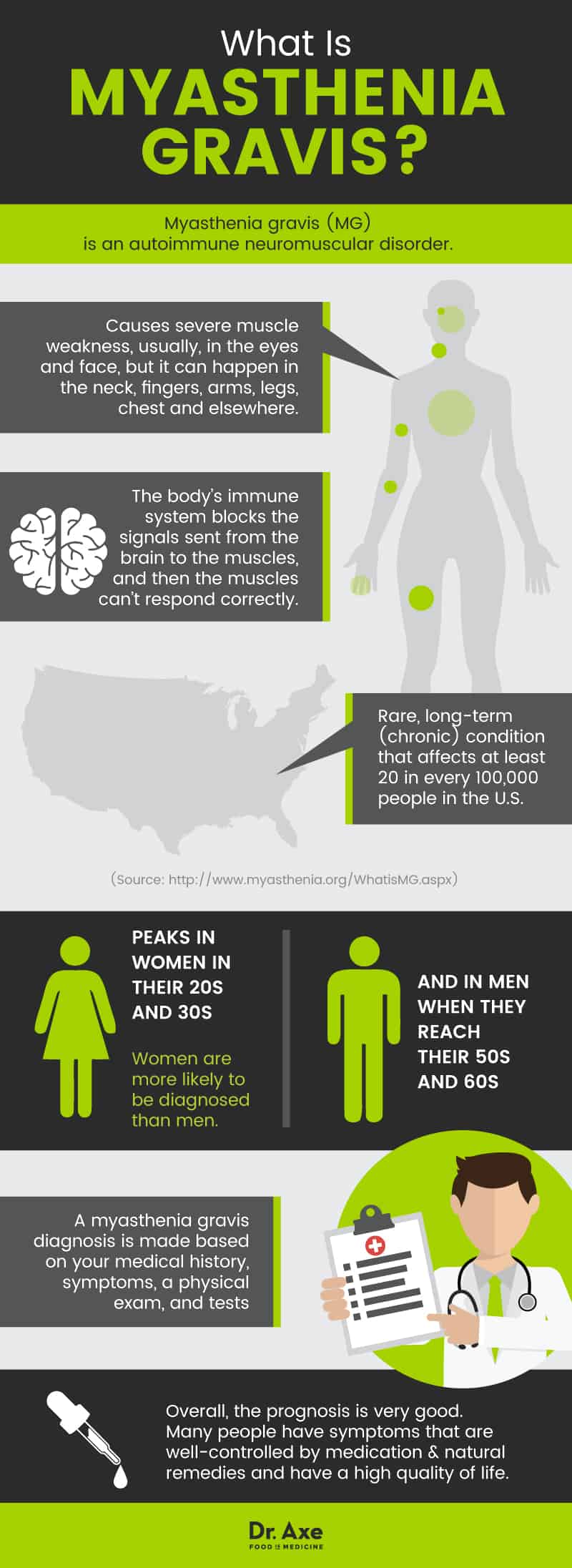
Myasthenia gravis is an autoimmune disorder. It causes severe muscle weakness. Usually, the weakness occurs in the eyes and face, but it can happen in the neck, fingers, arms, legs, chest and elsewhere. The weakness gets worse after activity and better after rest. Although it can be serious, most people with myasthenia gravis have a good quality of life, respond well to treatments and have a normal life expectancy. (1)
What Is Myasthenia Gravis?
Myasthenia gravis, sometimes just referred to as MG, is an autoimmune neuromuscular disorder. The body’s immune system blocks the signals sent from the brain to the muscles, and then the muscles can’t respond correctly. (1) It is a rare, long-term (chronic) condition that affects at least 20 in every 100,000 people worldwide. (2) It peaks in women in their 20s and 30s and in men when they reach their 50s and 60s, and women are more likely to be diagnosed than men. (3)
Myasthenia gravis results in weakness of skeletal muscles — the muscles the body uses to move. It typically gets better after rest and worse after activity. Although it most often affects the eyes (called ocular myasthenia when it doesn’t affect other muscles as well), it can affect the face, neck, speech, throat, arms and legs. In about 10 percent of people with myasthenia gravis, the condition affects the muscles that help them breathe, forcing them to use a ventilator for help breathing. (2) When this happens, it is called a myasthenic crisis.
