This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Diabetes Insipidus: Causes & Symptoms + 5 Natural Treatments
March 3, 2017
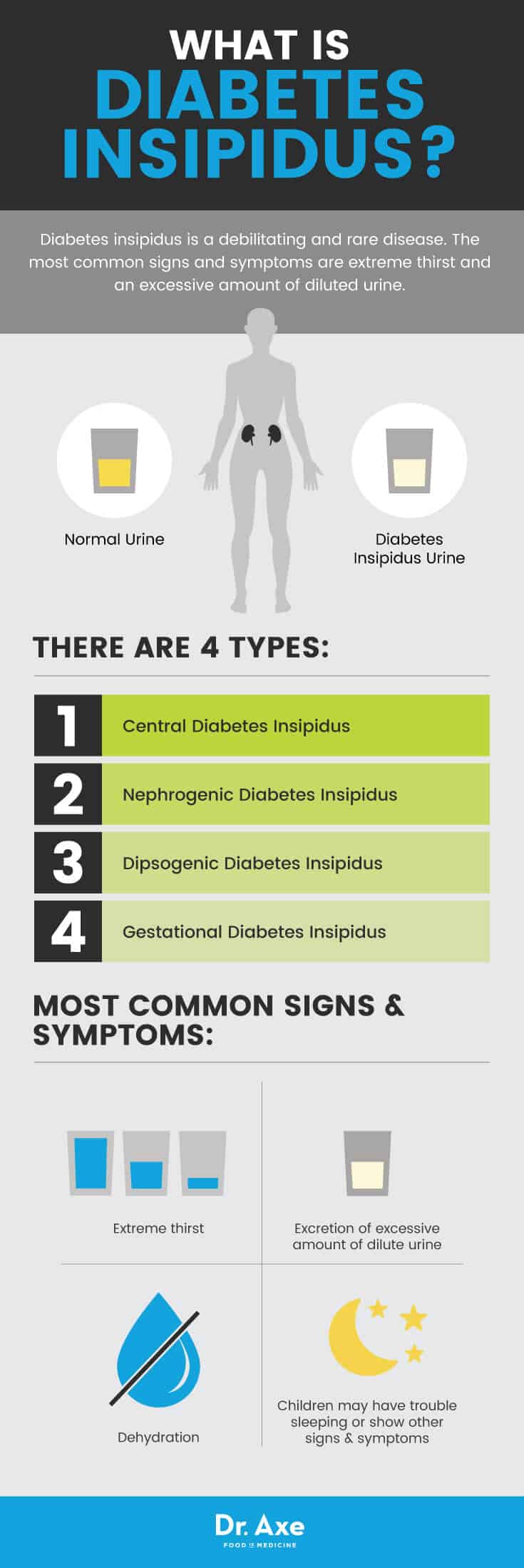
Diabetes insipidus, is a debilitating and rare disease, with a prevalence of 1 out of 25,000 people. Often referred to as “water diabetes,” it is a condition characterized by frequent and heavy urination, excessive thirst and an overall feeling of weakness. It’s caused by a defect in the pituitary gland or in the kidneys. (1)
The term insipidus means “without taste” in Latin, while diabetes mellitus involves the excretion of “sweet” urine. People with diabetes insipidus pass urine that is diluted, odorless and relatively low in sodium content.
Diabetes insipidus and diabetes mellitus (which includes both type 1 and type 2 diabetes) are unrelated. Both conditions do cause frequent urination and constant thirst. People with diabetes insipidus have normal blood sugar levels, but their kidneys cannot balance fluid in the body.
Although the symptoms of diabetes insipidus can be bothersome and sometimes even life-changing, the condition doesn’t increase future health risks when it is managed properly. It’s important to find the right treatment plan, which typically involves taking measures to avoid dehydration.
What is Diabetes Insipidus?
Diabetes insipidus is a condition that disrupts normal life due to increased thirst and passing of large volumes or urine, even at night. It is a part of a group of hereditary or acquired polyuria (when large amounts of urine is produced) and polydipsia (excessive thirst) diseases. It’s associated with inadequate vasopressin or antidiuretic hormone secretion.
Vasopressin, which includes arginine vasopressin (AVP) and antidiuretic hormone (ADH), is a peptide hormone formed in the hypothalamus. It then travels to the posterior pituitary where it releases into the blood. In order to fully understand the cause of diabetes insipidus, you must first learn about the role of vasopressin and how it affects your kidneys and fluid balance. (2)
Every day, your kidneys normally filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine. Urine is composed of wastes and extra fluid. Your urine then flows from your kidneys to the bladder and through tubes called ureters. Your body regulates fluid by balancing liquid and removing extra fluid. Thirst usually controls your liquid intake, while urination removes most fluid. People also lose fluid through sweating, breathing or diarrhea.
