This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Inflammatory Bowel Disease (+ 7 Natural Ways to Help Relieve IBD Symptoms)
June 5, 2018

Inflammatory bowel disease is chronic inflammation (swelling and irritation) of the gastrointestinal (GI) tract. The two main diseases that fall in this category are Crohn’s disease and ulcerative colitis. Both of these conditions are caused by an abnormal response from your body’s immune system, where your system attacks your own tissue.
Inflammatory bowel disease shares symptoms with many other conditions, such as celiac disease and irritable bowel syndrome (IBS). However, those two diagnoses are not considered inflammatory bowel diseases.
Lifestyle strategies and natural therapies may help relieve symptoms for people with Crohn’s disease and ulcerative colitis. Together with conventional medicine, many people can find relief for their symptoms and even get into remission — time periods without symptoms.
What Is Inflammatory Bowel Disease?
Inflammatory bowel disease (IBD) is used to describe conditions that cause long-term inflammation in the digestive tract. The two main diseases that fall in this category are Crohn’s disease and ulcerative colitis: (1)
- Crohn’s disease involves inflammation throughout the digestive tract, including the large and small intestines. The damage often happens in patches rather than affecting the entire tract. However, it can impact multiple layers of tissue in the intestines.
- Ulcerative colitis impacts just the large intestine, called the colon. The damaged tissue usually affects the entire colon in a continuous stretch, causing colon pain and inflammation of the colon. In most cases it only causes inflammation in the innermost lining of the colon. It can also cause symptoms in the rectum.
Other less common diseases also fall under the umbrella term of inflammatory bowel diseases. These include: (2)
- Microscopic colitis
- Behcet’s disease
- Lymphocyte colitis
- Collagenous colitis
- Diverticulosis-associated colitis
Inflammatory bowel diseases affect about 1.6 million Americans. (3) Unfortunately, there is no cure for IBD. The condition will flare up at times and at other times have no symptoms (remission). However, with treatment, most people can keep the disease under control so that they do not develop complications.
Complications of IBD can include: (2)
- Skin, eye and joint inflammation
- Blood clots
- Medication side effects
- Colon cancer
- Primary sclerosing cholangitis (scarring of the bile ducts that causes liver damage)
Is IBD a disability?
Depending on the severity of your symptoms and the impact of the disease on your ability to work, IBD may qualify as a disability. This may mean you can get disability income from the government. For some people, this can replace income lost by not being able to work full-time or at all. However, you will need the support of your physician and it requires time and paperwork to obtain approval. The Crohn’s and Colitis Foundation of America offers a sample disability appeal letter that you can submit with the support of your doctor. (4)
Signs and Symptoms
Inflammatory bowel disease causes a wide range of symptoms. These may vary by the exact diagnosis and the severity of your disease. In general, inflammatory bowel disease symptoms include: (1, 5)
- Diarrhea for a long period of time
- Belly pain
- Cramping
- Bleeding from the rectum or blood in your stools
- Poor appetite
- Unintended weight loss
- Fatigue or lack of energy
- Fever
- Urgency for bowel movements
For a diagnosis, physicians will look for some key IBD signs, including the location and degree of tissue inflammation. Inflammatory bowel disease diagnosis will be done through endoscopy, colonoscopy and imaging tests, such as MRI, computed tomography (CT) or contrast radiography. Together with blood tests and stool samples, these imaging tests should help you get an accurate diagnosis.
People with inflammatory bowel disease may also have other symptoms or complications specific to their disease. IBD symptoms for people with complicated Crohn’s disease can include: (5)
- Bowel obstruction (swelling that causes a blockage in the bowels, which may need surgery to fix)
- Anal fissures (a tear in the skin of the anus)
- Malnutrition
- Ulcers
- Fistulas (when an ulcer goes through the wall of the intestine)
People with ulcerative colitis may also experience complications. Some of these include: (2, 5)
- Toxic megacolon (when the colon suddenly swells and gets wider)
- Holes in the colon
- Extreme dehydration from excessive diarrhea
- Anemia
- Colon cancer
- Liver disease
- Osteoporosis

Causes and Risk Factors
Although the exact cause of most inflammatory bowel disease is unknown, it is believed to be due to a problem with the immune system. This may be triggered when your body tries to fight off bacteria or a virus in the gastrointestinal tract. Something goes wrong and your immune system doesn’t stop — it keeps attacking healthy tissue.