What is the prognosis for people with myasthenia gravis?
There is no known cure for myasthenia gravis, but there are many treatments that help most people with the disorder manage symptoms fairly well. In general, symptoms get worse, particularly for the first three years after diagnosis. (4) However, most people have an improvement in symptoms with treatment.
In some people (up to 1 in 5), the disorder goes away entirely for a time. (4) This is called remission. In many cases of remission, the disorder goes away for about five years and in others, it may never return. In still other cases, myasthenia gravis may get better to the point that medication is no longer needed. (1)
Overall, the prognosis is very good. Many people have symptoms that are well-controlled by medication and natural remedies and have a high quality of life.
How do you know if you have myasthenia gravis?
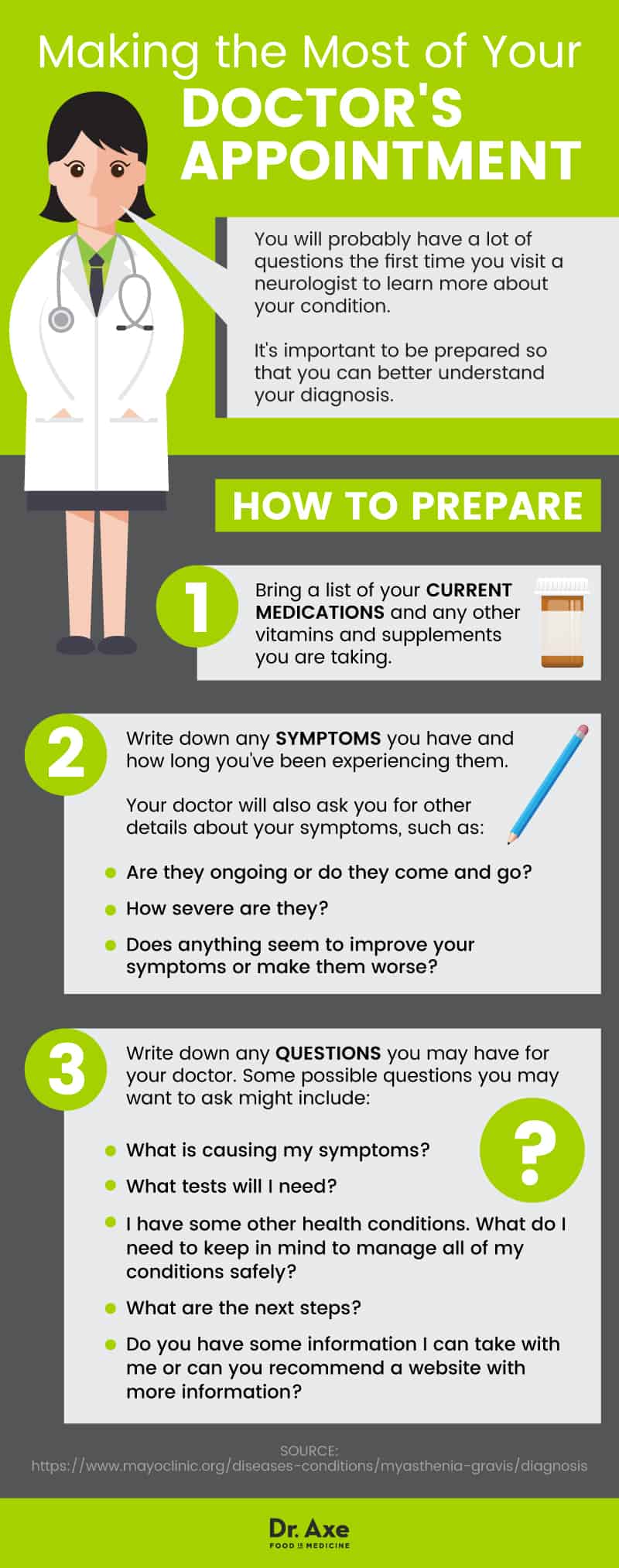
A trained medical professional should diagnose you. Do not attempt to diagnose yourself based on your symptoms, since other problems may share the signs and symptoms of myasthenia gravis (such as Bell’s palsy). (3)
A myasthenia gravis diagnosis is made based on your medical history, symptoms, a physical exam, and tests such as: (5)
- Neurological examinations to check your muscles, reflexes, balance, coordination and strength
- Eye exams to check you for double vision and other sight concerns
- Edrophonium injection test
- For this test, a chemical called edrophonium chloride is injected. If it improves your muscle strength, you may have myasthenia gravis.
