This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
How Lyme Disease Affects the Brain (And Mimics Other Diseases)
April 5, 2018
Did you ever wonder how Lyme disease affects the brain, including symptoms of brain fog? The U.S. Centers for Disease Control and Prevention estimates that about 200,000 people are diagnosed every year with Lyme disease.
But many believe the true number of people suffering from Lyme in the United States is actually much higher. That’s because Lyme disease symptoms vary greatly and can impact different people in different ways. Aside from that, the ELISA screening test most doctors use misses up to 35 percent of Lyme cases, making it a horrible first-line detection for the disease. (Screening tests should have an accuracy of at least 95 percent.) (1)
The problem is likely only going to get worse, too, being that Lyme is among the major health effects of climate change.
Even with many cases missed in the doctor’s office, Lyme disease is still the most common tickborne disease in the northern hemisphere. Despite being so common, Lyme disease symptoms vary depending on the patient and how the bacteria impacts different systems of the body. In fact, Lyme disease often mimics other diseases or illnesses and be referred to as the new “great imitator.” (2)
Lyme disease is often misdiagnosed as such diseases, including: (3)
- Chronic fatigue syndrome
- Fibromyalgia
- Multiple Sclerosis
- Dementia
- Alzheimer’s disease
- Autism-like syndromes
- Various psychiatric illnesses (For instance, a tickborne infection may cause panic attack symptoms)
In about 15 percent of cases, Lyme disease has a prominent effect on the nervous system. (That number may be higher, since public health official acknowledge there are likely thousands of cases of undignosed Lyme disease every year.) Even with its known profound effects on the nervous system, there are still many questions and unknown answers as to what is happening during and following the transmission of Lyme disease. Let’s take a close look at Lyme disease and central nervous system involvement…
How Lyme Gets Into Your Brain
To understand how Lyme disease affects, the brain, it’s important to understand the different phases of the infection. (And how the disease is transmitted in general.) Ticks, specifically deer ticks in the northeastern U.S., are the carriers of the bacteria spirochete Borrelia burgdorferi that causes Lyme disease. In particular, it’s the small, immature tick nymphs that feed on animals like the white-footed mouse, squirrels and other small mammals that serve as reservoirs for Borrelia burgdorferi. Later, an infected tick will attach themselves to a person or other mammal. Once attached, the tick will gorge on the blood of its host for several days. Many
Infection Phase
Even prior to entering the host, S. Borrelia Burgdorferi has its work to do. Host blood enters the tick gut during feeding, as S. Borrelia Burgdorferi simultaneously begins to multiply in preparation to travel to the ticks salivary glands. As the bacteria enter the host, there are several mechanisms that make it difficult for the immune system to attack and eradicate S. Borrelia Burgdorferi. (4)
First, to avoid an immune response from the host, the bacteria decrease the number of surface proteins that signal a pro-inflammatory response. These proteins are normally found at high levels within the tick gut, but are significantly decreased during feeding periods. (5)
Also, there is a upregulation of another surface protein that binds with inhibitor protein protecting the bacteria from the host immune system. The increased expression of this protein is essential for the survival of the infection within the host for the first 48 hours. The bacteria also induce the increase of anti-inflammatory cytokines, which play in modulating the immune response of the host. (6)
Studies show that another way the Borrelia burgdorferi avoid immune detection is by hiding. The extracellular matrix of cells are considered to be immuno-privileged and, as it turns out, a good place to hide. Borrelia burgdorferi can cause a cascade of events that lead to the local increase of a protein that digests the surrounding extracellular matrix. This allows for the bacteria to attach to the matrix. (7, 8)
Following the initial invasion into the host, researchers believe the bacteria utilize the bloodstream to gain access various other organs within the body, including the brain. Though it is still unknown how the bacteria transverse the blood-brain barrier to gain access to the brain, it is thought that the bacteria gains entry by ‘slipping’ through the endothelial cells which make up the blood-brain barrier or by a transcellular passage. (9)
Once the bacteria is in the central nervous system, the local immune system becomes activated. The immune cells consisting of monocytes, macrophages and dendritic cells activate the proinflammatory response of the brain. There is an increase in chemokines, that in turn attract more immune cells causing an even larger inflammatory response. (10, 11, 12)
How Lyme Disease Affects the Brain
Signs of infection may begin within days of a tick bite. Symptoms are characterized by three main stages: early localized, early disseminated and late disseminated. The latter can affect the immune, cardiac and neurological systems. The early localized stage occurs within days or weeks of the onset of the initial infection. Sometimes, an erythema migrans rash, often shaped like a bull’s eye, surfaces. Although the Bull’s eye rash is considered a classic sign of Lyme, it’s present in only about 50 percent of cases. (13)
But Lyme rashes aren’t always bull’s eyes. Research shows some clinicians misdiagnose a Lyme-related rash as spider bites, cellulitis or even shingles. (14)
Days to weeks after infection, the bacteria spread throughout the body in the early disseminated stage. These symptoms include:
- Fatigue
- Chills
- Fever
- Headache
- Stiff neck
Some or all of these symptoms may last for weeks, though intermittent, and fluctuate in intensity.
