This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
5 Natural Remedies for Interstitial Lung Disease
September 21, 2018

Interstitial lung disease (or ILD) is more than one disease; in fact, this term describes more than 200 different lung disorders that all affect the tissues and spaces around the alveoli (air sacs) in the lungs, called the interstitium. (1)
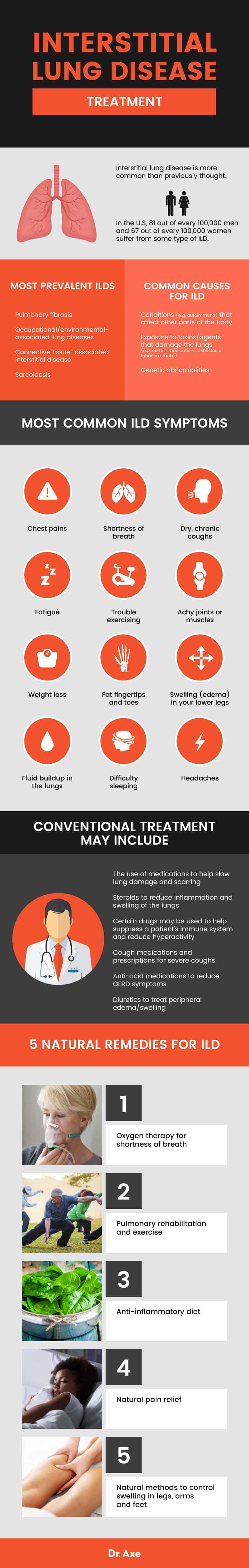
Today, ILD is believed to be more common than previously thought. Research indicates that in the U.S, up to 81 out of every 100,000 men and 67 out of every 100,000 women suffer from some type of interstitial lung disease. The most prevalent interstitial diseases include: pulmonary fibrosis, occupational/environmental-associated lung diseases, connective tissue–associated interstitial disease, and sarcoidosis (the growth of tiny collections of inflammatory cells called granulomas in the lungs).
Can interstitial lung disease be treated? It depends on the specific type of disease that someone has. For some types of ILD, there is no established treatment that has been shown to help, while for other types of ILDs treatment is usually effective. The older someone gets, typically the harder it is to treat ILD. Both incidence of ILD and mortality due to ILD increase with age. While interstitial lung disease can be difficult to manage and live with, treatments including medications, oxygen therapy, physical therapy, exercise, a healthy diet, and essential oils may all be able to help.
What Is Interstitial Lung Disease?
According to the American Lung Association, interstitial lung disease (or ILD for short) is an “umbrella term” for a large group of disorders that cause scarring (or fibrosis) of the lungs. (2) ILDs can affect parts of the lungs including: the alveoli, airways (trachea, bronchi, and bronchioles), interstitium, blood vessels, and pleura (outside lining of the lung).
Depending on the type of ILD someone has, they can develop varying degrees of fibrosis, inflammation, and other symptoms. Fibrosis associated with ILD describes an increased amount and abnormal structure (scarring) of connective tissue, while inflammation describes the excessive formation of inflammatory cells. If the lungs become damaged due to ILD, this can sometimes be permanent and progressive, meaning it can’t be reversed and get’s worse over time.
What are the different types of interstitial lung disease? Some specific ILD types include:
- Pulmonary fibrosis (IPF), when the small air sacs of the lungs called alveoli are hardened, scarred and damaged due to disruption from external particles.
- Idiopathic pulmonary fibrosis, which has no known cause.
- Interstitial pneumonitis (or hypersensitivity pneumonitis), in which the lungs become inflamed. This is often associated with an allergic reaction or autoimmune conditions (such as rheumatoid arthritis scleroderma or fibromyalgia).
- Sarcoidosis, inflammation of the lungs and usually swollen lymph nodes.
- Pulmonary hemorrhage, which describes acute bleeding from the lungs from the upper respiratory tract, trachea and alveoli.
