This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Diverticulitis Symptoms You Can Treat Naturally
December 27, 2016

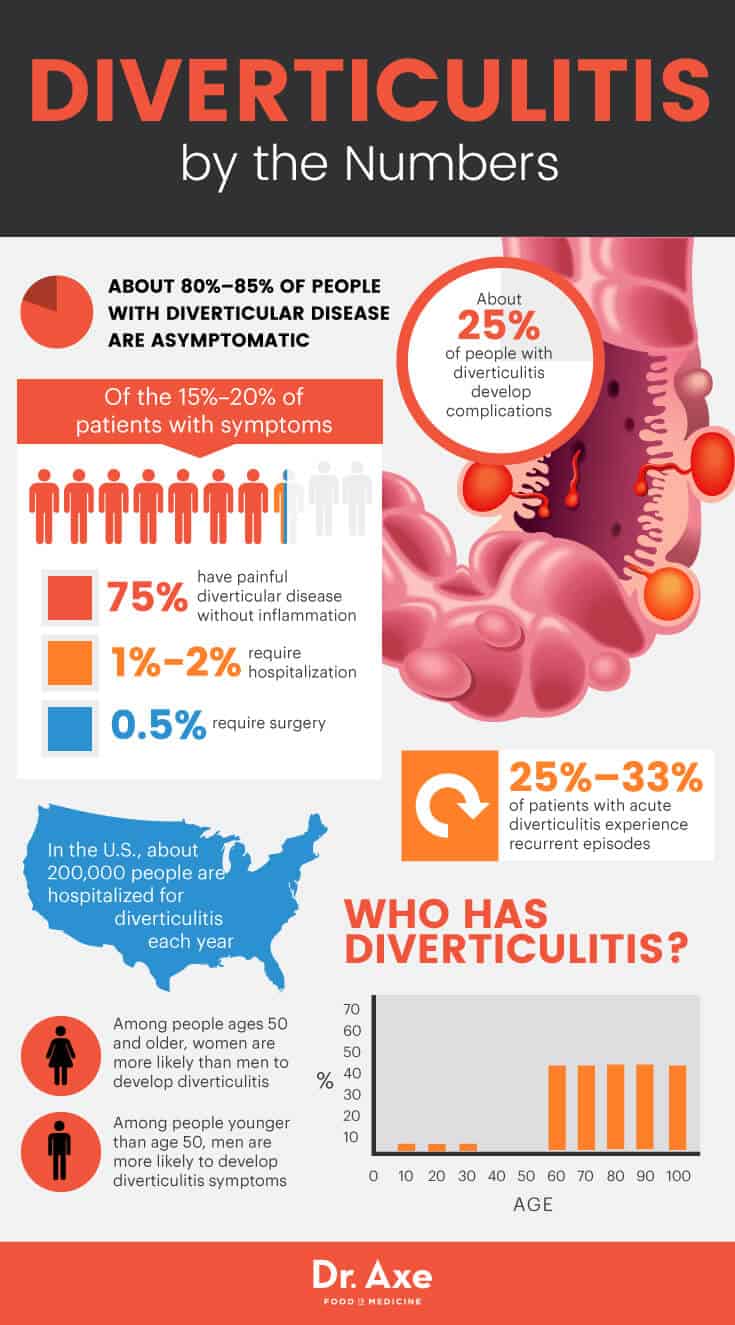
In the United States, about 200,000 people are hospitalized for diverticulitis each year. Diverticular disease can be a painful and upsetting disturbance in the digestive tract, and in severe cases, it can lead to hospitalization and surgery due to complications from diverticulitis symptoms.
The foods you eat and a variety of other risk factors can increase your chances of developing diverticulitis, especially after the age of 40. Conversely, following a diverticulitis diet and changing your lifestyle habits can help you relieve diverticulitis symptoms naturally.
What Is Diverticulitis?
Diverticulitis occurs when you have one or more pouches, or sacs, in the wall of your colon that have become inflamed. These small pouches (called diverticula), most commonly in the lower part of your colon called the sigmoid colon, form and push outward through weak spots in the colon wall. When the pouches form, this is called diverticulosis, which usually doesn’t cause any symptoms or problems. But when the pouches become inflamed or infected, this can lead to serious complications and hospitalization.
While the terms diverticulosis, diverticulitis and diverticular disease are often used interchangeably, they have different meanings. Diverticulosis refers to the presence of pouches in the colon, diverticulitis refers to the presence of inflammation and infection, and diverticular disease refers to the full spectrum of symptoms caused by the formation of pouches. (1)
When diverticula sacs become blocked with fecal matter, allowing bacteria to build, this can result in an infection and inflammation. As the sacs grow, they put an increasing amount of pressure on the walls of the intestine, leading to pain, gas, abdominal discomfort and other diverticulitis symptoms. (2)
Diverticulitis Symptoms
Although the majority of patients with diverticular disease do not have symptoms, research suggests that approximately 10 percent to 25 percent of patients develop symptoms, which may range from significant abdominal pain associated with fever and leukocytosis (the increase of the total number of white blood cells) requiring hospitalization to a large proportion of patients with recurrent, short-lived abdominal pain that may have significant impacts on their lifestyles.