During this stage, patients may begin to show Lyme disease central nervous system symptoms, or acute Lyme neuroborreliosis, within weeks to months of the initial onset of the tick bite.
Lastly, when left untreated, Lyme disease will progress to late disseminated stage months to years after the initial infection. Symptoms of this stage include joint pain, arthritis, and a transition from acute neuroborreliosis to chronic neuroborreliosis.
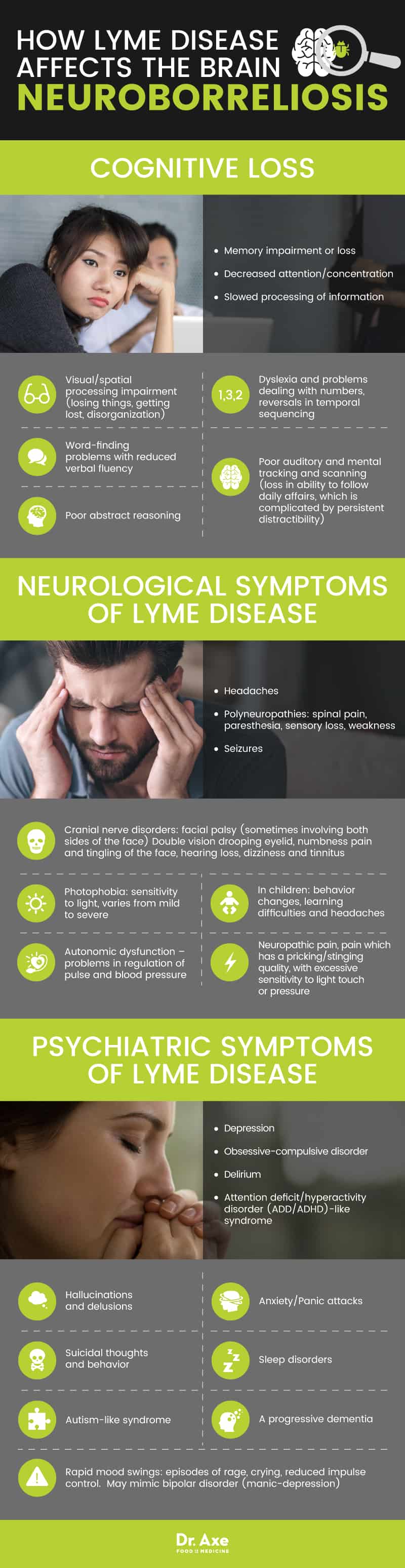
How Lyme Disease Affects the Brain: Neuroborreliosis
One of the most debilitating aspects of Lyme disease is neuroborreliosis. Patients often describe their quality of life living with neuroborreliosis as being poor. The symptoms of neurological dysfunction are vast and can be classified into three categories:
Cognitive Loss
- Memory impairment or loss
- Decreased attention/concentration
- Slowed processing of information
- Visual/spatial processing impairment (losing things, getting lost, disorganization)
- Dyslexia and problems dealing with numbers, reversals in temporal sequencing
- Word-finding problems with reduced verbal fluency
- Poor abstract reasoning
- Poor auditory and mental tracking and scanning (loss in ability to follow daily affairs, which is complicated by persistent distractibility)
Neurological Symptoms of Lyme Disease
- Headaches
- Polyneuropathies: spinal pain, paresthesia, sensory loss, weakness
- Cranial nerve disorders: facial palsy (sometimes involving both sides of the face), double vision, drooping eyelid, numbness pain and tingling of the face, hearing loss, dizziness and tinnitus
- Neuropathic pain, pain which has a pricking/stinging quality, with excessive sensitivity to light touch or pressure
- Seizures
- Photophobia: sensitivity to light, varies from mild to severe
- Autonomic dysfunction – problems in regulation of pulse and blood pressure
- Mimic other defined neurological disorders such as Parkinson’s disease symptoms, MS, Bell’s palsy, stroke, and ALS, Encephalomyelitis
- In children, indications of neurological involvement include behavior changes, learning difficulties and headaches
Psychiatric Symptoms of Lyme Disease
- Hallucinations and delusions
- Rapid mood swings: episodes of rage, crying, reduced impulse control. May mimic bipolar disorder (manic-depression)
- Depression
- Suicidal thoughts and behavior
- Anxiety/Panic attacks
- Obsessive-compulsive disorder (OCD)
- Sleep disorders
- Attention deficit/hyperactivity disorder (ADD/ADHD)-like syndrome
- Autism-like syndrome
- Delirium
- A progressive dementia
The presentation of neurological dysfunction caused by S. Borrelia burgdorferi varies. And although the pathophysiology behind it remains unclear, the theory is this: Researchers believe it’s caused by direct cytotoxicity, neurotoxic (causing damage to neural cells/tissue) mediators and triggered autoimmune reactions.