- An ice pack test, in which an ice pack is held on your eyelid for a few minutes to see if it improves droopiness, may be done instead of the edrophonium injection.
- Blood tests to check for antibodies, or proteins made by your immune system that may block nerve signals to your muscles
- Repetitive nerve stimulation to check, over and over again, your nerves’ ability to signal your muscles to move and whether the signals get worse as you get tired
- Breathing tests to see how well you are able to breathe
- Imaging, such as a CT or MRI, to look for tumors or thymus problems
- Electroymography (EMG) to measure the electric communication between your brain and a single muscle fiber, using a fine wire inserted through your skin
Signs & Symptoms
In addition to muscle weakness that gets worse when you are active and better after rest, myasthenia gravis symptoms include: (6, 5)
- droopy eyelids
- double vision
- problems with talking (for example, not sounding like normal when you speak)
- trouble chewing or swallowing (also called dysphagia)
- inability to move face muscles (for example, trouble smiling)
- fatigue (feeling very tired, especially after activity)
- difficulty walking upstairs, lifting things, or doing repetitive motions
- trouble breathing
What symptoms would you expect with myasthenia gravis?
The symptoms affecting the eyes are often the first to occur. People who have only eye-related symptoms for the first three years are more likely to stay that way and not experience other symptoms. (4)
The neck and jaw are also often affected early. This impacts talking, chewing, swallowing and head control. When myasthenia gravis affects the head and neck, it can change how you sound when you talk (making you slur speech or sound nasally). You may also choke or gag more often or feel tired of chewing after a few minutes.
Many people with myasthenia gravis feel best in the morning after a good night’s sleep and weakest in the evening. (4) However, symptoms can change throughout the day and be different day to day.
Causes & Risk Factors
How does myasthenia gravis occur?
