This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
How to Get Rid of Hemorrhoids (4+ Natural Remedies)
April 25, 2023

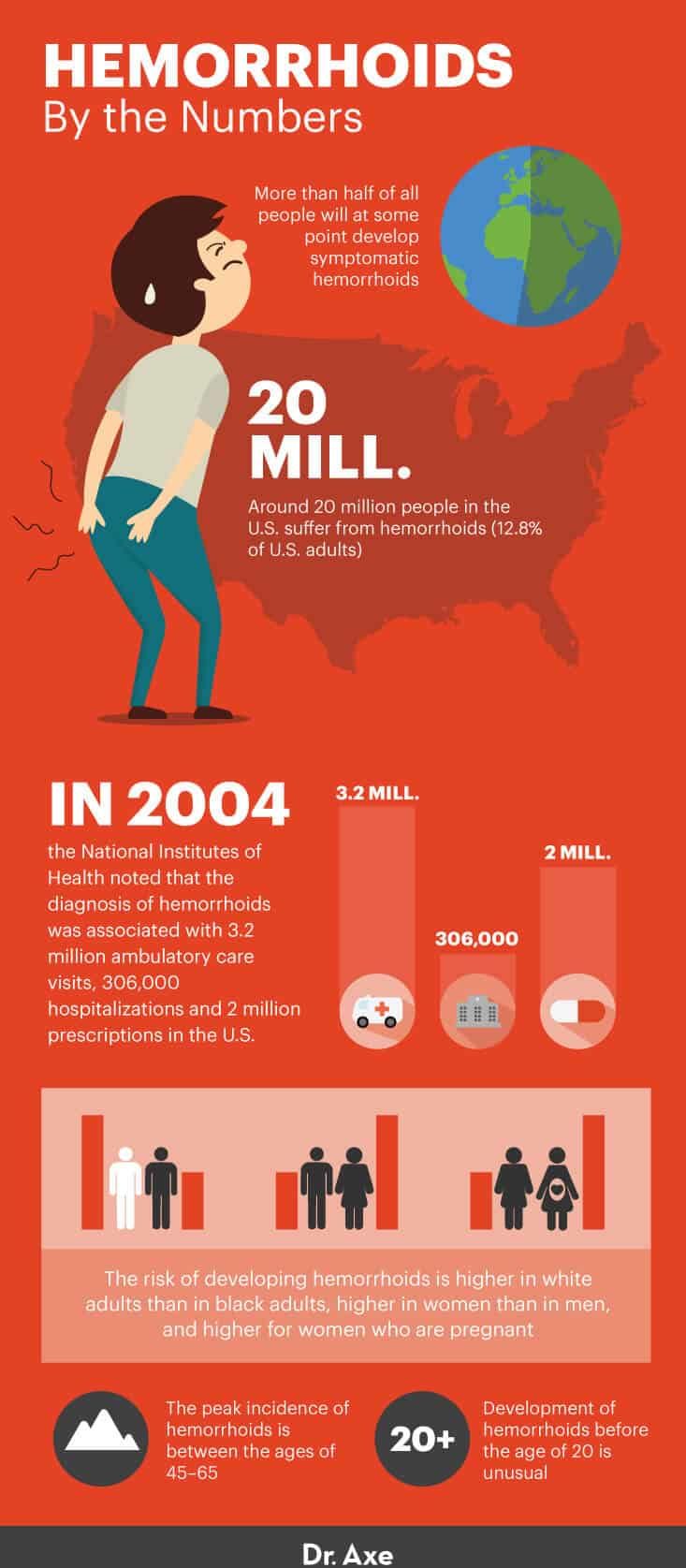
Hemorrhoids are a very common anorectal condition that affects millions of people around the world. More than half of all people will develop symptomatic hemorrhoids at some point, so it’s common to wonder how to get rid of hemorrhoids.
Most patients are able to get rid of hemorrhoids with a high-fiber diet, herbal supplements and non-surgical medical treatments, such as my DIY Hemorrhoid Cream with Turmeric and Tea Tree Oil.
