This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Stress Fracture Symptoms & How to Speed Up Recovery
February 19, 2016
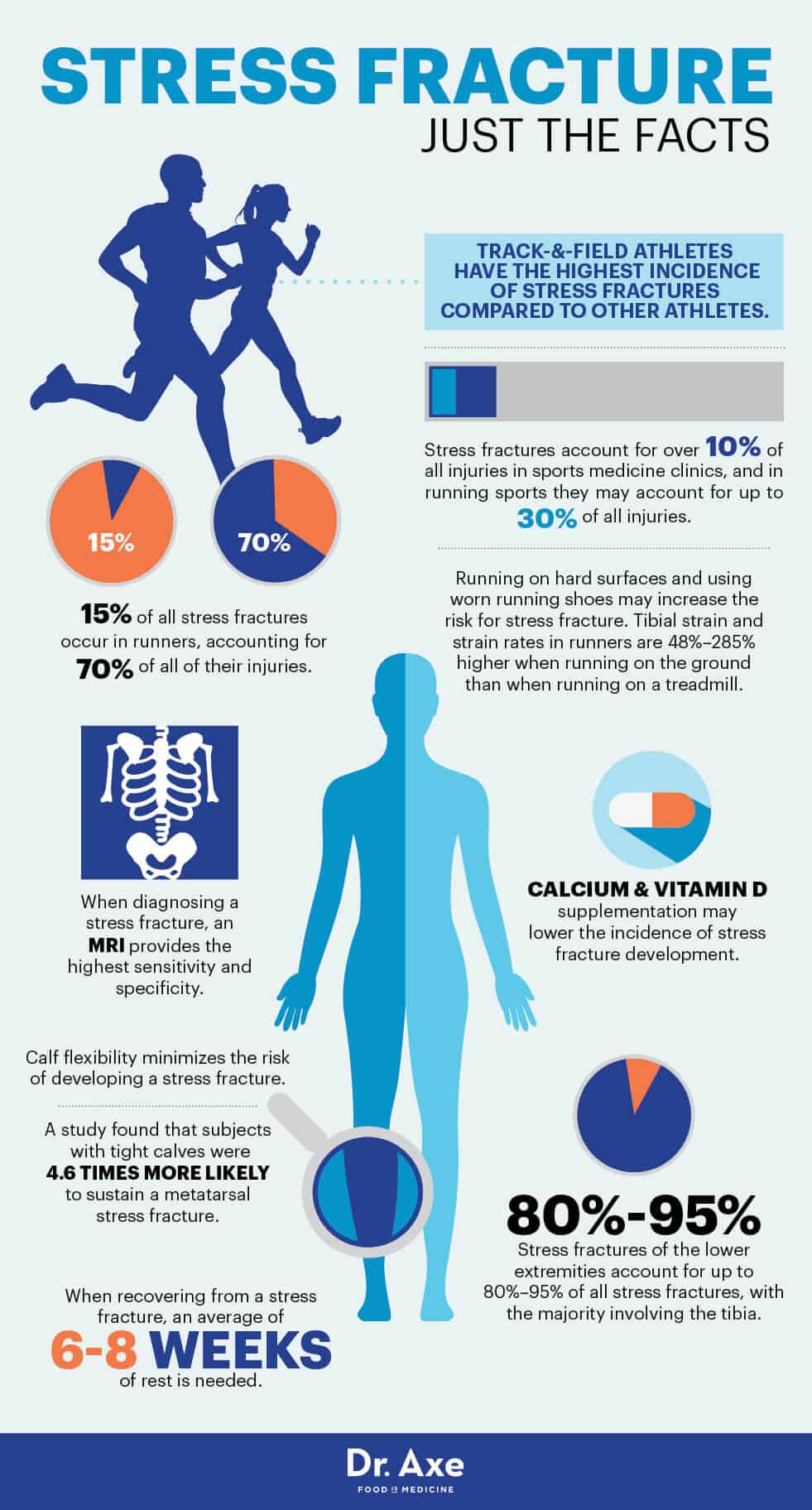
Stress fractures account for over 10 percent of all injuries in sports medicine clinics, and they’re some of the most common running injuries there are. In fact, in running sports they may account for up to 30 percent of all injuries. That’s because our bones endure stress whenever a force is loaded upon it, whether the stress comes from the pull of a muscle or the shock of a leg or foot contacting the ground, there is stress put on the load-bearing bone. Eventually, that stress can lead to a stress fracture.