According to research published in Therapeutic Advances in Gastroenterology, about 80 percent to 85 percent of people with diverticular disease are asymptomatic. Of the 15 percent to 20 percent of patients with symptoms, 75 percent of them have painful diverticular disease without inflammation, 1 percent to 2 percent require hospitalization and 0.5 percent require surgery. (3)
The most common of diverticulitis symptoms is pain in the lower left side of your abdomen that’s caused by the inflamed pouches. This severe pain usually comes on suddenly, and the intensity of pain can change over time, sometimes getting worse over several days. Acute diverticulitis is characterized by inflammation, microperforation and abscess formation, with 25 percent to 33 percent of patients experiencing recurrent episodes.
Other diverticulitis symptoms include:
- tenderness in the lower abdomen
- cramping
- bloating
- constipation or diarrhea
- fever and chills
- nausea
- vomiting
About 25 percent of people with diverticulitis develop complications, which may include: (4)
- Abscess — a painful, swollen, infected and pus-filled area just outside of your colon that makes you feel ill with symptoms like fever, nausea, vomiting and severe tenderness in your abdomen.
- Perforation — a small tear or hole in a pouch in your colon.
- Peritonitis — inflammation or infection of the lining of your abdomen, which is caused when pus and stool leak through a perforation.
- Fistula — an abnormal passage, or tunnel, between two organs, such as the colon and the bladder.
- Intestinal obstruction — a partial of total blockage of the movement of food or stool through your intestines.
Risk Factors and Root Causes of Diverticulosis Symptoms
People are more likely to develop diverticulosis and diverticulitis as they age. Research published in Clinics in Colon and Rectal Surgery indicates that diverticulosis is common in industrialized nations, and the prevalence increases dramatically with increasing age. Under the age of 30, about 1 percent to 2 percent of patients have diverticulosis, while this condition is found in over 40 percent of the population after the age of 60. Approximately 10 percent to 25 percent of patients with diverticulosis will develop diverticulitis.
Research also suggests that among people ages 50 and older, women are more likely than men to develop diverticulitis; however, among people younger than age 50, men are more likely to develop diverticulitis symptoms. (5)
Other risk factors for the development diverticulitis symptoms include:
- obesity
- smoking
- lack of physical activity/sedentary lifestyle
- a diet high in red meat and fat and low in fiber
- certain medications, such as NSAIDs, which increase the risk of complications of diverticulitis
Diverticulitis occurs when the diverticula, the marble-sized pouches that can form in the lining of your digestive system, develop when naturally weak places in your colon give way under pressure. This causes the pouches to protrude through the colon wall. When the pouches create a tear in the colon wall, it becomes inflamed or infected, which is called diverticulitis.
Conventional Treatment for Diverticulitis Symptoms
Treatment for symptomatic diverticular disease is largely based on the symptoms. Traditional therapy includes fiber, rest, antibiotics, pain control and surgery for selected cases. The goal of management of diverticular disease is to treat the infection, improve the symptoms, and prevent the recurrence of symptoms or development of serious complications.
Mesalamine is a medication that’s commonly used to treat certain bowel diseases. It works by decreasing swelling in the colon, and it’s used to reduce symptoms, such as rectal bleeding, stomach pain and diarrhea.
Rifaximin is an antibiotic that’s commonly used in the treatment of digestive and diverticular conditions. It’s typically used to treat traveler’s diarrhea and irritable bowel syndrome by dropping the growth of bacteria that causes diarrhea. Side effects of rifaximin include stomach pain, nausea, dizziness, excessive tiredness, headache, muscle tightening and joint pain.
If you have a severe attack or have other health problems, you’ll likely need to be hospitalized, and treatment will generally involve intravenous antibiotics and insertion of a tube to drain an abscess if one has formed.
If you experience complications, such as a perforation, abscess, fistula or bowel obstruction, you may need to have surgery to treat diverticulitis. It’s estimated that about 15 percent to 20 percent of all patients admitted to the hospital with acute diverticulitis, both complicated and uncomplicated, require surgical intervention during initial admission. Those with complicated diverticulitis are even more likely to require an operation during initial hospitalization, upward of 50 percent of the time. (6)
There are two main types of surgery for diverticulitis: Primary bowel resection removes diseased segments of your intestine and then reconnects the healthy segments, allowing you to have normal bowel movements. If there is too much inflammation to perform a primary bowel resection, you may need a bowel resection with colostomy, which involves creating an opening in your abdominal wall that’s connected to the healthy part of your colon. Waste then passes through the opening into a bag. Once there’s a reduction of inflammation, the colostomy may be reversed and the bowel reconnected. (7)
14 Natural Treatment for Diverticulitis Symptoms
Diet
Over the last four decades, researchers have been examining the role of dietary fiber in the development of diverticular disease. Recent research shows that fiber found in fruits and vegetables has the most protective effect, and a high intake of total fat and red meat increases the incidence of diverticular disease. In a Health Professionals Follow-Up Study encompassing 48,000 men, individuals with the highest fiber intake (more than 32 grams per day) had a risk reduction of 42 percent for development of diverticulitis compared to those with the lowest fiber intake. (8)
Based on this extensive research regarding dietary factors that are associated with the development of diverticulitis, I recommend the following guidelines for patients with diverticular disease:
1. Increase Fiber Intake to 20–30 Grams Per Day
To reduce your chance of developing diverticulitis, eat at least 20–30 grams of fiber per day, especially fiber found in fruits and vegetables. High-fiber foods, such as flaxseed, oat bran, spinach and cucumber, can be especially helpful.