Hemorrhoids are frequently seen in primary care clinics, emergency wards, gastroenterology units and surgical clinics, but how do you know when they have developed and when you should see a doctor? These are common concerns among people who develop hemorrhoids and don’t know how to deal with and treat the pain.
Thankfully, there are natural treatments for how to get rid of hemorrhoids fast, and starting there may help relieve these literal pains in the butt.
What Are Hemorrhoids?
Now, you might be wondering why it’s so important to know how to get rid of hemorrhoids, especially if you’ve never experienced hemorrhoid symptoms before. Well, it’s because no one is immune to them.
I bet you didn’t know that we all have hemorrhoids, but it’s true. Hemorrhoids are normal cushions of tissue that are filled with blood vessels and found at the end of the rectum, just inside the anus. Together with a circular muscle called the anal sphincter, hemorrhoids help control bowel movement.
When people say that they “have hemorrhoids,” what they really mean is that their hemorrhoids have become enlarged. Enlarged hemorrhoids are often associated with symptoms such as itching, mucus discharge or bleeding. Bleeding happens when hard stool damages the thin walls of the blood vessels in hemorrhoids.
The two basic types include internal and external hemorrhoids. Internal hemorrhoids are more common, and external hemorrhoids tend to feel like a large lump around the outside of the anus that can make sitting painful. Bleeding is fairly common with a swollen external hemorrhoid.
Swollen internal hemorrhoids might come out of the anus and can then be seen as soft lumps of tissue. These are called protruding or prolapsed hemorrhoids. Larger hemorrhoids can make it feel like something is pushing against the anus, which can make sitting very uncomfortable.
Hemorrhoids are classified by grade, which is based on how severe they are:
- Grade 1: Slightly enlarged hemorrhoids that cannot be seen from outside the anus.
- Grade 2: Larger hemorrhoids that may come outside of the anus at times, like when passing stool, but then go back in on their own.
- Grade 3: Hemorrhoids that come out of the anus when passing stool or engaging in physical activity and do not go back in on their own. They can only be pushed back inside the anus.
- Grade 4: Hemorrhoids that are always outside the anus and can no longer be pushed back inside. A small bit of the anal lining may also come down from the lower rectum and out of the anus, which is known as rectal prolapse.

The most common symptom of hemorrhoids is anal bleeding, and chief complaints include a perianal mass protruding from the anus and anal discharge. Other symptoms of hemorrhoids include:
- irritation and itching around the anus
- fecal leakage
- sensitive lumps in the anus
- painful bowel movements
- protrusion of skin during bowel movements
- blood on toilet paper after having a bowel movement
A particularly painful form of Grade 4 hemorrhoids comes in the form of a thrombosed hemorrhoid. This refers to (usually) external hemorrhoids that have no blood flow because the vein connected to them has a thrombosis (blood clot).
The thrombosis responsible for a thrombosed hemorrhoid will often reabsorb within two to three weeks without major treatment. Pain originating from the swelling and inflammation of the hemorrhoid is usually worst in the first 24–48 hours after it develops.
People with hemorrhoids are at an increased risk of portal hypertension. According to WebMD, “Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver.”
Many people find themselves wondering, “Do hemorrhoids go away?” Most swollen hemorrhoids do go away, given that you follow a wise regimen of diet and bathroom habits, as well as any other additional treatment methods recommended by your physician.
How long do hemorrhoids last? Hemorrhoid symptoms clear up within a few days for most people, but they may reoccur and/or require medical attention in some cases.
If symptoms continue for more than a week or two and haven’t been improved by home treatment, it’s probably time to visit the doctor. For those who already have frequent hemorrhoids, dietary intervention may be one of the best ways to get rid of external and internal hemorrhoids once and for all.
Although people assume that any anal pain while using the toilet is from hemorrhoids, there are a number of other anorectal disorders that can cause symptoms, including dermatologic diseases, diverticulitis, abscess and fistula, fissure, sexually transmitted diseases, warts, HIV, infections, and inflammatory ulcers. These conditions will be ruled out by your doctor when you go for a rectal exam if they aren’t the cause.