The hypothalamus (a small gland located at the base of the brain) produces vasopressin. Vasopressin is stored in the pituitary gland and released into the bloodstream when the body has a low fluid level. Vasopressin signals your kidneys to absorb less fluid from the bloodstream, resulting in less urine. But when the body has extra fluid, the pituitary gland releases smaller amounts of vasopressin, or even none at all. This causes the kidneys to remove more fluid from the bloodstream and produce more urine. (3)
These issues with the release of vasopressin lead to this rare disorder that occurs when the kidneys pass an abnormally large volume of urine that is insipid — dilute and odorless.
Causes and Risk Factors
There are four different types of diabetes insipidus — central, nephrogenic, dipsogenic and gestational. Each type of diabetes insipidus has a different cause.
Central Diabetes Insipidus
Central diabetes insipidus (or neurogenic diabetes insipidus) is the most common form of diabetes insipidus. It occurs in both males and females equally and at any age. Inadequate synthesis or release of vasopressin causes it, often due to surgery, head injury, an infection or a tumor that damages the hypothalamus or posterior pituitary gland. (4) The disruption of vasopressin causes the kidneys to remove too much fluid from the body, leading to an increase in urination.
Nephrogenic Diabetes Insipidus
Nephrogenic diabetes insipidus results from the failure of the kidneys to respond to vasopressin. This causes the kidneys to continue to remove too much fluid from a person’s bloodstream. Nephrogenic diabetes insipidus can result from inherited gene changes or mutations that prevent the kidneys from responding normally to vasopressin. (5) Chronic kidney disease, low potassium levels in the blood, high calcium levels in the blood, a blockage of the urinary tract and certain medications (like lithium) can cause nephrogenic diabetes insipidus. (6)
Dipsogenic Diabetes Insipidus
Dipsogenic diabetes insipidus (also known as primary polydipsia) is a defect in the thirst mechanism, located in the hypothalamus. This defect results in an abnormal increase in thirst and liquid intake that suppresses vasopressin section and increases urine output. Events or conditions that damage the hypothalamus or pituitary gland cause it, such as surgery, inflammation, a tumor or a head injury. Certain medications or mental health problems may predispose a person to this type of diabetes insipidus.
Gestational Diabetes Insipidus
Gestational diabetes insipidus can occur during pregnancy when an enzyme made by the placenta breaks down the mother’s vasopressin. Or, in some cases, a pregnant women produces more prostaglandin, which reduces chemical sensitivity to vasopressin. Symptoms of gestational diabetes insipidus often go unnoticed. The condition typically goes away after the mother delivers the baby. (7)
Diabetes insipidus can develop at any age and the prevalence is equal among males and females. Nephrogenic diabetes insipidus that’s present at or shortly after birth is usually genetic and tends to affect males. However, women can pass the gene on to their children.
Common Signs and Symptoms
The most common signs and symptoms of diabetes insipidus include extreme thirst and the excretion of an excessive amount of diluted urine. A person’s body regulates fluid by balancing liquid intake and removing extra fluid. Thirst usually controls a person’s rate of liquid intake, while urination removes most fluid.
Normally, a healthy adult will urinate an average of less than 3 liters a day. Depending on the severity of the disease, urine output can be as much as 15 liters a day when you’re drinking a lot of fluids. Because of this frequent urination, people with diabetes insipidus usually have to get up in middle of the night to urinate (called nocturia). They may even struggle with bedwetting.
Infants and young children with diabetes insipidus may have trouble sleeping, or show other signs and symptoms of disease. These can include: unexplained fussiness, inconsolable crying, fever, vomiting, diarrhea, constipation, excessively wet diapers, weight loss and delayed growth. (8)
The main complication of diabetes insipidus is dehydration, which occurs when fluid loss is greater than liquid intake. Signs of dehydration include: thirst, dry skin, sluggishness, fatigue, dizziness, confusion and nausea. If you are severely dehydrated, you can even experience seizures, permanent brain damage and death.
Another common complication is an electrolyte imbalance. Electrolytes are certain nutrients or chemicals (such as sodium and potassium) present in your body that have many important functions, from regulating your heartbeat to allowing your muscles to contract so you can move. Electrolytes are found within bodily fluids, including urine, blood and sweat. When you have an imbalance, you may experience muscle aches, spasms or twitches, anxiety, frequent headaches, feeling very thirsty, fever, joint pain, confusion, digestive issues, irregular heartbeats, fatigue and changes in appetite or body weight.
Conventional Treatment
The primary treatment for diabetes insipidus involves drinking enough liquid to prevent dehydration. Depending on what type of diabetes insipidus you have, treatment for constant thirst and frequent urination will vary.
Since its introduction in 1972, desmopressin has been the most widely used drug for the treatment of diabetes insipidus. Desmopressin is a synthetic, man-made hormone that comes as an injection, nasal spray or pill. It works by replacing the vasopressin that a patient’s body would normally produce, which can control the amount of urine your kidneys make. Desmopressin helps a patient to manage her symptoms, but it does not cure the disease. (9)
Desmopressin can cause a low level of sodium in the blood. This is rare, but can be serious and possibly life-threatening. Drinking too much water or other fluids increases your risk of having low sodium levels in your blood. It’s important to follow your doctor’s directions if you are using this drug and limit your fluids as instructed. Signs of low levels of sodium in the blood include: loss of appetite, severe nausea, vomiting, severe headache, mental and mood chances, muscle weakness, cramps and spasms, shallow breathing and loss of consciousness.
