This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
6 Ways to Improve Scleroderma Symptoms Naturally
September 22, 2017
Scleroderma is a rare and difficult disease. Also known as systemic sclerosis, it affects about 75,000 to 100,000 people in the United States. It can be a severe condition that can cause significant physical distress, disability and shortened life expectancy. Many patients with scleroderma are uncomfortable and self conscious about their appearance. This leads to social discomfort, anxiety and even depression. (1)
Because scleroderma is an autoimmune disease, the symptoms and severity of the condition vary from person to person, and scientists aren’t exactly sure what causes the disease. Treatment plans are multidisciplinary, tackling symptoms that involve many bodily organs. This can be an extremely difficult disease to live with. But with some support and awareness, you can become more comfortable in your skin and relieve common symptoms like pain, fatigue and malnutrition.
What Is Scleroderma?
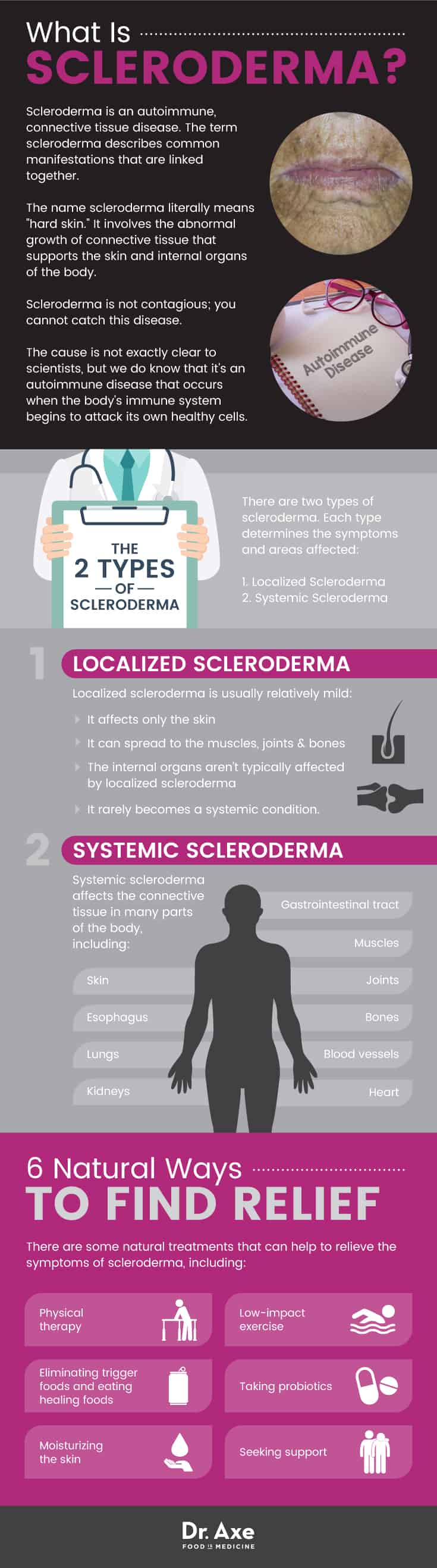
Scleroderma is an autoimmune, connective tissue disease. The term scleroderma describes common manifestations that are linked together. But the course and severity of this disease varies greatly from person to person.
In fact, it can affect the skin and other organs of the body, including the heart, lungs, kidneys and intestinal system. The name scleroderma literally means “hard skin.” It involves the abnormal growth of connective tissue that supports the skin and internal organs of the body. (2)
This is an autoimmune disease, which means that the body’s immune system attacks your healthy cells. Researchers have found that patients with scleroderma have immunologic abnormalities, which is suggested by the presence of autoantibodies such as ANA, anticentromere and anti-Sci-70. These antibodies are responding to an antigen, or trigger, that the immune system deems dangerous, even though there is no foreign invader (like bacteria or a virus) in the blood.
Signs & Symptoms of Scleroderma
The signs and symptoms of scleroderma vary widely, ranging from minor to severe and life-threatening. The severity of symptoms depends on which parts of the body the disease affects and how widespread it has become.
