This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Hypernatremia: Symptoms + 4 Natural Treatments for Prevention
March 15, 2017
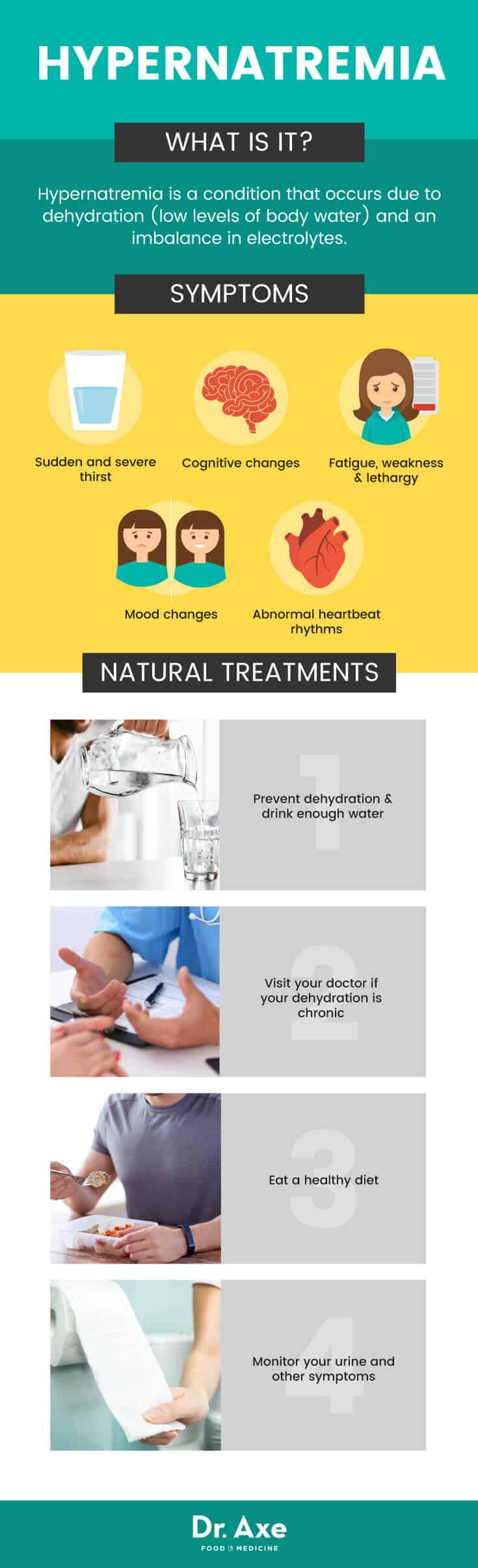
Hypernatremia is a condition that occurs due to dehydration (low levels of body water) and an imbalance in electrolytes, including sodium and potassium. A key difference between hypernatremia and common dehydration is who these problems usually affect. Athletes or those who don’t drink enough water are more prone to experiencing dehydration; however, the elderly or people recovering from illnesses and surgery are most likely to develop hypernatremia symptoms.
While sodium, an essential electrolyte and mineral, has important roles in the body, too much relative to water and potassium levels can cause hyponatremia symptoms or dangerous complications. (1) Depending on how severe the condition becomes, symptoms such as weakness, confusion, dry mouth and complications like heart or cognitive problems can all occur.
What Is Hypernatremia?
Too much water loss and/or too much sodium gain characterizes hypernatremia. This is the opposite of hyponatremia, a condition that leads to a severe decrease in sodium. Technically the definition of hypernatremia is “a rise in serum (blood) sodium concentration to a value exceeding 145 mmol/L.” (2) The Cleveland Clinic states: “It is most commonly caused by the loss of water via the skin, urine, or gastrointestinal (GI) tract.”
How common of a problem is hypernatremia? While we hear a lot about the dangers of consuming too much salt/sodium, and hypernatremia can be a serious condition, it’s not very common. It only occurs when the thirst response in impaired or water is not available.