Diverticulitis vs. Hemorrhoids
People are sometimes confused by the difference between diverticulitis and internal hemorrhoids. Diverticulitis is a condition in which sacs or pouches within the colon walls become inflamed and press into the colon. While some of the symptoms and root problems are similar to what causes hemorrhoids, diverticulitis tends to be a bit more serious and is related closely to age and poor dietary fiber intake.
Causes
Researchers propose that degradation (or disintegration) of the supporting tissues of the anal cushions causes hemorrhoids to develop. There are some contributing factors for hemorrhoids, including:
- being overweight
- regularly lifting heavy objects
- aging
- pregnancy and giving birth
- heredity
- constipation or chronic diarrhea
- faulty bowel function due to overuse of laxatives or enemas
- spending excessive periods of time on the toilet
An increase in intra-abdominal pressure during pregnancy or when constipated and sitting on the toilet for a prolonged period of time while straining are major contributing factors for the development of hemorrhoids. Weakening of supporting tissue as a result of aging and genetics may also serve as another cause.
Conventional Treatment
When you go to see a doctor for enlarged hemorrhoids, he or she will look at your anus to see if it’s inflamed and whether the hemorrhoids come out of the anus when you push or if they’re already outside. Depending on the severity of your symptoms, there are a number of examinations your doctor may choose to perform in order to make a diagnosis.
Doctors typically do a digital rectal examination first, which involves gently inserting a finger into the anus with gloves and lubricant. The doctor will feel the inside of the anal canal using circular movements, which allows him to examine the sphincter muscles and the texture of the membranes lining the anus.
If your doctor believes that you do have enlarged hemorrhoids, she will most likely perform a proctoscopy next. This involves inserting a short tube with a light and lens on it (the proctoscope) that exams the membranes lining the rectum.
The doctor is looking to see if there are enlarged hemorrhoids and how big they are. People tend to fear the pain and discomfort that come with these procedures, but they usually don’t hurt and do help your doctor make suggestions about how to get rid of hemorrhoids.
Most of the patients suffering from hemorrhoids have their symptoms alleviated through diet therapy, fiber supplements, hemorrhoid cream and medical treatments — such as sclerotherapy, rubber band ligation and infrared coagulation.
1. Sclerotherapy
Sclerotherapy is a procedure that involves injecting a chemical (the sclerosant) into a vein to destroy it. The sclerosant is used to damage the innermost lining of the vessel, which results in a clot that blocks the blood circulation in the vein. Over time, the vessel turns into scar tissue and fades away.
In 2010, a group of 338 Japanese medical institutions reported good results for sclerotherapy using aluminum potassium sulfate and tannic acid (ALTA). Upon injecting ALTA into Grade 2, 3 and 4 hemorrhoids, of 3,519 patients, 98 percent reported positive effects within 28 days. The recurrence rate after two years was 18 percent, and complications included pyrexia, low blood pressure, perineal pain and rectal ulcers, but those were mild.
2. Rubber Band Ligation
This procedure is used to remove a hemorrhoid with a rubber band. Your doctor inserts a small tool called a ligator through a lighter tube into the anal canal. Then the doctor grasps the hemorrhoid with forceps, slides the ligator’s cylinder upward and releases the rubber band around the base of the hemorrhoid.
The rubber band cuts off the hemorrhoid’s blood supply and causes it to wither away.
A 2000 study published in Digestive Surgery found that rubber band ligation is a useful, safe and successful method for treating symptomatic second- and third-grade hemorrhoids and can be applied successfully in fourth-grade cases but with an increased rate of recurrence and additional treatments required.
3. Infrared Coagulation
Infrared coagulation is a procedure that’s used for internal hemorrhoids. The doctor uses a device that creates an intense beam of infrared light to cause scar tissue and cut off the blood supply to the hemorrhoid.
When the hemorrhoid dies, a scar forms on the anal canal below the lower rectum, and the scar tissue holds nearby veins in place so they can’t bulge into the anal canal.
A 2003 study compared infrared coagulation and rubber band ligation in terms of effectiveness and discomfort. Researchers found that postoperative pain during the first week after treatment was more intense in the band ligation group. Pain and a feeling of constantly having to pass stool was also more intense with band ligation.