In some cases, there is a genetic component to IBD. This means you may be more likely to develop IBD if you have certain genes or family members with the condition.
Risk factors for IBD include: (2, 3, 5)
- Age younger than 30 (you can get it at any age though)
- Ashkenazi Jewish heritage
- White race
- Having a close relative with IBD
- Smoking (it is a risk factor for Crohn’s, though it may provide some protection against ulcerative colitis)
- Taking non-steroidal anti-inflammatory drugs (NSAIDs); these also make symptoms worse if you already have IBD
- Living in developed countries or in urban areas
- Living in northern climates
- Higher socioeconomic status
- Diets high in fat or refined foods may also be a risk factor
Some people theorize that IBD has become more common in developed countries due to lack of exposure to germs. However, there doesn’t appear to be any single cause to the condition.
Conventional Treatment
Inflammatory bowel disease treatment depends on the type of underlying disease you have.
Common medical treatments for IBD include: (3)
- Aminosalicylates to reduce inflammation
- Corticosteroids to calm the immune system
- Immunomodulators to keep the immune system from causing inflammation
- Antibiotics to help treat infections and abscesses
- Biologic therapies to target inflammatory proteins and reduce inflammation
- Surgery to remove intestinal blockages, fistulas or abscesses
- Surgery to remove the colon (for people with severe ulcerative colitis)
Typically, a treatment plan starts with the safest medications and works up to the most serious drugs (biologics and immunomodulators) or surgery. Many people with IBD only need to take drugs while they have “flares” — periods of active symptoms. Once the disease signs (checked by blood tests) and symptoms have faded or gone away completely (remission), many people can go off of medication, at least for a while.
Surgery does not cure Crohn’s disease. It basically cures ulcerative colitis but in most cases leaves people with a pouch to collect feces that has to be emptied regularly.
People may also take medications for symptoms. These may include: (6)
- Anti-diarrheal medication
- Dietary supplements for iron, calcium, vitamin D and other nutrients
- Acetaminophen
Natural Ways to Help Manage IBD Symptoms
Although IBD isn’t caused by diet alone, nutrition plays an important role in these diseases and their symptoms. In addition, other natural approaches can help you manage your IBD symptoms and possibly achieve remission or stay in it longer. Consider these natural ways to manage your IBD:
1. Keep a food diary
The impact of diet on the development of IBD is not totally clear. However, what you eat and drink can play an important role in your symptoms. Keeping a food diary is one way to find out what does and does not bother your gut as well as what might help your symptoms.
- Keep a digital or print food diary. (There’s an app for that, yes!) Track what you eat for every meal and snack for several weeks at least. You can either keep a small notebook with you to mark down the info throughout the day or keep it by your bed to fill out every night. Apps make it easy to track the data in your phone and may offer special report features as well.
- Track your symptoms in the diary as well. This means obvious symptoms, such as diarrhea, as well as other symptoms including: headaches, cramping, fatigue, bloating, poor mood and any other changes in how you feel. In addition, make a note of days you feel well. Knowing what you’ve eaten on good health days can be just as valuable as knowing what made you feel poorly.
- Keep track of time. Note when you eat something as well as what time you have other symptoms. This will help you trace the symptoms back to what you ate.
- Bring your diary to an expert. A dietician or health care professional familiar with IBD can help you sort through your diet and symptoms. They can use your diary to figure out what you are eating that soothes or triggers symptoms.