- Studies have found that the prevalence of hospitalized patients with hypernatremia varies. But it’s much higher in general than in those who develop the condition before coming to the hospital. In fact, over 60 percent of hypernatremia cases are believed to be acquired by patients while in the hospital. (3)
- Around 1-10 percent of all hospital patients develop severe hypernatremia (higher prevalence exists among older patients). Only about .01-1.4 percent of patients visiting a hospital have the condition before admission.
- Elderly patients and those in critical care experience electrolyte imbalances most often. Between 9-26 percent of critically ill patients will develop hypernatremia symptoms. Certain studies have found that mild hypernatremia can affect up to 22.2 of geriatric hospital patients, 19 percent of those in nursing homes, 6 percent of non-geriatric patients, and up to 7 percent of patients taken to the hospital via an ambulance. (4)
Common Signs and Symptoms of Hypernatremia
Sometimes patients with hypernatremia aren’t aware of their condition until it becomes serious. This can happen since they don’t experience normal thirst signals. When symptoms of hypernatremia do occur, they can include:
- Thirst, sometimes which is sudden and severe. This is polydipsia, the term given to excessive thirst. It’s one of the first symptoms to emerge due to diabetes. (5) Intense thirst might also be accompanied by polyuria, or the production of large volumes of dilute urine. In this case urine is usually lighter in color than normal (less yellow). Also, the need to urinate happens more frequently. (6)
- Cognitive changes involving the central nervous system (CNS) which can include brain fog, confusion and dizziness.
- Fatigue, weakness and lethargy, including muscular aches or weakness and trouble moving normally.
- Mood changes such as irritability.
- Experiencing involuntary myoclonic jerks, cramps and seizures.
- Signs and symptoms of dehydration including dry mouth (dry oral mucosa) and weakness.
- In severe cases when complications develop, hyperosmolarity can occur from water loss. This can lead to neuronal/brain damage including cell shrinkage and brain injury. Dehydration can pull too much water from cells into the blood (increased osmolality). It’s also possible to experience swelling of the brain (cerebral edema). This is a very dangerous response to fluid retention in response to severe dehydration.
- Rhabdomyolysis, which is a complex condition involving the rapid breakdown of skeletal muscle that causes muscle proteins and other muscle constituents to leak outside of cells and into the bloodstream.
- Other complications include cardiovascular and/or circulatory problems, such as abnormal heartbeat rhythms. Rapid or irregular heart beats, or a resting heart rate that exceeds the normal rate may be experienced (called tachycardia) or low blood pressure (hypotension). (7, 8)
- Hypernatremia can be deadly in some cases, especially if the patient is already critically ill or elderly. Studies of hypernatremia patients who were receiving intensive care in the hospital showed mortality rates of 30-48 percent.
Hypernatremia Causes and Risk Factors
In most cases the reason hypernatremia develops is due to impaired thirst (leading to low water or fluid intake), restricted access to water, or increased fluid loss. Hypernatremia only occurs when the thirst mechanism is impaired. This means thirst doesn’t kick in in response to hyperosmolality. There are several reasons this can happen, which are covered more below.
Those who are at the highest risk for developing hypernatremia include:
- The elderly, who are more likely to be admitted to the hospital for various health conditions, to require intravenous fluids, and who may develop changes in digestion, hormone production or thirst signaling due to aging.
- Anyone staying in the hospital in critical care, including requiring ventilation, recovering from a coma, or under sedation. Certain studies have found that patients in critical care have almost double the risk of mortality if they develop hypernatremia than if they do not experience abnormal changes in sodium levels. (9)
- Adults who have kidney damage or acute kidney injury
- Those with a damaged hypothalamus, dementia, diabetes or who have hypothalamic lesions which cause changes in thirst.
- Mentally and physically impaired adults, who sometimes failto drink enough water or perceive thirst.