A stress fracture occurs when muscles become fatigued and can’t handle added shock. The fatigued muscle eventually transfers the stress to the bone, which causes tiny cracks or stress fractures. The repeated stress is lower than the stress required to fracture the bone in a single event, but over time it will do damage. The pain is similar shin splints or a heel spur and oftentimes can even be confused for them at first, but a stress fracture is even more common and more problematic if left untreated.
Did you know that a bone continuously remodels itself to withstand the stress involved with physical activity? But stress fractures occur with increased remodeling, causing a weakening of the outer surface of the bone. That’s why it’s important to increase training intensity gradually, instead of increasing mileage or weight before the bone has a chance to rest and repair. If you take some precautions, you can avoid a stress fracture, and that’s key because a stress fracture keeps you on the couch for six to eight weeks while you wait for your bones to recover.
8 Ways to Avoid a Stress Fracture
1. Intensify Training Slowly
Don’t make drastic changes in milage or intensity when training. When you increase intensity, your bone is actually weaker for about a month after the change before it becomes stronger. Therefore, you need to gradually intensify your training or workouts so your bones can properly adapt to the added stress.
Shoot for no more than a 10 percent increase in load per week in order to strengthen your muscles and avoid overtraining. If you’re new to running, read up on running tips for beginners in order to avoid an injury.
This theory is supported by evidence that military recruits are most likely to endure a stress fracture during their first weeks of service. Recruits for the German Armed Forces in the years from 1998–2000 participated in a study examining stress fracture rates. In the study, 191 cases with 204 fractures were analyzed, and more than 50 percent of the fractures occurred within the first eight weeks of service. The soldiers were exempted from duty for an average of 26.5 days in order to recover fully. (1)
2. Work on Calf Flexibility
Studies show that a common cause of stress fractures is calf tightness, which causes a premature lifting of the heel while running and transfers a significant amount of force into the forefoot. A study published in the Journal of Orthopedic and Sports Physical Therapy found that subjects with tight calves were 4.6 times more likely to sustain a metatarsal stress fracture. (2)
This shows the importance of stretching to loosen muscles, particularly in the calves. It’s also why it’s important to allow for proper muscle recovery so your muscles don’t stay tight all the time and increase the risk of a stress fracture.
3. Allow Your Bones to Heal Completely After an Injury
A premature return to full activity may increase the risk of complications when treating injuries. If you already have a stress fracture, have an MRI before returning to training. If the fracture is not healed completely, you increase your risk of delayed healing. (3)
4. Consume Dairy Products
A two-year study conducted at the Clinical Research Center at Helen Hayes Hospital in New York worked to identify the nutrients, foods and dietary patterns that are associated with stress fracture risk and changes in bone density among young female distance runners. In the study, 125 female competitive distance runners ages 18–26 participated in the study. Their bone mineral density and content of the spine, hip and total body were measured annually, and stress fractures were recorded on monthly calendars. Seventeen participants had at least one stress fracture during follow-up.