- Connective tissue diseases.
- Occupational/environmental-associated ILD, including asbestosis, Black lung disease among coal miners, Farmer’s lung from inhaling farm dust, siderosis from inhaling iron from mines or welding fumes, and silicosis from inhaling silica dust. (3)
- Drug/radiation induced ILD.
Is emphysema the same thing as interstitial lung disease? While the two have symptoms in common, they are not the same thing. Emphysema is considered a type of chronic obstructive pulmonary disease (COPD). COPD is another umbrella term that includes over 100 different but related diseases, including emphysema and chronic bronchitis. COPD is different from ILD because it describes obstructive lung diseases that mostly affect the ability to breathe due to tightening of the airways, while ILD is mostly due to scarring and fibrosis that restricts the ability to breath. (4)
Symptoms and Signs
Interstitial lung disease symptoms vary depending on the specific type of disease that has someone has. Symptoms are caused by four main types of abnormalities that characterize interstitial lung diseases:
1. Respiratory symptoms, such as shortness of breath.
2. Those caused by chest abnormalities.
3. Those caused by changes in pulmonary function, including decreased lung volume.
4. Those caused by microscopic patterns of inflammation and fibrosis.
The most common interstitial lung disease symptoms include: (5)
- Chest pains
- Trouble breathing and shortness of breath
- Dry, chronic coughs
- Feeling fatigued, lethargic and weak
- Trouble exercising
- Achy joints or muscles
- Unintended weight loss
- Fingertips and toes that get wider and rounder at the ends (clubbing)
- Swelling (edema) in your lower legs
- Fluid buildup in the lungs (pulmonary edema.), caused by fluids and water collecting in the air sacs of the lungs
- Difficulty sleeping
- Headaches
- Depending on underlying causes of ILD, you might develop a fever or signs of an allergic reaction
What are the symptoms of end stage lung disease? In other words, how do you know if your disease may be advanced? Symptoms of advanced ILD can include: (6)
- Breathlessness/shortness of breath
- Ongoing fatigue
- Fast, rapid breathing
- Confusion due to high levels of carbon dioxide in your bloodstream
Causes and Risk Factors
The causes of interstitial lung disease are classified into four categories:
1. ILDs caused by conditions that affect other parts of the body (for example, autoimmune diseases that affect the blood vessels or collagen that forms connective tissue).
2. ILDs caused by exposure to toxins/agents that damage the lungs (for example, certain medications, asbestos, or tobacco smoke).
3. ILDs caused by genetic abnormalities.
4. Idiopathic ILDs that usually have no known cause. This is the most common type of interstitial lung disease.
In the case of pulmonary fibrosis (the most common ILD) the cause is the development of scar tissue in the lungs, which builds up and blocks oxygen from passing from your lungs into the blood. (7) Not having enough oxygen in the blood leads to symptoms like shortness of breath, and feeling tired and weak.
Interstitial lung disease most often affects adults, although children can sometimes be affected too, usually if they have a family history of ILD in close relatives. Different types of ILD tend to develop in adults of different ages. For example, sarcoidosis, pulmonary Langerhans cell histiocytosis, and autoimmune-associated lung diseases most often develop in young adults, while idiopathic pulmonary fibrosis (IPF) most often develops in adults between the ages of 40 and 70.
Risk factors for interstitial lung disease include:
- Genetics and family history of ILD, especially having 2 or more close relatives who suffer from ILD.
- Having an autoimmune disease.
- Exposure to toxic agents, such as asbestos, silica, metal/wood dusts, and antigens. Current and former farmers, miners, and construction workers are at an increased risk due to exposure to certain pollutants that can harm the lungs.
- Smoking cigarettes and using tobacco products.
- Having allergic reactions/hypersensitivity to things like dust, fungus, molds or chemicals.
- Being born with a genetic abnormality that affects the lungs.
