This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
The Importance of Pap Smear Screening in the Fight Against Cervical Cancer
November 7, 2016

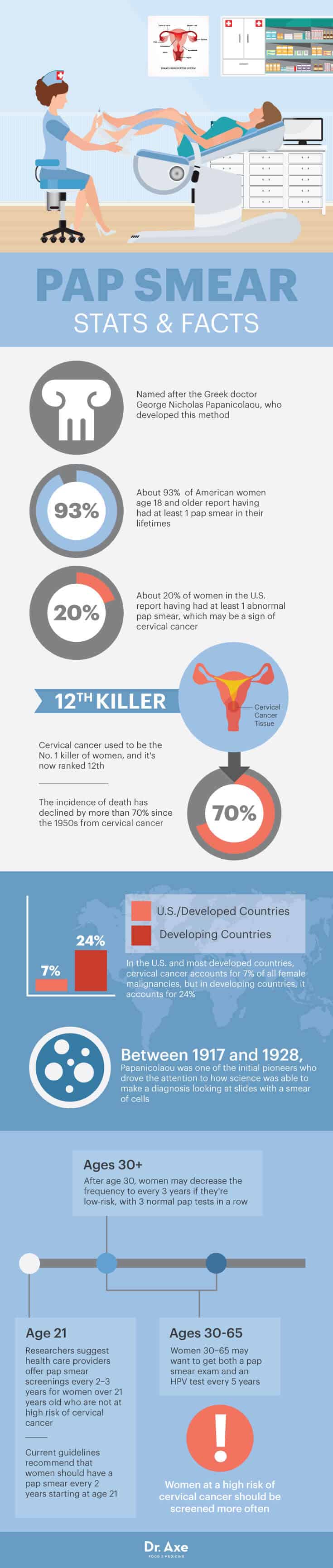
The vast majority (93 percent) of American women age 18 and older report having had at least one pap smear in their lifetimes. And according to a study published in the Journal of General Internal Medicine, 20 percent of women in the United States report having had at least one abnormal pap smear, which may be a sign of cervical cancer. (1)
Screening for cervical cancer remains an important health and economic concern in the United States and throughout the world. The effectiveness of pap smear screenings in reducing cervical cancer mortality is almost universally accepted, as the incidence of death has declined by more than 70 percent since the 1950s. This is largely due to the widespread implementation of screening programs, which has become a top global health care priority. (2)
What Is a Pap Smear?
A pap smear, also known as the Papanicolaou test, is a procedure in which cells are scraped from the cervix and examined under a microscope. The test is used to detect any cell abnormalities that may serve as a sign of cervical cancer or other conditions, such as infection and inflammation. A pap smear screening is the best tool to detect precancerous conditions and small, hidden tumors that may lead to cervical cancer.
The pap smear is named after the Greek doctor George Nicholas Papanicolaou, who developed this method. In the period between 1917 and 1928, Papanicolaou was one of the initial pioneers who drove the attention to how science was able to make a diagnosis looking at slides with a smear of cells. Several studies indicate that rates of cancer death due to cervical cancer dropped tremendously after the 1950s when the pap smear screening programs started. (3)
When performing a pap smear, the gynecologist inserts a speculum into the woman’s vagina so she is able to widen the opening and exam the cervix and vagina. The doctor then takes samples of the cervical cells using a small spatula or brush. The samples are taken from the opening of the cervix, which extends into the vagina, and from the cervical canal, which is deeper inside the womb. The cells then are placed into a solution, transferred onto a small glass slide and sent to the laboratory for a procedure called a cytological examination. (4)
The cytological examination evaluates the formation, structure and function of cells under a microscope. If the cells appear to be abnormal, further testing is needed in order to determine the seriousness of the abnormalities.
Pap Smear Guidelines
In 2004, a group of researchers collected data on the frequency of cervical cancer screening in the United States. These researchers found that among women with no history of abnormal smears, 55 percent underwent a pap smear exam annually, 17 percent went every two years, 16 percent went every three years and 11 percent were not screened regularly. They found that even the elderly reported frequent screening, with 38 percent of women age 75–84 and 20 percent of women age 85 and older reported annual pap smears. Overall, 20 percent of women reported having at least one abnormal exam, and among these women, rates of frequent pap smear screenings are considerably higher at 80 percent. Based on their findings, researchers suggest that health care providers offer pap smear screenings every two or three years for women over 21 years old who are not at high risk of cervical cancer. (5)
Current guidelines from the American Society of Obstetricians and Gynecologists recommend that women should have a pap smear every two years starting at the age of 21. After age 30, women may decrease the frequency to every three years if they’re low-risk, with three normal pap tests in a row. The American Cancer Society suggests that women between the ages of 30–65 could get both a pap smear exam and an HPV test every five years. Women who are at a high risk of cervical cancer because of a suppressed immune system, which may be due to an infection, organ transplant or long-term steroid use, should be screened more often.
The American Cancer Society also suggests that women over 65 years of age who have had regular screenings in the previous 10 years and haven’t had any serious pre-cancers found in the last 20 years should stop cervical cancer screening. Women who have had a total hysterectomy should also stop pap tests, unless the hysterectomy was done as a treatment for cervical pre-cancer. (6)
Benefits of a Pap Smear
The main benefit of a pap smear test is that it serves as a screening for cervical cancer and has saved the lives of many women. Cervical cancer occurs when cervical cells become abnormal and grow out of control over time. The cancer cells invade deeper into the cervical tissue, and in advanced cases the cancer cells can spread to other organs of the body.