Scleroderma causes the skin to become thick and hard. It’s associated with a buildup of scar tissue, which can damage your internal organs. There are two types of scleroderma. Each type determines the symptoms and areas affected. Here’s an explanation of the two types and the symptoms:
Localized Scleroderma
Localized scleroderma is usually relatively mild. It affects only the skin, although it can spread to the muscles, joints and bones. The internal organs aren’t typically affected by localized scleroderma and it rarely becomes a systemic condition. There are two forms of localized scleroderma (3):
- Morphea: This is when discolored patches form on the skin. The patches vary in size, color and shape, and they have a waxy appearance.
- Linear scleroderma: This is when streaks or bands of hard, thick skin develop on the arms and legs. When the streaks form on the head or neck, this is called en coup de sabre because it resembles the wound of a saber or sword.
Systemic Scleroderma
Systemic scleroderma affects the connective tissue in many parts of the body, including the skin, muscles, joints, bones, blood vessels, heart, gastrointestinal tract, esophagus, lungs and kidneys. There are two types of systemic scleroderma:
- Limited cutaneous systemic sclerosis: About 50 percent of patients have limited scleroderma, which is known to be a slower, less widespread form of the illness. Limited scleroderma involves skin thickening. It’s usually confined to the fingers, hands and face. Internal problems usually don’t develop with limited sclerosis. If they do develop, it can take several years. Sometimes, limited sclerosis is called “CREST,” which stands for the first letters of five common features of the illness (4):
- Calcinosis: When the formation of calcium deposits cause small, white lumps to form under the skin of the fingers and other areas of the body.
- Raynaud phenomenon: When areas of the body, like the fingers and toes, feel numb and cold when exposed to cold temperatures or stress. Raynaud phenomenon is caused by limited blood circulation after smaller arteries that supply blood to the skin begin to narrow.
- Esophageal dysfunction: When the skin in the esophagus hardens, it makes the muscles less functional and makes swallowing more difficult.
- Sclerodactyly: When the buildup of fibrous tissue causes the skin to tighten so much that you can no longer curl your fingers and you lose mobility.
- Telangiectasia: When you develop threadlike red lines on the skin because the blood vessels near the surface of the skin dilate.
A complication of CREST syndrome is pulmonary hypertension, a very severe condition that has a mortality rate of 50 percent after only two years. This condition occurs when the lung’s blood vessels become so narrow that it causes impaired blood flow and shortened breath.
- Diffuse scleroderma: This form more frequently involves a hardening of internal organs, such as the gastrointestinal tract, kidneys, heart and lungs. Diffuse scleroderma is also associated with skin thickening and tightness that comes on quickly and spreads to more skin areas than in limited scleroderma. It usually affects the hands, face, chest, stomach and arms. This is the most severe type for people who experience symptoms in their internal organs, which occurs in about one-third of patients with diffuse scleroderma. (5)
Scleroderma symptoms depend on the type of condition and which organs it has affected. Here’s a general list of possible symptoms:
- dry, stiff skin
- red spots on the hands and face
- ulcers on the fingers and toes
- fatigue
- dry mouth
- tooth decay and loose teeth
- difficulty swallowing
- shortness of breath
- heartburn
- changes in appetite
- diarrhea
- constipation
- gassiness
- abnormal heartbeat
- uncontrolled high blood pressure
- headaches
Causes & Risk Factors
Scleroderma involves an excess formation of scar tissue, which decreases blood flow to your extremities and causes the hands and organ tissue to become hard. When you have scleroderma, your cells make too much collagen, as if you were injured and needed to replace dead skin. The extra collagen in your tissues then prevents your body’s skin and organs from functioning properly. (6)
Scleroderma is not contagious; you cannot catch this disease. The cause is not exactly clear to scientists, but we do know that it’s an autoimmune disease that occurs when the body’s immune system begins to attack its own healthy cells.
Based on the research, here are some facts about the risk factors associated with scleroderma (7):
- Women between the ages of 30 and 50 are most at risk of developing scleroderma. Data suggests that approximately 80 percent of patients with scleroderma are female, and one-half develop the condition before the age of 40.
- African- and Native Americans are more at risk than Caucasians.
- Children can develop scleroderma, but this is rare and the disease is different than it is for adults.
- Scleroderma has a worse prognosis in individuals older than 65 because they are at a higher risk of complications like pulmonary hypertension.
- A family history of autoimmune connective tissue diseases, such as lupus, may increase the risk of developing scleroderma.
- Some environmental factors may trigger scleroderma, such as silica (a chemical compound made of silicon) and solvents.