This disorder happens when there is an abnormal block put up by the body’s immune system. The body creates proteins called antibodies that attack receptors in muscles. When the receptors are blocked or disabled, the muscles can’t get signals sent by the nerves that tell them to contract. This means they can’t move as well, which results in the typical muscle weakness of people with the disorder. (3)
In more technical language, the nerves send something called acetylcholine to tell a muscle to move. People with myasthenia gravis have an immune system that mistakenly makes something to block acetylcholine from linking up with its receptors in the muscles. Fewer receptors end up getting the acetylcholine signal they need because of the blockers (called anti-acetylcholine receptor antibodies or anti-AChR), so the muscle response is weaker than it would be in someone without the disorder. Other antibodies also exist but their role in the disease is still being explored, and they result in the same eventual effect on muscle strength. (3)
While the overall cause of myasthenia gravis is an autoimmune problem, it is not known what triggers the immune system to start making antibodies that dull muscle response. However, many people with the disorder (up to 3 in every 4 people) also have a problem with the thymus. (3) The thymus gland is a tiny organ that works during childhood and puberty creating cells to fight off infections and keep our body from attacking itself. (7) As we age, the thymus shrinks and slowly turns to nothing more than fat. (8) But for many people with myasthenia gravis, there are too many cells in the thymus, such as cancerous or benign tumors. The thymus then doesn’t effectively stop the cells that make the antibodies that block muscle receptors. (3)
Myasthenia gravis causes may also include your genes. Although there is no known specific genetic cause, it is likely that people inherit certain genes that make them more likely to develop myasthenia gravis. Then when they are faced with some sort of environmental trigger, it may develop and cause symptoms. (3)
Myasthenia gravis risk factors
Certain characteristics may increase the chances of a diagnosis with this disorder. Risk factors include: (9, 10, 11)
- Having another autoimmune condition, particularly rheumatoid arthritis, thyroid disease or lupus
- Having a family member with myasthenia gravis
- Being stressed, ill or fatigued
- Taking certain medications
- These include beta blockers, quinidine gluconate or sulfate, quinine, phenytoin and certain antibiotics and anesthetics
- Having a problem with the thymus gland
The known risk factors are not very helpful in determining whether you are truly at risk, since the disorder is so rare and the risk factors may only make your chances of getting the disorder slightly higher. Myasthenia gravis can affect people of any ethnicity and any age. (12)
Conventional Treatment
Not everyone needs medical treatment for myasthenia gravis. However, when you have symptoms that interfere with daily life or that make you uncomfortable, you may wish to seek treatment. You should also get treatment if your condition affects your swallowing or breathing, since these can be dangerous symptoms.
Conventional myasthenia gravis treatment options include: (5, 13)
- Cholinesterase inhibitors, also called anticholinesterases. These drugs help boost the acetylcholine that your muscles can use. These may relieve symptoms very quickly after use (within minutes!), but may have some unpleasant side effects. Since they make other muscles contract more easily, too, you may experience diarrhea or have too much saliva in your mouth until your doctor finds the right dose for you. Most people with myasthenia gravis also need other drugs to help manage their symptoms, but some do well with just cholinesterase inhibitors.
- Corticosteroids or immunosuppressants. These drugs may keep your immune system from making antibodies against acetylcholine. If they work well, your muscle receptors will not be blocked and may be able to receive the nerve signals telling them to move. These drugs can have serious side effects and may require you to go in for regular blood tests or other health checks.
- Plasmapheresis. This process routes your blood through a machine that filters out the antibodies that block muscle receptors. Your own blood is then put right back into your body. The effects last a few weeks, until your body has made more antibodies to block the muscle from getting nerve signals again.
- Antibody therapy. There are two types of this therapy, which tries to change your immune system.
- Intravenous immunoglobulin (IVIg) therapy puts normal antibodies into your veins, temporarily stopping your immune system from making the blockers.
- Monoclonal antibody therapy puts medication such as rituximab into your veins. This drug works to lower the number of a certain type of white blood cell in your veins. Your immune system may then stop making as much of the muscle receptor blockers.
- Surgery. Many people with myasthenia gravis have a tumor or problem with their thymus gland. Even if they don’t, removal of the thymus may help relieve symptoms. In many cases, it may stop all symptoms, without drugs. Its effects may be permanent, but sometimes they don’t happen right away — they can take months or even years to help.
Talk with your health care provider about the best treatment options for you, since some therapies may be a better fit — and more likely to work — than others. The best options may depend on your age, health, other medicines you may take and more. There may also be clinical trials with new therapies that could be a good option for people who do not respond to other treatments. (14)
12 Natural Treatments
There are many natural ways people with myasthenia gravis can work to relieve their symptoms. In general, these are natural myasthenia gravis therapies you may wish to try:
- Ask about respiratory muscle training.
- Plan ahead.
- Eat small meals more often.
- Eat a diet that meets your myasthenia gravis-specific needs.
- Make your home safer.
- Avoid manual work when possible.