Researchers found that higher intakes of calcium, skim milk and dairy products were associated with lower rates of stress fracture. Each additional cup of skim milk consumed per day was associated with a 62 percent reduction in stress fracture incidence, and a dietary pattern of high dairy and low fat intake was associated with a 68 percent reduction. Researchers concluded that higher intakes of skim milk, dairy foods, calcium-rich foods, animal protein and potassium were associated with significant gains in whole-body bone mineral density and bone mineral content. (4)
5. Increase Calcium and Vitamin D Intake
Researchers at the Creighton University Osteoporosis Research Center in Nebraska recruited 5,201 female Navy recruit volunteers and randomized them to 2,000 milligrams calcium and 800 international units vitamin D or placebo. Of the 309 subjects that were eventually diagnosed with a stress fracture, researchers found that the calcium and vitamin D group had a 20 percent lower incidence than the control group. (5)
That means consuming more vitamin D-rich foods, along with calcium foods, can help strengthen bones and decrease the risk of sustaining a stress fracture.
6. Avoid Using Nonsteroidal Medications
There is an increasing amount of literature that suggests that nonsteroidal anti-inflammatory drugs (NSAIDs) may be harmful when used to treat a stress fracture. Nonsteroidal medications have been shown to interfere with bone remodeling and inhibit tendon repair following a sports injury.
A critical analysis published in the Scientific World Journal found that regular use of nonsteroidal medications was associated with an increased relative risk of non-vertebral fractures compared with patients who did receive NSAIDS. Researchers concluded that clinicians should treat NSAIDs as a risk factor for bone healing impairment, and their administration should be avoided in high-risk patients. (6) Further shows that there is a marked association between patients with nonunion of femoral fractures and the use of NSAIDS. (7)
7. Avoid Running on Hard Surfaces
Running or training on a hard surface can lead to increased stress on the muscles and bones. For instance, when a tennis player switches from a soft surface court to a hard court, she increases her risk of developing a fracture. Studies show that people are less likely to develop a stress fracture when running on a treadmill than when running on concrete or hard, outdoor surfaces. If you run or engage in physical activity outdoors, be mindful of the stress being placed on your bones, and lower the intensity. (8)
8. Wear Proper Running Shoes
It’s important that you use proper running shoes with support in order to avoid a stress fracture. If you’re unsure what kind of shoes are best for you, ask for help at your local sneaker store.
The best shoe depends on the shape of your feet; you may have flat, neutral or high arches. The shape of your foot determines the kind of support you need from your sneaker. If you’re flat-footed, you need a higher stability shoe because your feet are prone to inward rolling motions. Neutral runners should go for a moderate stability shoe, and runners with high arches should choose a cushioned shoe that provides midsole padding with flexibility. (9)
What Is a Stress Fracture?
Stress fractures can be classified into two types: fatigue and insufficiency. The fatigue fracture is caused by an abnormal stress to a normally elastic bone, while insufficiency fractures arise when there’s stress on a bone that’s mineral-deficient or abnormally elastic. Insufficiency fractures are most prevalent in nutrient-deficient and older populations, when osteoporosis and rheumatoid arthritis are more common.
According to research published in the Journal of Athletic Training, the tibia is reported to be the most frequently injured bone in runners, followed by the fibula, metatarsal and pelvis. Fifteen percent of all stress fractures occur in runners, accounting for 70 percent of all of their injuries. In dancers, the metatarsal is the most common location of injury. Stress fractures in the ribs have been described in golfers, and stress fractures of the pars interarticularis are prevalent in racket sports and basketball players. (10)
If you experience localized bone tenderness that’s not associated with a specific incident, you may have a stress fracture. The pain does not decrease with rest, and you may notice redness, swelling and tenderness when you press on the bone.
The vast majority of stress fractures heal within eight weeks of treatment. However, a small percentage may require surgical intervention.
Stress fractures can be grouped into two categories: low-risk and high-risk. A low-risk stress fracture will typically heal on its own after refraining from running or sports for six to eight weeks. These fractures commonly take place in the tibia, fibula and metatarsals. A high-risk stress fracture is one in an area that doesn’t heal easily, such as stress fractures to the navicular, pelvis and femur. High-risk fractures require significantly more time avoiding physical activities like running.