Patients in the infrared coagulation group returned to work earlier, but they also had a higher recurrence or failure rate. Researchers concluded that band ligation, although more effective in controlling symptoms and obliterating hemorrhoids, is associated with more pain and discomfort to the patient — something to keep in mind when you’re looking for ways on how to get rid of hemorrhoids.
4. Hemorrhoid Surgery
Surgical intervention is now less frequently performed than in the past, but it can be considered for patients with acute complications of hemorrhoidal disease or for those who were unable to treat hemorrhoids with other measures. Surgery for hemorrhoids, known as a hemorrhoidectomy, involves removing the hemorrhoid or the clot with a small incision. Having a hemorrhoidectomy is generally an outpatient procedure and involves a two- to three-week recovery period.
Having hemorrhoid surgery can seem frightening, but it is a relatively minor procedure that doctors recommend when all other treatment methods have failed.
How to Get Rid of Hemorrhoids Naturally
1. Improve Your Diet
Eat High-Fiber Foods
To get rid of hemorrhoids, it’s important that you avoid constipation and hard stool, which can be done by eating plenty of high-fiber foods to make stools soft. For how to get rid of hemorrhoids, the recommendation is 30–35 grams of fiber daily.
Eat foods such as:
- avocados
- berries
- figs
- Brussels sprouts
- acorn squash
- beans
- lentils
- nuts
- flaxseeds
- chia seeds
- quinoa
In clinical studies, high-fiber diets reduced the risk of persisting symptoms and bleeding by approximately 50 percent.
Drink Plenty of Water
Dehydration can lead to constipation because water and fluids are required for fiber to travel smoothly through the digestive tract. Many studies, including one published in the European Journal of Clinical Nutrition, indicate that fluid loss and fluid restriction can increase constipation, which can worsen hemorrhoid symptoms.
To relieve constipation and as a way for how to get rid of hemorrhoids, drink at least one glass of water with each meal and snack of the day.
Eat Fermented Foods
Fermented foods like kefir, kimchi and raw, pastured yogurt can help provide the digestive system with healthy bacteria that are essential for proper elimination. Several studies have shown that fermented foods and probiotics improve intestinal tract health, synthesize and enhance the bioavailability of nutrients, modify gut pH, and aid digestion.
Limit Alcohol and Spicy Foods
Alcohol can be dehydrating and hard on the digestive system, making hemorrhoid symptoms worse, while spicy foods can intensify the symptoms of hemorrhoids. Some studies show that both alcohol and spicy foods consumption serve as risk factors for hemorrhoids, although the data isn’t consistent.
To be safe, limit these foods until the hemorrhoids have cleared up.
2. Practice Better “Toilet Habits”
Avoid Straining
Straining during a bowel movement can be painful and make hemorrhoid problems even worse.
Don’t wait too long before going to the toilet. Pay attention to your body’s signals, and when you feel an urge to use the bathroom, go right away.
Otherwise the stool will become harder, and this will automatically make you push harder. When you’re at the toilet, take your time, and relax your body.
Prevent Constipation
Constipation forces you to strain while using the bathroom, and that will increase the pain and inflammation of the hemorrhoid. To avoid constipation, drink plenty of fluids, engage in regular physical activity and eat high-fiber foods that make stools soft. These steps also help answer how to get rid of hemorrhoids or prevent them in the first place.
Avoid Prolonged Sitting on the Toilet
Spending too much time on the toilet can worsen hemorrhoids.
Don’t read or distract yourself while using the bathroom. This only leads to more time spent straining. (Read: Put the phone down.)
Clean Yourself Thoroughly
If stool is left behind after you wipe, it can aggravate hemorrhoids even more, which is why it’s important to cleanse yourself thoroughly after going to the bathroom. Do not, however, cleanse yourself too roughly or use soaps that contain harsh chemicals, alcohol or perfumes.
Instead, use plain water to wipe yourself, and then dry your bottom afterward. A sitz bath is helpful to patients with anal itching, aching or burning and is known as one of the best ways to get rid of hemorrhoids fast.