- Wear an eye patch.
- Get support.
- Take baths.
- Avoid possible triggers.
- Ask about traditional Chinese medicine.
- Talk to a chiropractor.
1. Ask about respiratory muscle training
Research shows that people who receive pulmonary (breathing) training develop better endurance and have less breathlessness. (15, 16) The training tries to improve the strength of muscles that help you breathe in and out so that your body doesn’t have to work as hard to move those muscles. The goal of this type of therapy is to keep you from having trouble breathing and, possibly, to lower your chances of myasthenic crisis. (17)
2. Plan ahead
You may feel too tired by the end of the day to do anything physically demanding. If you plan your day’s activities for times when you have the most energy (for example, just after waking up in the morning or after an afternoon nap), you may be better able to accomplish your daily tasks. (5)
3. Eat small meals more often
Many people with myasthenia gravis have difficulty chewing, especially when the food is tough like steak or pork. If your jaw tends to get tired, or if you ever have trouble swallowing, take extra care when you eat. (5) Think about eating small meals so that you do not get tired of chewing before you are done. You may need to eat more often to get the same number of calories, but by spreading out the stress on your jaw, you may avoid the annoyance of exhausting chewing and the danger of difficult swallowing. You can also eat foods that are easier to chew, such as soups, cooked vegetables, fish, stews, lentils, bananas, rice, oatmeal, etc.
4. Eat a diet that meets your myasthenia gravis-specific needs
People with myasthenia gravis may struggle with excess weight, bone loss, drug side effects such as nausea or diarrhea, low potassium levels and fluid retention. You can follow specific diet changes to address these symptoms, if you have any. For example: (18)
- Eat more vegetables, grains and lean proteins and watch your overall calorie intake if you are above a healthy weight.
- Ask your doctor about a calcium and vitamin D supplement. You may need at least 1,000 milligrams of calcium and up to 800 IU of vitamin D each day.
- Avoid fatty, spicy or high-fiber foods and dairy (except yogurt) if you have diarrhea or an upset stomach.
- Eat foods rich in potassium, such as avocados, bananas, potatoes and orange juice.
- Scale back on salt and high-sodium foods, such as frozen meals, canned goods, processed foods and salty snacks.
5. Make your home safer
Think about things that make your home more challenging for you when you are tired. Are they trip hazards? Slippery surfaces? Lots of stairs? “Weakness-proof” your house so that you are less likely to be injured when you are weak or tired. Things that may help support you and keep you safer include: (5)
- grab bars or railings in the shower or near stairs
- clean floors
- clear paths and sidewalks
- an automatic stair lift
6. Avoid manual work when possible
Many people with myasthenia gravis may need to make some adjustments in their work life. However, there are simple changes you can make at home and throughout your day to limit how much energy you spend on daily activities. (5) For example, use power tools such as electric toothbrushes, a countertop mixer, a leaf blower, or other items that save you physical effort. You can also make small changes, such as doing housework in small pieces every day rather than waiting for it to pile up. If you can afford it, consider paying someone for help cleaning your house or doing yard work, washing the car, or doing house projects.
7. Wear an eye patch
If you have double vision, you may be able to avoid it by wearing a patch. (5) Switch it between eyes throughout the day while you read, write or watch TV so that one eye doesn’t get over-strained.
8. Get support
Some people with myasthenia gravis have trouble coping with the disorder. (19) Its limits on activity can make you feel more isolated or depressed, or you may be mourning your loss of energy or former activities. By being open about any emotional stress, anxiety, or depression you have, you may be able to work with a health care provider or support group to improve your quality of life. You may also form friendships and get great advice by talking with others living with myasthenia gravis. The Myasthenia Gravis Foundation of America has a list of support groups and events. (20) There are also many online groups that offer chat rooms and email support.