- Use the information to avoid triggers. You can use your diet diary to find a diet plan that works for you. Working with your dietitian or doctor can also help, since they can help you build a diet that is balanced nutritionally while still avoiding your triggers. Common triggers for IBD symptoms include:
- Fiber, such as seeds, nuts and raw vegetables and fruits
- Acidic foods
- Caffeine
- Dairy
- High-fat foods
- Spicy foods
- Vegetables in the cabbage family, including cauliflower
2. Optimize your nutrition
Many people with Crohn’s disease and ulcerative colitis may end up with nutrient problems during flares or when the disease gets serious. Anemia can result from blood loss in diarrhea. Malnutrition can occur in Crohn’s disease when the gut doesn’t absorb nutrients. To help avoid nutrient deficiencies, consider these steps:
- Work with a dietitian. You can get simple blood tests to check for common nutrient deficiencies in IBD. You can also ask for suggestions of IBD-friendly foods and supplements to make sure you get enough nutrition. A nutritionist or registered dietitian may also be able to create a custom plan to help you avoid nutrient deficiencies using your food diary.
- Consider a liquid diet. Some people with severe flares may benefit from liquid diets, which make it very easy for your body to digest and obtain nutrients. They can also help ease pain and may even kick-start a period of remission for some people with Crohn’s disease. A liquid diet should be guided by a physician and nutritionist and can include either store-bought liquid meal replacements or enteral nutrition (a tube into the stomach, for example). Liquid meal replacements may not taste very good, and the diet needs to be followed for at least six weeks in most cases. However, some people have excellent results. (7)
- In children, enteral nutrition is just as good as corticosteroids at jump-starting remission. It is also the preferred method because it is very safe and won’t impact growth. (8)
- Take supplements. Many people with IBD, particularly Crohn’s disease, have trouble digesting food properly and may have nutrient deficiencies. These can cause fatigue and even osteoporosis. The Mayo Clinic suggests multivitamin and mineral supplements may be useful after talking with your doctor. (6) Instead of a multivitamin, supplements for single nutrients may be helpful. The Crohn’s and Colitis Foundation suggests supplements or diets rich in the following nutrients may be helpful:
- Iron — to help fatigue and avoid anemia from blood loss
- Calcium — to help you avoid low bone density and weak bones caused by a lack of calcium, which can happen due to problems absorbing nutrients or when you take steroids
- Vitamin D — this is recommended for everyone with IBD due to its possible role in reducing intestinal inflammation. It is great to take in combination with calcium to support bone health
- Folic acid — this nutrient can be depleted by common IBD medications, and is especially important for women of childbearing age
- Vitamins A, E and K — people with IBD may have trouble avoiding these fat-soluble vitamins
- Vitamin B12 — this is especially important for people on a vegetarian diet or for people who have problems with the ileum, where vitamin B12 is best absorbed
- Zinc — many people with frequent diarrhea can develop a zinc deficiency, so supplements for zinc may be very helpful
- Try ready-made diet guides. Many people with IBD have similar triggers. Some sample diets exist, such as Dr. Axe’s diet for ulcerative colitis. Tips include eating small, frequent meals, getting plenty of fluids, avoiding high-fiber foods and taking specific supplements. Always discuss diet and supplement plans with your health care professional prior to making any major changes.