Cytotoxicity is the ability of cells to be toxic and result in the death of another cell. Within the brain, astrocytes are cells that provide support for cells that make up the blood-brain barrier and help maintain the nutrient supply to neural tissue. S. Borrelia burgdorferi has been shown to induce astrogliosis, a process of rapid cell multiplication and then cell death, in astrocytes.
Borrelia burgdorferi has also been shown to induce astrocytes and microglia to produce toxic substances which can damage nerve cells which could lead to memory impairment, decreased concentration and fatigue. Alterations in neurotransmitter levels, such as a decrease in tryptophan (a precursor to serotonin), may play a role in the psychiatric symptoms.
Varying neurotransmitter levels may be responsible for the symptoms of stress, anxiety and sleep disorders as well. Lastly, the induction of cytokines produced by S. Borrelia burgdorferi is believed to cause an autoimmune-mediated reaction that is not clearly understood. (15, 16)
Diagnosis Issues
There is no absolute reliable diagnostic test available for Lyme disease, since most testing available results in false positives or false negatives. Blood testing and Western blot analysis can be used but are not highly sensitive and the results can be inaccurate. Individuals with chronic neurological symptoms may have brain MRI and late-stage Lyme disease testing done, including cerebrospinal fluid testing, in conjunction with other tests to determine the presence of S. Borrelia burgdorferi.
Lyme disease brain MRI scans may also show brain involvement Interestingly, Lyme disease brain lesions sometimes show up on brain scans and look similar to multiple sclerosis lesions. (17) Lyme disease lesions on the spine are also possible. (18)
Clinical representation of Lyme disease is often the best way for diagnosis. Rashes are often present, but not in all cases and can be easily overlooked. The best diagnostic option may be to use several methods together since this disease has such a prolific reach of symptoms.
Treatment
Does Lyme brain fog go away? I have seen people with neurological Lyme disease symptoms feel well again. And there are natural strategies to treat Lyme disease. In my opinion, the real cause of chronic Lyme disease includes weakened immunity, inhibited cellular function and environmental factors. So to truly heal from Lyme disease, there’s a lot to address.
An individualized, integrative approach may prove to be the best approach for treatment since there are several stages of the disease and far-reaching symptoms that affect several systems within the body.
The conventional therapy includes oral antibiotics, even sometimes intravenous antibiotics. But there are other supplemental treatments, including antivirals, immune modulators, hormonal therapies and nutritional supplements. A diet of anti-inflammatory foods such as leafy green vegetables, fish, nuts and fruits may also be helpful in reducing the autoimmune effects of the disease. Lyme disease brain fog treatment and a neurological Lyme disease cure will likely require a suite of lifestyle changes and the right supplements for your particular case, including a focus on fixing methylation problems. (19)
Prevention
There are several preventative measures that can be taken to reduce the risk of contracting Lyme disease.
- First, prior to outdoor activities use a homemade bug spray to repel ticks.
- Other nontoxic tick repellents include essentials oils like lavender, rosemary, tea tree, peppermint, lemongrass and sage. Lemongrass possesses tick-repelling properties.
- When hiking outdoors or playing in wooded or higher grass areas, wear long sleeves and long pants tucked into socks or cuffed at the bottom.
- Wear light-colored clothing so you can spot ticks easier and remove them immediately.
- Following outdoor activities, change clothes promptly and place them in the washer/dryer.
- Check for ticks immediately; since the nymphs are tiny and can often be overlooked, look for a rash a few days following the event.
Final Thoughts
- Lyme disease is highly prevalent in the U.S. and many people have the disease and don’t even know it.
- Symptoms vary and affect nearly every system of the body.
- Since characteristic symptoms are so wide-ranging and diffuse, it is often difficult to diagnose this disease.
- There is no single appropriate diagnostic method.
- How does Lyme disease affect the brain? Neuroborreliosis affects an individual’s cognitive and neurological functions and causes various psychiatric symptoms that severely diminish an individuals’ quality of life.
- It’s critical that more research is done to allow for a better understanding of neuroborreliosis so a more appropriate diagnostic testing system can be utilized.