Conventional Treatments
There is no cure for scleroderma and, because symptoms and the course of the disease vary from person to person, the treatment methods depend on the patient’s type and severity of the condition. Research shows that there is no treatment that has proven to modify the overall disease. So the only effective course of therapy is to target specific affected organs before irreversible damage occurs. (8)
Scleroderma can affect many different organs of the body, so it’s not uncommon that several doctors are involved in a patient’s care. If the disease has spread to the gastrointestinal tract, doctors may prescribe proton pump inhibitors (PPIs) to treat heartburn. Angiotensin-converting enzyme (ACE) inhibitors (which is a blood pressure medication) are prescribed for scleroderma-related kidney damage or failure, and anti-inflammatory drugs, like glucocorticoids, are prescribed to reduce muscle pain and weakness. For patients who suffer from lung damage, medications like cyclophosphamide and mycophenolate are prescribed to reduce scarring of the lung tissue. And prostacyclin-like drugs and endothelin receptor antagonists are used to treat high blood pressure in the arteries of the lungs. (9)
Immunosuppressive therapy, which lowers the activity of the body’s immune system, is commonly used to reduce scleroderma symptoms. Corticosteroids are also prescribed, but researchers suggest that this may be dangerous when treating active scleroderma skin disease because these types of drugs are associated with serious complications, such as renal issues. (10)
6 Natural Treatments for Scleroderma
Although there is no one treatment plan for every patient with scleroderma, certain natural remedies can help to minimize the damage to specific affected organs. Researchers indicate that addressing nutrition, pain, musculoskeletal disuse and emotional aspects of the disease (such as social withdrawal, fear and depression) can be beneficial to the patient. With that in mind, here are some ways to relieve the emotional and physical symptoms of scleroderma in a natural way (11):
1. Physical Therapy
Physical therapy can help patients who are suffering from stiff and painful joints. Regular physical therapy can help to prevent the loss of joint motion, which occurs when blood flow decreases and your skin becomes taut. Exercises that increase range of motion include stretching the fingers, hands, wrists and shoulders. Strengthening the fingers and hands is also important when working with scleroderma patients. Exercises like squeezing putty or rice improve grip strength. (12)
Physical therapy will also help a patient with scleroderma to perform everyday activities in a way that won’t put stress on his or her joints. Patients often practice their stretching program at home so that the joints don’t become stiff. Splints are also used to prevent the loss of range of motion and contractures. This is when the muscles, tendons or tissue harden and lead to rigid or deformed joints. (13)
2. Reduce Pain with Exercise
Studies show that 60 to 83 percent of patients with scleroderma experience pain that reduces their physical and social functioning. The pain associated with scleroderma varies, affecting different areas of the body and ranging in intensity, so there’s not one tool for pain management that will work for everyone.
If you are able to engage in physical activity, it can help to reduce pain by relieving muscle tension, improving circulation, and stretching and strengthening your joints. Try low-impact exercises like swimming, water aerobics, walking, cycling, using an elliptical, and yoga, if appropriate.
Before you begin using exercise as a natural remedy for joint pain, talk to your doctor or physical therapist about your limitations and the best approach for your body. Recent research published in Disability and Rehabilitation found that approximately half of patients with both limited and diffuse scleroderma are currently exercising by walking. But patients engage in a wide variety of exercise-related activities. Researchers indicate that individually designed exercise programs are most likely to support and encourage physical activity in patients with scleroderma. (14)
3. Moisturize the Skin
Patients with scleroderma suffer from dry, stiff and thick skin, so making sure to keep the skin moist can be helpful. Moisturize your entire body as soon as you get out of the bath of shower. Natural moisturizers like coconut oil, olive oil or almond oil are some great options. As a cooling agent, essential oils with menthol can help to reduce inflammation, reduce itchiness and relieve pain. Try combining 1–2 drops of peppermint oil with ½ teaspoon of coconut oil. Apply the mixture topically to the area of concern. Start by doing a patch test on a small area of skin to make sure that the peppermint isn’t irritating before you apply it to a larger area.
It’s important to avoid harsh soaps, laundry detergent and household cleaners that contain dangerous chemicals, which can make symptoms worse. Also, taking very hot showers or baths can dry the skin and so can being out in the sun for too long. In the winter months, using a humidifier can also be helpful.