3. Consider complementary supplements
In addition to supplements your doctor may recommend based on your other medications or your overall health, you may wish to ask about others. Some supplements studied for use in people with IBD include: (9)
- Green tea polyphenols — drinking green tea may reduce inflammation in the intestines, and scientists believe the research on it merits clinical trials in humans for treating IBD
- Resveratrol — studies in animals suggest resveratrol may calm the immune system’s reaction, reduce inflammation and even prevent colitis and colon cancer
- Curcumin or turmeric — early studies show it has anti-inflammatory and antioxidant effects, but more rigorous research is needed before it is considered a treatment for IBD
- Rutin — found in citrus fruits, buckwheat seeds and tea, rutin is a flavonoid that may help reduce inflammation in the colon. So far only animal studies have been done
- Fresh pineapple juice (bromelain) — early research strongly suggests that long-term intake of fresh pineapple juice can calm immune-mediated diseases and inflammation in the colon
- Pomegranate — early studies have found a promising role for pomegranate in the calming of colitis, ulcers and diarrhea
- Fish oil — omega-3 fatty acids from fish oil supplements may reduce inflammation and keep people in remission from IBD symptoms longer
- Aloe vera gel — believed to help speed wound healing and reduce inflammation, but more research is needed in IBD patients
- Wheat grass juice — drinking juice for four weeks reduced rectal bleeding and disease activity in one study with IBD patients, but showed little other impact on IBD
- Germinated barley — this may improve diarrhea symptoms
- Cinnamon extract — in early experiments with animals, cinnamon extract may fight colitis
- Freeze-dried black raspberry powder — because of its potent anti-inflammatory effects, this is being studied for IBD help
- American ginseng — very early research suggests this may reduce the risk of colon cancer-associated colitis
- Ginger extract — because of its anti-inflammatory properties, ginger may be researched further in the field of IBD treatment
4. Minimize stress
The link between stress and IBD is controversial. However, many people with Crohn’s or ulcerative colitis say that flare-ups are more likely to happen when they are in periods of high stress. You can help keep stress in check by:
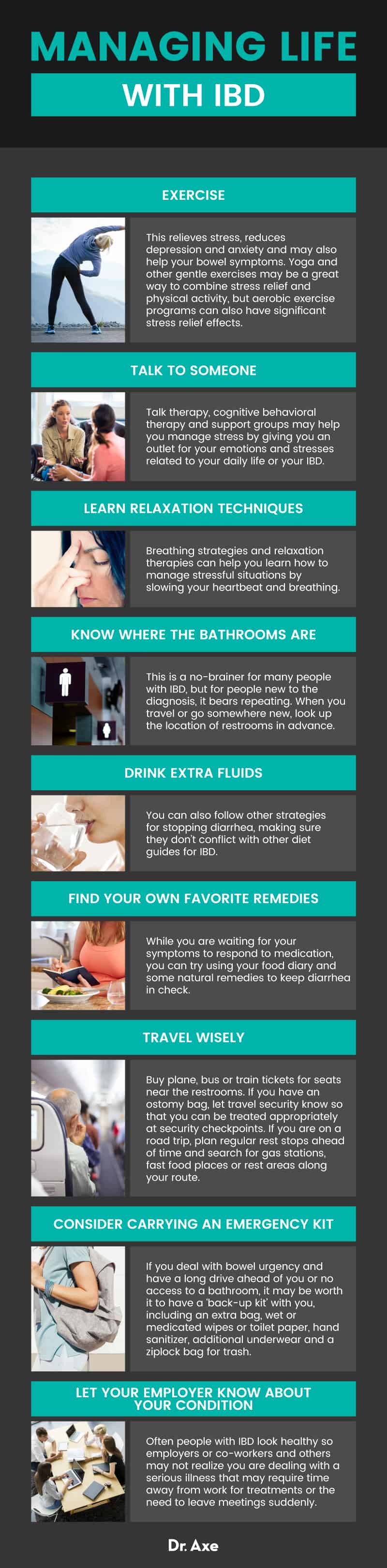
- Exercising. This relieves stress, reduces depression and anxiety and may also help your bowel symptoms. Yoga and other gentle exercises may be a great way to combine stress relief and physical activity, but aerobic exercise programs can also have significant stress relief effects.
- Talking to someone. Talk therapy, cognitive behavioral therapy and support groups may help you manage stress by giving you an outlet for your emotions and stresses related to your daily life or your IBD.
- Learning relaxation techniques. Breathing strategies and relaxation therapies can help you learn how to manage stressful situations by slowing your heartbeat and breathing. Biofeedback is one strategy, but you can find many ways to help manage stress on a daily basis, such as meditation, to keep your stress levels lower.
5. Consider probiotics
Probiotics may help keep a healthy balance of bacteria in the gut. Early research in patients with inflammatory bowel disease suggests that probiotics may help rebalance the immune system’s response to the bacteria in the gut. Probiotics may also reduce inflammation and disease severity. (9)
Prebiotics do not have the same level of evidence yet, although some laboratory research suggests they may help reduce inflammation in IBD. (10)
6. Quit smoking
Smoking and tobacco have different effects depending on your type of inflammatory bowel disease. In Crohn’s disease, smoking makes you more likely to develop the disease. Once you have it, smoking also makes Crohn’s more severe. In ulcerative colitis, however, smoking cigarettes may actually have a protective effect, making symptoms less severe.