3. Take Helpful Supplements
Butcher’s Broom
Butcher’s broom can help reduce swelling and inflammation of hemorrhoids. A 2002 study conducted in Germany found that butcher’s broom was an effective means of treatment for patients suffering from chronic venous insufficiency, a condition where the flow of blood through the veins is inadequate, causing the blood to pool.
Pycnogenol®
A 2010 study published in Phytotherapy Research investigated the efficacy of orally and topically applied Pycnogenol® hemorrhoid cream for the management of acute hemorrhoidal attacks in a controlled, randomized study with 84 subjects. Within less than 48 hours of an attack, patients were enrolled and their signs and symptoms were scored.
The decrease in scores was significantly more pronounced in the Pycnogenol® group than in the control group given placebo. The study indicates that oral and topical Pycnogenol® helps heal acute hemorrhoids.
Horse Chestnut
Horse chestnut is commonly used as an herbal remedy for poor blood flow and swelling. According to research published in Alternative Medicine Review, horse chestnut has been shown to improve microcirculation, capillary flow and vascular tone, all of which are helpful for how to get rid of hemorrhoids.
Witch Hazel
Witch hazel is a plant that’s used for its skin-healing, astringent and antioxidant properties. Topical application of witch hazel can help soothe hemorrhoids by reducing inflammation and pain.
Psyllium Husk
Psyllium husk is a natural source of pure fiber that’s sold in powder form. Studies suggest that plant fibers like psyllium husk can reduce the frequency of bleeding when using the bathroom and help avoid constipation or straining. When using psyllium husk, make sure to drink plenty of water.
A 2011 animal study published in Digestive Diseases and Sciences found that psyllium husk has a gut-stimulatory and laxative effect on mice, and at higher doses it has antisecretory (reducing the normal rate of secretion of a body fluid) and antidiarrheal activity.
MSM
MSM supplements seem to help treat hemorrhoids, according to studies. Applying a gel containing MSM along with tea tree oil can reduce pain and swelling caused by hemorrhoids (swollen blood vessels of the rectum that make it hard to go to the bathroom without pain or bleeding).
4. Try Beneficial Essential Oils
Cypress Oil
Cypress essential oil stops excess blood flow and promotes the clotting of blood. This is due to its hemostatic and astringent properties.
Cypress oil helps with the contraction of blood vessels, and it tightens tissues. It’s also known to reduce anxiety, which can help relieve constipation for some people.
Use cypress topically by adding three to four drops to a cotton ball and applying to the area of concern.
Helichrysum
Helichrysum essential oil helps stimulate the secretion of gastric juices that are needed to break down food and prevent digestive issues. It also serves as an anti-inflammatory agent when applied topically.
To use helichrysum, rub two to three drops into the abdomen or area of inflammation.
Hemorrhoids by the Numbers
Precautions
A common concern is that hemorrhoids increase the risk of colorectal cancer, but that’s not true. However, the two conditions do cause similar symptoms. This is why it’s important to mention your hemorrhoids to your health care provider.
Even when a hemorrhoid is healed completely, a colonoscopy may be done to rule out other causes of rectal bleeding. According to the American Society of Colon and Rectal Surgeons, every person age 50 and older should undergo a colonoscopy to screen for colorectal cancer.
Conclusion
- Hemorrhoids are a very common anorectal condition that affects millions of people around the world.
- Enlarged hemorrhoids are often associated with symptoms such as itching, mucus discharge or bleeding. Bleeding happens when hard stool damages the thin walls of the blood vessels in hemorrhoids.
- Avoidance of constipation is key when trying to get rid of hemorrhoids. It’s important that you don’t strain while using the bathroom, don’t sit for an excessive period of time and clean yourself thoroughly when finished.
- Foods and herbal supplements that help relieve constipation can alleviate the symptoms of hemorrhoids. A high-fiber diet and drinking plenty of fluids are the most helpful dietary changes you can make when it comes to how to get rid of hemorrhoids.
- If non-medical treatments don’t work, there are relatively painless procedures that can be done to treat hemorrhoids. For extreme cases, an outpatient surgery called a hemorrhoidectomy may be required.