According to research published in Obstetrics and Gynecology Clinics of North America in 2009, cervical cancer incidence and mortality in the United States has declined significantly since the 1950s by more than 70 percent. This decline is mainly attributed to the introduction of the pap test in the 1940s. Cervical cancer used to be the No. 1 killer of women, and it’s now ranked 12th. Researchers found that in the United States and most developed countries, cervical cancer accounts for 7 percent of all female malignancies, but in developing countries, it accounts for 24 percent. This disparity is primarily attributed to the lack of screening and treatment of pre-cancerous lesions. (7)
A 1994 study published in the International Journal of Gynecology and Obstetrics evaluated the effectiveness of the pap smear screening program in terms of reduction of mortality from cervical cancer. A analysis gave a calculated 53 percent reduction in cervical cancer mortality that’s attributable to screening, supporting the hypothesis that pap smear screenings have had an important impact. (8)
What to Do If Your Pap Is Abnormal
Abnormal pap smear tests do not mean that you have cancer, but an abnormal test does mean that the cells of the cervix do not look normal. Because a pap test is a screening test and not a diagnostic test, it cannot tell for certain that cancer is present. An abnormal test may be due to inflammation or minor cell changes, which is also called dysplasia. Before cancer cells form in tissues of the body, the cells go through abnormal changes — this is dysplasia. In dysplasia, the cells look abnormal under a microscope, but they’re not cancerous and may never become cancer. Other causes of an abnormal pap smear test are related to using a diaphragm, engaging in sexual intercourse or having cellular changes related to the menstrual cycle.
Most non-cancerous issues detected in a pap smear tend to clear up or go back to normal on their own. If your doctor notices minor or moderate abnormalities, she will probably recommend that you have a follow-up test within a few months. If the abnormal cells have not disappeared after a longer period of waiting, or if they have progressed, then more examinations will be needed.
The human papillomavirus (HPV) test detects the presence of the human papillomavirus, which can lead to the development of genital herpes, abnormal cervical cells or cervical cancer. After receiving an abnormal pap smear, your doctor might recommend the HPV test to see if the virus is causing cellular changes. Most cases of cervical cancer are caused by infection with HPV, which is passed from person to person during sexual activity. Most HPV infections go away on their own and only cause mild changes in cervical cells, but in some women, HPV does not go away and can cause severe changes in cervical cells. Research published in Clinical Microbiology Reviews suggests that the improvements in pap smear screening as well as the introduction of HPV testing greatly facilitate the identification of women at risk for cervical cancer. (9)
If a pap smear exam and HPV test show abnormal cells, you may need to have a test called colposcopy. During a colposcopy, the doctor examines the cervix with an instrument that has magnifying lenses (called a colposcope). The doctor applies a weak solution of acetic acid to the cervix so the abnormal areas are easier to see. If an abnormal area is seen on the cervix, a biopsy will be done, which involves taking a small piece of tissue from the area. A biopsy is the only way to tell for sure that an abnormal area is pre-cancerous, cancerous or neither. (10)
If pre-cancerous cell changes are found, the abnormal tissue can usually be removed completely and the tumor will stop developing. The reason why pap smears are done so regularly is because cervical cancer takes many years to develop and stopping cell abnormalities when they’re just beginning allows doctors to deal with the issue before it becomes more serious.
Precautions About a Pap Smear
Cervical screening results are not always accurate, and sometimes the results show abnormal cells when the cells are actually normal or they may not detect abnormal cells when they’re present. Some factors that may cause a false-negative result include having a small number of abnormal cells, having an inadequate collection of cells during the exam or having inflammatory cells obscuring the abnormal cells. To get the most accurate results from a pap smear, avoid sexual intercourse, douching or using vaginal creams for 48 hours before the test. You should also avoid cervical cancer screenings when you have your menstrual period.
Unfortunately, receiving an abnormal pap smear can be stressful and nerve-wracking experience. Research has found that there is a psychosocial burden among women who receive abnormal pap smear results. A 2009 study conducted in Thailand evaluated 75 women negative for abnormal cell growth and 76 women with abnormal cell growth. Researchers found that the women with abnormal results were concerned about issues such as getting cancer, the pain during the visit to the gynecologist and that having sex with their partners may give them infections. (11)
If you do have an abnormal screening, talk to your health care provider about other available tests in order to determine your treatment plan. For many women, the cervical cell changes go back to normal on their own, and if they don’t, it often takes several years for even high-grade changes to become cancer.
Final Thoughts
- Screening for cervical cancer remains an important health and economic concern in the United States and throughout the world. The effectiveness of pap smear screenings in reducing cervical cancer mortality is almost universally accepted.
- A pap smear, also known as the Papanicolaou test, is a procedure in which cells are scraped from the cervix and examined under a microscope. The test is used to detect any cell abnormalities that may serve as a sign of cervical cancer or other conditions, such as infection and inflammation.
- Women should have a pap smear every two years starting at the age of 21. After age 30, women may decrease the frequency to every three years if they’re low-risk, or they can have a pap smear and HPV test every five years. Women over 65 years of age who have had regular screenings in the previous 10 years and haven’t had any serious pre-cancers found in the last 20 years should stop cervical cancer screening.
- Research shows that cervical cancer incidence and mortality in the United States has declined significantly since the 1950s by more than 70 percent. This decline is mainly attributed to the introduction of the pap test in the 1940s.
- Abnormal pap smear tests do not mean that you have cancer, but it does mean that the cells of the cervix do not look normal.
- Most non-cancerous issues detected in a pap smear tend to clear up or go back to normal on their own. If your doctor notices minor or moderate abnormalities, she will probably recommend that you have a follow-up test within a few months.