Even though smoking may make ulcerative colitis symptoms less severe, most physicians say it is still important to quit smoking — no matter what type of IBD you have. This is because smoking has so many other negative impacts on health, including raising your risk for heart disease and lung cancer. You can try some of Dr. Axe’s tips for quitting smoking.
7. Manage diarrhea
Some of the most common symptoms of inflammatory bowel disease are diarrhea and, at times, bleeding during bowel movements. While this may only happen during flares, it’s important to know how to manage it. Tips for managing diarrhea include:
- Know where the bathrooms are. This is a no-brainer for many people with IBD, but for people new to the diagnosis, it bears repeating. When you travel or go somewhere new, look up the location of restrooms in advance. Try using the restroom before long stretches where it may be difficult to make it to a restroom.
- Drink extra fluids. You can also follow other strategies for stopping diarrhea, making sure they don’t conflict with other diet guides for IBD.
- Find your own favorite remedies. While you are waiting for your symptoms to respond to medication, you can try using your food diary and some natural remedies to keep diarrhea in check.
- Travel wisely. Buy plane, bus or train tickets for seats near the restrooms. If you have an ostomy bag, let travel security know so that you can be treated appropriately at security checkpoints. If you are on a road trip, plan regular rest stops ahead of time and search for gas stations, fast food places or rest areas along your route.
- Consider carrying an emergency kit. If you deal with bowel urgency and have a long drive ahead of you or no access to a bathroom, it may be worth it to have a ‘back-up kit’ with you, including an extra bag, wet or medicated wipes or toilet paper, hand sanitizer, additional underwear and a ziplock bag for trash.
Precautions
- Do not try to self-diagnose or self-treat inflammatory bowel disease. Symptoms of inflammatory bowel disease can be easily confused with many other conditions, including infections, cancer, irritable bowel syndrome (IBS) and celiac disease. Treatment varies for each disease, so it is essential to have a correct diagnosis.
- Inflammatory bowel disease isn’t a fatal condition. However, complications of IBD can be deadly. Work with a health care professional to get appropriate treatment and stick to your follow-up care plan. Regular visits with your medical team can make sure you catch problems early. Notify your doctor if you have a major change in symptoms or a gradual but steady worsening of symptoms. You should also call your doctor if you notice some of the following warning signs of complications:
- Heavy bleeding during or between bowel movements
- Weakness and fatigue beyond what you feel normally
- Extreme cramping or abdominal pain
- Weight loss
- Fever
- Any worsening of your usual IBD symptoms
- In most cases, vitamin and mineral supplements are safe for people with IBD. Regardless, you should always check with your health care provider before adding or changing your supplements, since some supplements can interact with medications.
- Do not stop taking your IBD medication without first discussing the change with a health care professional. If you have side effects or wish to explore other treatment options, talk with your doctor before changing on your own.
Final Thoughts
- Inflammatory bowel disease is an umbrella term for conditions that cause inflammation in the gastrointestinal tract. The most common types of IBD are ulcerative colitis and Crohn’s disease.
- Ulcerative colitis affects the large intestine (colon). It is usually milder than Crohn’s disease but can have serious complications.
- Crohn’s disease affects the entire digestive tract, including the small and large intestines, and usually causes patches of inflammation.
- There is a strong need for finding the best inflammatory bowel disease diet for you. This will depend on identifying triggers and foods that soothe your symptoms and will take trial and error.
- Inflammatory bowel disease cannot truly be cured, but many people with IBD achieve good control of the condition. Most people have long periods of good health (remission) with occasional flares of symptoms. However, medications are often required to achieve and maintain periods of good health.
7 Natural Therapies to Help IBD Symptoms Include:
- Keeping a food diary
- Optimizing your nutrition
- Considering complementary supplements
- Minimizing stress
- Trying probiotics
- Quitting smoking
- Managing diarrhea
Read Next: 9 Candida Symptoms & 3 Steps to Treat Them