- Taking certain prescription drugs, such as those used to treat chronic GERD (gastroesophageal reflux disease), irregular heart rhythm, some antibiotics, radiation and chemotherapy, and certain prescription anti-inflammatory drugs.
- History of cancer and having had received radiation to the chest or certain chemotherapy drugs.
- History of tuberculosis, pneumonia, and certain viral infections that may damage the lungs. Mycoplasma pneumoniae (also commonly referred to as “walking pneumonia”), which describes bacteria that live in your respiratory system, is another potential cause of lung infections and damage.
- Being a male between the ages of 40-70 years old.
- Being caucasian. Some studies have found that in the U.S, caucasians are more likely to be diagnosed with certain types of ILD (such as pulmonary fibrosis) and have higher mortality rates compared to African Americans.
Diagnosis and Prognosis
How do you diagnose interstitial lung disease? ILD is usually diagnosed using a combination of: blood tests, breathing tests, a chest X-ray and high-resolution CT (HRCT) scan of your chest, and a stress test or exercise test to determine how the lungs functioning. Some patients will also need a lung biopsy, especially if other tests suggest the patient is dealing with ILD. (8)
What is the life expectancy of a person with interstitial lung disease? In terms of prognosis, someone with interstitial lung disease has a better chance of recovering if a lung biopsy shows predominately high levels of inflammation, but not a very advanced stage of fibrosis. If a biopsy indicates that someone has a predominance of fibrosis, this usually means that the disease is more advanced and more difficult to treat. Those with a predominance of inflammation typically have a better prognosis and response to treatment.
Sadly, studies suggest that both incidence rates and mortality rates for ILDs like idiopathic pulmonary fibrosis are rising in many countries, including the United States and United Kingdom. And mortality rates from idiopathic pulmonary fibrosis are expected to keep increasing because there is no established treatment that has been shown to help cure the disease or prolong life expectancy.
Sarcoidosis usually has a better prognosis than IPF. The reversal of sarcoidosis is high in most cases, while unfortunately the median survival of those with IPF is two to three years. About 77 percent of people with pulmonary fibrosis die from breathing-related complications, and others pass away due to related causes such as cancer, heart attacks, strokes, accidents or illness.
Conventional Treatment
Interstitial lung disease treatment can involve: (9, 10)
- The use of medications to help slow lung damage and scarring. The FDA has approved medications called nintedanib (Ofev®) and pirfenidone (Esbriet®) for treatment of idiopathic pulmonary fibrosis (IPF). These medications are called anti-fibrotic agents.
- Steroids, also known as glucocorticoids or corticosteroids, are also sometimes used to reduce inflammation and swelling of the lungs.
- Certain drugs may be used to help suppress a patient’s immune system and reduce hyperactivity, including azathioprine, cyclophosphamide and mycophenolate mofetil (Cellcept®, Myfortic®). These are sometimes with combined with high-doses of antioxidants, such as N-acetyl cysteine.
- Cough medications, including over-the-counter products like Robitusson® and cough drops, prescriptions like hydrocodone (Tussionex PennKenetic®) and benzonatate (Tessalon Perles®),or Thalidomide (Thalomid®) for severe coughs.
- Anti-acid medications (for example, Proton pump inhibitors including Prilosec OTC® and Nexium®, or H2-Blockers including Zantac® and Pepcid®) can be used to reduce GERD symptoms by blocking the formation of acid in the stomach.
- Diuretics (like Lasix) may be prescribed in order to treat peripheral edema/swelling.
- If the disease has progressed and become advanced, lung transplant may be needed to prolong survival. This is usually done in patients younger than 65 without other significant medical conditions. Studies suggest that the five-year survival rate in patients who undergo lung transplant is approximately 40 percent and the median survival is 3.9 years.
5 Natural Remedies for Interstitial Lung Disease Symptoms
1. Oxygen Therapy
Oxygen therapy is primarily used to reduce complications associated with low blood oxygen levels, including shortness of breath and trouble exercising. It can help make breathing and physical activity easier, improve sleep, and reduce blood pressure in the right side of the heart. (11) Some people only use oxygen while they sleep or exercise, while others use it all day to control symptoms.