2. Eat More Anti-Inflammatory Foods
Increase your consumption of anti-inflammatory foods, such as leafy green vegetables, celery, beets, broccoli, blueberries, walnuts, chia seeds, bone broth and coconut oil. Inflammation is the main feature of acute diverticulitis, so adding anti-inflammatory foods can help reduce diverticulitis symptoms. (9)
3. Consume Nuts, Grains and Popcorn
Although people with diverticula have long been advised to avoid nuts, grains, corn or popcorn because it was believed that undigested particles would remain lodged in portions of the diverticulum, recent research shows that the consumption of nuts or popcorn at least twice a week can reduce the risk of developing diverticulitis or diverticular hemorrhage by 20 percent for nuts and 27 percent for popcorn. (10)
4. Eat More Probiotic Foods
Eat probiotic foods, such as kimchi, sauerkraut, natto, yogurt and kefir. Probiotics should be added to your diet to help negate food sensitivities and relieve digestion issues, such as constipation, gas and bloating. If you have diverticulitis, you need an influx of these healthy bacteria to aid in the healing of your colon, while preventing disease recurrence.
5. Reduce Your Consumption of Red Meat
A case-control study examined 86 patients with diverticulitis and 106 controls; researchers found that individuals who consumed red meat at least once per day had 25 times the risk of developing diverticulosis compared to those who ate red meat less than once a week. (11)
6. Reduce Alcohol Consumption
A cross-sectional study found that individuals who consumed alcohol have a risk of developing diverticulosis that’s 2.2 times greater than the risk of people who do not consume alcohol.
Supplements
7. Slippery Elm
Slippery elm is a demulcent, meaning it protects irritated tissues and promotes healing, which is necessary in treating diverticulitis symptoms. (12)
8. Protein Powder Made from Bone Broth
Protein powder made from bone broth helps heal leaky gut and the digestive tract. Bone broth also helps you easily digest essential nutrients that your body needs, including calcium, magnesium, phosphorus, silicon and sulphur. (13)
9. Probiotics
A 2003 study involving 15 patients with uncomplicated diverticular disease experienced longer periods of remission and improved abdominal symptoms after receiving probiotic supplementation compared to treatment before. (14)
10. Aloe Vera
Aloe vera, in juice form, aids in digestion, helps normalize pH levels, regulates bowel processing and encourages healthy digestive bacteria. About 12–16 ounces of aloe vera juice (that does not contain aloe latex) is recommended, but any more than that can further irritate your system. (15)
11. Licorice Root
Licorice root lowers stomach acid levels, relieves heartburn and acts as a mild laxative, which can help you clear your colon of waste. It also helps increase bile, aiding your digestion, and it helps reduce spasms and inflammation in the gastrointestinal tract.
Natural Remedies
12. Increase Physical Activity
Research shows that increasing exercise may be associated with a reduced risk of developing diverticulitis symptoms, and being overweight is a risk factor for developing diverticular disease. (16)
13. Quit Smoking
A cross-sectional study found that the probability of diverticulosis was 30 percent greater among smokers. (17)
14. Avoid NSAIDs
Research suggests that chronic nonsteroidal anti-inflammatory medication use is almost twice as common in patients with diverticular disease as it is in healthy controls. (18)
Diverticulitis Precautions
The first step to reduce your chances of developing diverticulitis is to increase your fiber intake, but taking too much fiber too quickly may cause a worsening of symptoms, including diarrhea, gas or bloating. It’s better to gradually increase your fiber consumption in order to avoid these digestive issues.
Final Thoughts on Diverticulitis Symptoms
- People are more likely to develop diverticulosis and diverticulitis as they age. Other risk factors for the development diverticulitis symptoms include gender, obesity, smoking, lack of physical activity, a diet high in red meat and fat and low in fiber, and certain medications.
- Diverticulitis occurs when you have one or more pouches, or sacs, in the wall of your colon that become inflamed. These small pouches (called diverticula), most commonly in the lower part of your colon called the sigmoid colon, form and push outward through weak spots in the colon wall.
- The most common diverticulitis symptom is pain in the lower left side of your abdomen that’s caused by the inflamed pouches.
- Treatment for symptomatic diverticular disease is largely based on the symptoms. Traditional therapy includes fiber, rest, antibiotics, pain control and surgery for selected cases.
- Natural treatments for diverticulitis include eating a high-fiber diet with more anti-inflammatory and probiotic foods and using supplements, such as slippery elm, aloe vera and protein powder made from bone broth. Lifestyle changes like increasing physical activity, losing weight and quitting smoking are also helpful in treating diverticulitis symptoms.