- Anyone recovering from an acute infection, especially during or after hospitalization. Those at the highest risk are usually people with kidney damage, kidney disease or who are in critical care situations and receiving intravenous fluids. All of these can alter thirst and urination mechanisms. (10)
- Have consumed too much salt/sodium due to use of saline products such as situations in tube feeding, from taking antibiotics containing sodium intravenously, or when receiving other fluids during a hospital stay such as sodium bicarbonate.
- Infants who are breastfeeding. In some cases, inadequate breastfeeding (poor milk supply or an inexperienced mother who isn’t used to nursing) causes infant dehydration. This rarely develops in most cases (less than .05 percent of the time). Neonatal hypernatremia is most likely to affect infants in their first 3 weeks of life. This is especially true if they have lost 10 percent or more of their birth weight. Signs include seizures and abnormal lethargy.
- Those who have been sick with an upset stomach (experiencing vomiting, diarrhea and nausea or example) due to fluid loss.
- Athletes can experience dehydration due to overtraining (especially in hot climates). This can include those who have been excessively sweating such as marathon runners. It also can include people who are underweight who over-exercise without drinking and eating enough.
- People who have eating disorders, such as bulimia nervosa, or who have abused laxatives, diuretic “water pills,” or weight loss pills.
Why & How Hypernatremia Develops:
Intake and excretion of water normally balances levels of sodium in the blood. This includes rising and falling levels of other electrolytes including potassium. So, in order for sodium to rise to dangerously high levels, there must be an abnormal exchange between sodium/water/potassium.
In healthy people without hypernatremia, changes in water intake (drinking water or fluids) along with water excretion (urination) usually maintains normal sodium levels. Without you even knowing it, the body constantly controls these two factors through two primary mechanisms. It controls the amount of salt and water leaving the body through adjusting urinary concentrations (the kidneys and pituitary gland help control this). It also makes you feel thirstier when you’re in need of more water and less salt.
Some of the things that can interfere with this process of sodium-water-balance include: releasing more or less of the antidiuretic hormone called arginine vasopressin (or AVP), loss of normal circulation (a decrease in blood volume flowing through the arteries), in response to infection or pain, due to digestive issues such as nausea, as a side effect of lots of stress or anxiety, and due to taking medications or drugs that change release of AVP.
Several hormones, especially one called aldosterone, control sodium levels. Aldosterone signals the kidneys to increase or decrease the release of sodium depending on someone’s intake of water and salt. Because of this, kidney dysfunction or acute kidney injury can be a major contributor to hypernatremia. Stimulus for AVP secretion happens from activations in the hypothalamus. This is why hypothalamus damage or other problems are also a big hypernatremia risk factor.
Conventional Treatments for Hypernatremia
Treatment for hypernatremia depends on the underlying cause of why it’s happening. Most treatments have the goal of restoring water levels back to normal and reducing sodium intake. According to information provided by American Family Physician, some typical hypernatremia treatments include:
- Stopping loss of water and fluids, such as due to excessive sweating, vomiting, diarrhea, diuretic use, or in response to severe burns.
- Treating injuries that cause fluid loss and abnormal electrolyte changes. These can include heat exhaustion, elevated creatinine levels, or dehydration due to over-exercising without consuming water.
- Correcting any elevated stress hormone levels or glucose levels (such as due to diabetes or other conditions), to reduce the underlying cause and correct the patient’s broken thirst signal.
- Adjusting levels if sodium is increasing due to use of intravenous fluids or other medications while in the hospital
Prevention & 4 Natural Treatments for Hypernatremia
1. Prevent Dehydration & Drink Enough Water
If you’re mostly healthy and don’t suffer from something like diabetes or brain damage, then your thirst signal should be intact enough to prevent hypernatremia from happening. Therefore mild-to-moderate dehydration should not trigger hypernatremia in most people that is severe enough to be treated. That being said, drink enough water and prevent dehydration symptoms to feel your best and reduce risk for complications.