Talk to your doctor about using a pulse oximeter at home, which is a small device placed over your fingertip that tells you how much oxygen is in your blood and if you require more.
2. Pulmonary Rehabilitation and Exercise
“Pulmonary rehabilitation” includes a number of therapy approaches that can help improve daily functioning and well-being among people with interstitial lung disease. Pulmonary rehabilitation may include: physical therapy, an exercise program that is safe and appropriate (usually including both aerobic and strength training), occupational therapy to make every activities easier, nutritional support, emotional support, and breathing exercises that can improve lung efficiency. (12)
Staying active, such as by working with a physical therapist or personal trainer who is familiar with lung diseases, is important for supporting the lungs, cardiovascular system and immune system. Inactivity can make shortness of breath, stiffness, swelling and pain worse. Talk to your doctor about safe ways to stay active, such as walking outdoors, swimming, cycling or doing yoga and Tai Chi. Aim for 20–30 minutes of moderate exercise (think a brisk walk or a slow jog) every day if possible.
3. Anti-Inflammatory Diet
If you’re suffering from ILD, it’s a good idea to meet with a dietician or nutritional counselor for help customizing a healthy diet. If you’re experiencing weight loss due to loss of appetite, it’s important to make sure you’re consuming enough calories to support your needs and prevent nutrient deficiencies. You should also speak with your nutritionist or doctor about any supplements and medications you take to make sure they aren’t worsening symptoms such as changes in blood pressure or GERD.
The Lung Institute recommends that people with interstitial lung disease eat a healthy, balanced diet that includes: (13)
- A variety of vegetables and fruits to maximize antioxidant, vitamin, mineral and fiber intake. Some of the best choices include: all types of leafy greens, sweet potatoes, broccoli and other cruciferous veggies, carrots, tomatoes, squash, garlic, herbs and spices, citrus, mangos, cherries, melon, all types of berries, cocoa, green tea and sea vegetables. Organic foods are best to help decrease exposure to pesticides and chemicals.
- Plenty of lean protein, such as fish, grass-fed meat, pastured eggs and poultry.
- Wild-caught fish like salmon or sardines that provide omega-3 fatty acids.
- Probiotic foods, including yogurt, kefir and cultured veggies.
- Stay hydrated, particularly with water, fresh vegetable juices and herbal teas/infusions.
- Avoid refined and processed foods, including fried foods, fast food, and those made with refined grains, added sugar and hydrogenated fats.
- I also recommend that if you have an autoimmune disease or allergies, consider trying an elimination diet and avoiding common allergens like gluten, dairy, peanuts and shellfish.
4. Natural Pain Relief
Your doctor might recommend that you take an over-the-counter pain killer if pain and swelling become worse. You can also try using natural painkillers like cold packs, essential oils and a humidifier to improve lung and respiratory function.
- Get plenty to sleep, which supports your immune system and helps manage stress.
- To help reduce persistent coughs, consider using a humidifier in your home so you breathe in moist, warm air. This helps to soothe your airways, calm a sore throat, and improve lung function.
- Stay hydrated. Your lungs are 83 percent water! Drink lots of fluids to prevent coughs, dehydration associated with fevers, and and GI issues.
- Apply a cool compress or ice pack wrapped in a towel to your head or chest if you’re dealing with fever, nausea or pain.
- Consider applying essential oils topically, like eucalyptus or peppermint, to your chest, temples, neck and throat. The vapors can help relieve headaches, open your airways and reduce a lingering cough.
Another approach to dealing with chronic pain and discomfort is seeking out emotional support and/or therapy. A therapist can teach patients with interstitial lung disease breathing and mindfulness/meditation techniques that can help them manage stress and feel more relaxed. Muscle relaxation techniques can come in handy during periods of anxiety or stress that may lead to shortness of breath. It can also be helpful to join a support group and talk with others going through the same thing. Supports groups are beneficial for learning new ways to deal with symptoms, feeling less alone, lifting your spirits, and helping you cope with stress or depression.