9. Take baths
Baths can spare you the effort of a shower. You can avoid standing, lots of movement of your arms up overhead, bearing your full body weight, etc. Even better, early research shows that taking a long, hot bath may have benefits (similar to those from exercise!) for your metabolism and body inflammation. (21) Of course, if heat is a trigger for your symptoms, an hour in a hot tub is probably not a good therapy for you.
10. Avoid possible triggers
Some people with this condition find that there are specific triggers to myasthenic crisis or to worse day-to-day symptoms. Conquer MG offers a thorough list of possible triggers, but you should track your activities and symptoms to find out what helps or hurts you. Triggers may include: (22)
- lack of sleep
- stress
- illness
- anger
- pain
- depression
- extreme temperatures
- bright light
- hot foods and drinks
- alcohol
- quinine (tonic water)
- some chemicals
Some drugs are also believed to make myasthenia gravis symptoms worse. However, before you stop taking a drug because of its association with symptoms, talk with your doctor. It may be more important to your health to keep taking it despite its impact on your myasthenia gravis symptoms. (23)
11. Ask about traditional Chinese medicine (TCM)
Some formal research has found promising effects of TCM on myasthenia gravis symptoms. However, these are still under study and you should use caution. Be sure that your doctor and the TCM practitioner know everything you are taking, including supplements and herbs. This will help them understand possible interactions TCM may have with other drugs or supplements in your system. Early research shows possible positive impacts of Buzhongyiqi decoction, auricular acupuncture, electroacupuncture, and Yiqi Qushi recipe. (24, 25, 26, 27)
12. Talk to a chiropractor
Although not typically considered for myasthenia gravis, there is a published case report of a young child with myasthenia gravis who experienced total remission from the disorder after several months of chiropractic care. (28) This may have just been a coincidence, as myasthenia gravis in children is more likely to go away on its own than it is in adults. (29) However, if you have back pain and a chiropractor thinks you are a good candidate for spinal manipulation, you may find some relief.
Precautions
Myasthenic crisis can be deadly. If you notice a sudden or steady increase in how weak you feel, or if you have unusual weakness that is making it harder to talk or breathe, get medical help immediately.
Drug avoidance to prevent myasthenia gravis may be appropriate for some people. However, sometimes the health condition treated by the medication is more important to control than myasthenia gravis symptoms. Always talk with your doctor before changing your medication. If you are worried that one of your medicines is causing or worsening your symptoms, ask if there is an alternative.
Myasthenia gravis may make it less enjoyable or more challenging to eat a regular diet. This can lead to malnutrition unless you work hard to make sure you still get a good balance of healthy food and enough calories. (30) Talk with a health care professional or a nutritionist if you have so much trouble chewing or swallowing that you are losing weight. You may be able to go on a liquid or partially liquid diet to help get the nutrition you need until your symptoms improve.
Myasthenia Gravis Key Points
Myasthenia gravis can cause different symptoms in everyone. Some may have severe symptoms that cause difficulty talking or breathing, while others may just have occasionally droopy eyelids. Remember:
- Overall, the prognosis for people with myasthenia gravis is good. Many people have a normal life expectancy and relatively good quality of life.
- Most people’s symptoms improve with treatment. Some people even have long-term or permanent remission of the disorder.
- Your doctor will likely recommend cholinesterase inhibitor drugs, immunosuppressants, antibody therapy or surgery to remove your thymus as part of a conventional treatment plan. These can be very effective at stopping or reducing symptoms.
- Simple lifestyle changes can help you accommodate your condition and improve your quality of life.
12 Natural Tips to Help Manage Myasthenia Gravis
-
- Ask about respiratory muscle training.
- Plan ahead.
- Eat small meals more often.
- Eat a diet that meets your myasthenia gravis-specific needs.
- Make your home safer.
- Avoid manual work when possible.
- Wear an eye patch.
- Get support.
- Take baths.
- Avoid possible triggers.
- Ask about traditional Chinese medicine.
- Talk to a chiropractor.