Several important ways to prevent yourself from becoming dehydrated include: not over-using diuretics or weight loss pills; treating the underlying cause of vomiting or diarrhea and being sure to take in enough fluids when it does occur (such as if you’re sick); monitoring symptoms you experience due to taking antibiotics; managing your blood and side effects of diabetes; and keeping an eye on side effects due to taking other pharmacologic agents that you’ve been prescribed.
2. Visit Your Doctor if Dehydration is Chronic
If you suspect another cause of dehydration, talk to your doctor right away about treating the cause of water loss and reversing the water deficit. Your doctor may evaluate you for edema or other conditions. Evaluations will depend on if your hyponatremia symptoms are short-term (acute) versus chronic. Your doctor can then decide how to best restore serum sodium levels back to normal.
Most experts recommend restoring sodium gradually and correcting it by no more than 0.5 mEq/L/hour. This is important to avoid the development of complications like brain swelling. Two ways to possibly reduce sodium include: intranasal or oral desmopressin (DDAVP) and with subcutaneous aqueous vasopressin. If you require treatment to reverse hypernatremia, serum sodium levels and neurologic functions will be monitored frequently to ensure everything is safely returning to its normal level.
3. Eat a Healthy Diet To Prevent Complications
Patients with diabetes (specifically nephrogenic diabetes insipidus) have an increased risk for hypernatremia. If you have diabetes or another chronic condition that affects your sodium, glucose, insulin and water levels, eating a healthy diet is key. Those who are chronically ill are usually advised to eat a low-sodium, low-protein diet. This diet is high in things like fresh vegetables and fruit for electrolytes. Sometimes it’s also necessary to take a thiazide diuretic to prevent fluid retention. According to the Cleveland Clinic, “The diuretic and low-sodium diet act to create a mild volume depletion and therefore result in a reduction in urine output. A decrease in protein intake results in a decrease in obligate renal solute excretion and therefore a decrease in water excretion and urine flow.”
4. Monitor Your Urine & Other Symptoms
Experts recommend that as long as your thirst signal is not impaired for any reason, keep water and sodium levels in balance by not forcing yourself to drink more water than you’re thirsty for. Drink water throughout the day depending on how you feel, while also staying hydrated via eating a healthy, unprocessed diet. It’s also best to drink a good sports drink with electrolytes (not plain water) during long races, marathons or workouts. It’s also good to keep track of how often you’re going to the bathroom (look for a pale yellow color, not clear or very dark).
If you’re avid an exerciser, consider this: the opposite of hypernatremia —hyponatremia, or water intoxication as it’s sometimes called — can also happen. According to the Active website, “One study that was conducted by the medical staff of the Boston Marathon found that an alarmingly high percentage of the finishers of the 2002 Boston marathon had developed hyponatremia — a potentially fatal condition — during the race. Hyponatremia results when the sodium concentration of the blood falls too low due to prolonged sweating combined with excessive fluid consumption. Symptoms include dizziness, muscle cramping, confusion, and stomach bloating.” (11)
Precautions Regarding Hypernatremia
Hypernatremia can be a very serious, even deadly, condition that typically warrants getting professional treatment. If you notice signs of dehydration (weakness, dizziness, nausea, passing out, spasms, etc.) and you’re unsure of the cause, visit your doctor. Always tell your doctor about any side effects you’re experiencing due to medication use. Monitor your symptoms carefully if you’re managing any chronic illness.
Final Thoughts on Hypernatremia
- Too much water loss and/or too much sodium gain characterizes hypernatremia. Reasons this can happen include dehydration, due to conditions like mental impairment or diabetes, as a result of brain injury, or due to kidney disease or damage.
- Symptoms of hypernatremia include fatigue, extreme thirst, weakness, nausea or vomiting and increased urination.
- Visit your doctor if signs of dehydration or hypernatremia persist. Treatments may include restoring normal sodium and water levels, changing your medications, treating brain damage or another injury and changing your diet.