5. Help with Controlling Swelling (Edema)
If you experience peripheral edema in your legs, arms and feet, these steps may be able to help reduce discomfort:
- Reduce consumption of high sodium foods, like table salt, soy sauce, olives, ham, salami and bacon. Many processed and packaged foods are also high in sodium. Stick to eating fresh produce, lean protein and healthy fats instead.
- Exercise, stretch, stand and stay active throughout the day. Aim to get up and move around at least 5–8 times per day, even if it’s just for 10 minutes. Try to avoid too much sitting so that your blood can continue to flow properly.
- Try natural diuretics like parsley and dandelion tea. One of the best ways to use parsley as a natural and safe diuretic is to make parsley tea. You can do this by adding a quarter cup of chopped parsley to one cup of boiling water. Let the tea steep for about 5 minutes. Strain the parsley leaves and add a teaspoon of honey.
- Use grapefruit essential oil and fennel essential oil. Just add 1–2 drops of either essential oil to warm water or a cup of herbal tea (like chamomile). Or combine 3–4 drops of fennel with 1 teaspoon of any carrier oil and massage the mixture into the affected area.
- Try massage therapy, yoga or acupuncture to promote blood flow.
- To reduce water retention in your legs, try to elevate the affected area a few times a day for about 20 minutes in order to relieve pressure.
Interstitial Lung Disease Prevention Tips
- Get treatment for any known autoimmune disorders, which may involve making lifestyle and dietary changes and/or taking medications.
- Avoid exposure to agents that can cause hypersensitivity and allergies, such as dust and mold.
- Avoid exposure to toxic agents like asbestos and pesticides.
- Quit smoking. You can speak with your doctor or therapist about options for quitting, including smoking cessation programs or relaxation techniques.
- Exercise to help strengthen the lungs and immune system.
- Get treatment for gastroesophageal reflux disease (GERD).
- Take steps to reduce lung infections, such as practicing food hygiene and avoiding being around people who are sick. You can also discuss the benefits of vaccines for respiratory infections including pneumonia that can worsen symptoms of interstitial lung disease.
- Eat a nutrient-dense diet to keep inflammation levels low.
- Maintain a healthy weight.
- Keep stress and anxiety under control.
- Get enough sleep and rest.
Precautions
The earlier that ILD is treated, the better. Don’t put off getting evaluated or receiving treatment if needed. Get help from your doctor right away if you have any of the following symptoms, especially if you’re at an increased risk for ILD:
- Chronic coughing and shortness of breath.
- High blood pressure in your lungs, also called pulmonary hypertension.
- Lung complications, such as blood clots, lung infections or even a collapsed lung.
- Symptoms associated with lung cancer.
- Unusual side effects from treatments and medications.
- Signs of respiratory failure, or a lack of enough oxygen in the blood.
Final Thoughts
- Interstitial lung disease (or ILD for short) is an “umbrella term” for more than 200 disorders that cause scarring (or fibrosis) of the lungs. ILDs can affect parts of the lungs including: the alveoli, airways (trachea, bronchi, and bronchioles), interstitium, blood vessels, and pleura (outside lining of the lung).
- Signs and symptoms of ILD can include: trouble breathing, fatigue, coughs, muscle weakness and aches, fever, loss of appetite, and headaches.
- ILDs can be caused by autoimmune diseases, lung infections or viruses, genetic abnormalities, smoking and exposure to toxins.
- Five natural ways to help manage interstitial lung disease symptoms include oxygen therapy, pulmonary rehabilitation, including exercise and physical therapy, eating a healthy diet, managing pain naturally with a humidifier, essential oils and cool compresses and controlling edema and swelling with dietary changes, elevation, essential oils and natural diuretics.