Health care providers commonly prescribe diuretics to help patients’ kidneys remove fluid from the body. On the the other hand, there’s a class of diuretics called thiazides that help to reduce urine production and help patients’ kidneys concentrate urine. Patients with nephrogenic diabetes insipidus would use these. Thiazide diuretics are sometimes combined with amiloride to prevent hypokalemia, or low potassium levels in the blood. Amiloride works to increase the amount of sodium and decrease the amount of potassium.
Aspirin or ibuprofen is sometimes used to help reduce urine volume as well. Do not use these drugs on a regular basis because of the risk of overdose. Symptoms of a ibuprofen overdose to look out for include: a ringing in the ears, blurred vision, headaches, confusion, dizziness, drowsiness and skin rashes.

5 Natural Treatments
1. Change Your Diet
A diet containing nutrient-dense whole foods with plenty of water-heavy fruits and vegetables can be helpful for people with diabetes insipidus. (10) Some examples of water-based, hydrating foods to consume regularly include: cucumbers, zucchini, dark leafy green vegetables (such as spinach and kale), red cabbage, red peppers, blueberries, watermelon, kiwi, citrus fruit, pineapple and strawberries. Starchy vegetables like sweet potatoes, squash, bananas and avocados are also great options. You may also find that coconut water is hydrating and helps to balance your electrolytes.
While you focus on adding these nourishing foods into your diet, try to avoid eating processed foods that are typically high in sodium and other chemicals that are used as preservatives. Removing caffeine from your diet may also be helpful, which includes carbonated soft drinks.
2. Avoid Dehydration
It’s vital for diabetes insipidus patients to drink enough liquids to replace their urine losses and to relieve excessive thirst. You need to drink extra water to compensate for fluid loss, especially after being active or exercising. Research shows that without enough water present in the body, dehydration and deficits can cause cardiovascular complications, muscle cramping, fatigue, dizziness and confusion. (11)
Make sure to always carry water with you wherever you go. Wearing a medical alert bracelet will alert professionals of your condition and advise them of your need for fluids.
3. Keep Your Electrolytes Balanced
The major electrolytes found within the body include calcium, magnesium, potassium, sodium, phosphate and chloride. These nutrients help to stimulate nerves throughout the body and balance fluid levels. You can keep your electrolytes balanced by avoiding packaged or processed foods because of their sodium content. Sodium is an electrolyte that plays a significant role in the body’s ability to retain or release water. So if your diet is very high in sodium, the kidneys excrete more water. This can cause complications balancing other electrolytes. It’s also important to drink enough water throughout the day and to increase your water intake after exercise, when you are sick or any time you are losing fluids. (12)
4. Keep Your Mouth Moist
Sucking on ice chips or sour candies can help to moisten your mouth and increase saliva flow, reducing your desire to drink. This can be especially helpful later in the evening when you don’t want to consume as much water and be up in middle of the night to use the bathroom.
5. Check Your Medications
Some medications can impact your electrolyte balance, a complication of diabetes insipidus. These include antibiotics, diuretics, hormonal pills, blood pressure medications and cancer treatments. Cancer patients who are receiving chemotherapy usually experience the most serious forms of electrolyte imbalances. Laxatives and diuretics also change potassium and sodium levels within the blood and urine. It’s also possible to develop electrolyte imbalances due to hormonal interactions from antidiuretic hormone medications, aldosterone and thyroid hormones. Even high levels of physiological stress can impact hormones to the point that fluid and electrolyte levels can become thrown out of balance. (13)
If you begin experiencing the signs and symptoms of diabetes insipidus, be sure to consider whether a new medication or supplement can be causing fluid or electrolyte imbalances.
Precautions
A major complication of diabetes insipidus is dehydration. You can prevent dehydration by increasing the amount of liquids that you drink. If you experience the signs of dehydration, such as confusion, dizziness or sluggishness, seek immediate care.
Final Thoughts
- Diabetes insipidus is a condition that disrupts normal life due to increased thirst and passing of large volumes of urine, even at night. It’s associated with inadequate vasopressin or antidiuretic hormone secretion.
- Issues with the release of vasopressin lead to this rare disorder that occurs when the kidneys pass an abnormally large volume of urine that is insipid — dilute and odorless.
- There are four different types of diabetes insipidus — central, nephrogenic, dipsogenic and gestational. Each type of diabetes insipidus has a different cause.
- The most common signs and symptoms of diabetes insipidus are extreme thirst and the excretion of an excessive amount of diluted urine. A person’s body regulates fluid by balancing liquid intake and removing extra fluid.
- Two major complications of diabetes insipidus are dehydration and an electrolyte imbalance.
- Desmopressin is a synthetic form of vasopressin used to treat diabetes insipidus. To treat this condition naturally, you must be sure to drink enough water to stay hydrated, watch your medications (some may be altering fluid balance), and change your diet.