4. Remove Triggers and Eat Healing Foods
Research shows that about 30 percent of patients with scleroderma are at risk of malnutrition and in 5–10 percent of patients, gastrointestinal disorders are the leading cause of death. As part of the multidisciplinary treatment plan, patients should include nutritional intervention, which improves gastrointestinal symptoms and quality of life. (15)
Because scleroderma is an autoimmune disease, you want to avoid any food triggers that are causing an immune response and inflammation. Certain foods can particularly aggravate the gastrointestinal tract, which scleroderma may affect. This includes refined carbohydrates, artificial ingredients, spicy foods, alcohol and caffeine.
It’s also common for people with an autoimmune disease to suffer from nutrient malabsorption and food sensitivities. For this reason, trying an elimination diet may help you to pinpoint which specific foods are stimulating an immune response.
The next step is to bring healing foods into your diet. Some of the best foods that you can eat to help heal your body and reduce inflammation include:
- fresh vegetables, like asparagus, beets, broccoli, carrots, celery, cucumbers, leafy greens, mushrooms and squash
- berries, like blueberries, blackberries, goji berries, raspberries and strawberries
- wild-caught fish, including salmon, halibut and mackerel (avoid shellfish)
- organic, grass-fed meat, such as beef, bison, chicken, turkey, lamb and eggs
- organic, raw dairy, like A2 cow’s milk, goat milk, goat cheese and kefir
- healthy fats, like avocados, coconut oil, coconut milk, grass-fed butter, olive oil and almond oil
- nuts and seeds, including almonds, pecans, pistachios, walnuts, chia seeds, flaxseeds, pumpkin seeds, nut butter and seed butter
- spices and herbs, like basil, cilantro, cinnamon, cumin, garlic, ginger, oregano, rosemary and turmeric
5. Take (or Eat) Probiotics
Probiotics may help to relieve scleroderma symptoms because they help repair your gut and tissues. More and more research is showing that leaky gut may provide a unifying theory for most autoimmune conditions. The microbiome plays a major role in keeping the immune system in check so that it doesn’t produce too many antibodies. When we have good bacteria in the gut, they help to restore a balance between pro- and anti-inflammatory immune cells.
Research conducted at the University of Utah shows that probiotics significantly improves reflux and bloating in patients with scleroderma. Participants noticed significant results after two months of daily probiotic use. (16)
Taking a probiotic supplement or eating probiotic foods is the best way to restore the balance of bacteria in your gut. Some of the best probiotic foods include kefir, kombucha, yogurt, cultured vegetables, apple cider vinegar and tempeh.
6. Seek Counseling or Support
There’s plenty of research that indicates the many problems faced by people living with scleroderma. Patients commonly suffer from psychological distress, including anxiety, depression and body image issues. Studies show that peer support is an effective first step to reduce symptoms of depression because patients get to talk openly with someone who has experienced similar problems. Telephone or internet support groups are more common. They are better-attended than face-to-face groups, according to research, most likely because they are flexible and private. (17)
Cognitive behavioral therapy techniques and social skills training programs have also proven to be effective and beneficial for scleroderma patients. These programs help patients to deal with anxiety caused by social interactions and body image concerns. Know that if you are suffering from scleroderma, you aren’t alone and there are many support groups that are in place to help you deal with the physical changes that you are experiencing. (18)
Final Thoughts
- Scleroderma is an autoimmune, connective tissue disease. In fact, the name literally means “hard skin,” and it involves the abnormal growth of connective tissue that supports the skin and internal organs of the body.
- There are two types: localized scleroderma and systemic scleroderma. The type determines the symptoms of the disease and areas affected.
- Some symptoms of scleroderma include: dry, stiff skin; red spots on the hands and face; fatigue; pain; dry mouth; shortness of breath; heartburn and gastrointestinal issues; abnormal heartbeat; and headaches.
- Scleroderma involves an excess formation of scar tissue, which decreases blood flow to your extremities and causes the hands and tissue of your organs to become hard. When you have scleroderma, your cells make too much collagen, as if you were injured and needed to replace dead skin.
- There is no cure for scleroderma. Because scleroderma symptoms and the course of the disease vary from person to person, the treatment methods depend on the patient’s type and severity of the condition.
- There are some natural treatments that can help to relieve the symptoms of scleroderma, including: physical therapy; low-impact exercise; eliminating trigger foods and eating healing foods; taking probiotics; moisturizing the skin; and seeking support.