Root Causes of a Stress Fracture
According to the American Academy of Orthopedic Surgeons, stress fractures are often the result of increasing the intensity of an activity too rapidly. They can also be caused by the impact of an unfamiliar surface, using improper equipment and increasing physical stress. (11)
Track-and-field athletes have the highest incidence of stress fractures compared to other athletes, and stress fractures of the tibia, metatarsals and fibula are the most frequently reported sites.
A stress fracture is a fatigue fracture of bone caused by repeated submaximal stress. That means that the force required to generate a stress fracture is less than the maximum force tolerated by the bone, but its repetitive application causes a disruption in the bone homogeneity. During a physical activity, the muscles become fatigued, and this increases the force put on the bone, contributing to the overloading process. Over time, microfractures that occur because of overloading stress accumulate, and a stress fracture may develop. (12)
Hard surfaces usually pose a higher risk for stress fractures. Tibial strain and strain rates in runners are 48 percent to 285 percent higher when running on the ground than when running on a treadmill. Worn running shoes may also increase the risk for stress fracture because of decreased shock absorption. (13)
Studies involving female athletes suggest that disordered eating, irregular periods and osteoporosis significantly increase the risk of stress fractures because of the negative effect on bone health. A study published in the American Journal of Sports Medicine found that significant risk factors for women include lower bone density, a history of menstrual disturbance, less lean mass in the lower limb, a discrepancy in leg length and a low-fat diet, adding stress fractures to the list of low-fat diet risks. The study also revealed that the age of the athlete’s first menstrual cycle and her calf girth were the best independent predictors of stress fractures in a woman. (14)
Treating a Stress Fracture
Prevention and early intervention are the preferable treatments, but it’s difficult to predict injury because athletes vary with regard to biomechanical predisposition, training methods and other factors — such as diet, muscle stretch and flexibility. (15)
An MRI is currently the gold standard for diagnosing a stress fracture. This is largely due to the instrument’s ability to display both soft tissue and bone edema. One of the earliest signs of stress fracture is bone edema, a condition where fluid is found within the bone. The fluid develops in response to an injury, just like when muscles collect fluid. Bone edema isn’t easily visible on standard radiographic imaging, which is why an MRI is often used.
Conventional treatment for stress fractures varies with the location of the fracture and the goals of the patient. According to research published in the Open Access Journal of Sports Medicine, a two-phased protocol for rehabilitation for a runner with lower extremity stress fractures is generally accepted as a suitable treatment. The first phase includes rest of the site, maintenance of aerobic fitness, physical therapy modalities and oral analgesics, other than non-steroidal anti-inflammatory drugs that potentially slow healing the broken bone.
The second phase of stress fracture rehabilitation should begin about two weeks after the person is pain-free when walking and cross-training, focusing on a progressive return to full-impact activities, such as running. Rehabilitation should focus on muscle endurance training, core and pelvic girdle stability, balance training, flexibility, and gait retraining when needed. Return to sport activities can continue when the person experiences pain-free weight-bearing.
Stress Fracture Takeaways
- Stress fractures are caused by tiny cracks in the bone that result from the repetitive application of force, such as running long distances or repeatedly jumping up and down.
- Once you have a stress fracture, you’re at risk for developing the same injury again, so be sure to evaluate your training methods and intensity.
- Seek professional advice if you’re unsure about your workouts or training, if you need new, proper running shoes, or if you need to formulate a new training program that focuses on gradual intensity and stability.
- To avoid a stress fracture, be sure to increase your training intensity gradually, by about 10 percent per week.
- Make sure to wear proper running shoes while training, and avoid the repeated stress of hard surfaces.
- Calcium and vitamin D intake can help strengthen bones and avoid cracks or fractures.
- If you’re recovering from a stress fracture, give your bone at least six weeks of rest, and gradually begin training again once the pain is completely gone.