This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Psoriasis Symptoms, Risk Factors + 5 Natural Remedies
June 12, 2023

If you have dry, itchy, scaly, painful, red patches of skin that crop up, there’s a chance you’re suffering psoriasis symptoms.
Psoriasis is a persistent autoimmune condition that causes red, raised plaque to form on the surface on skin, which can be both irritating and embarrassing. Considered to have no definitive cure, it usually comes and goes in cycles over the course of someone’s life, often causing scaly, uncomfortable skin flare-ups at times when immune function is low or stress levels are high.
It’s believed to affect more than 3 percent of the U.S. population — or more than 5 million (and up to 7.5 million) adults at any time.
Doctors normally use medications and prescription creams to help lower the appearance of red psoriasis patches on the skin, but these don’t actually solve the underlying problem or autoimmune condition itself.
Below the skin’s surface, psoriasis can cause skin cells to multiply at a very rapid pace, sometimes up to 100 times faster than in someone who doesn’t have this condition. This causes a high amount of skin cells to eventually reach the outer layer of the skin and die off on the surface (as all aged skin cells do), leaving behind a raised, red plaque covered with white/silver scales.
Experts still don’t know of any way to end this cycle from happening for good, although research shows that improving immunity and helping treat sensitive psoriasis skin topically using natural, gentle ingredients can ease symptoms. You might also be surprised to know how better managing stress and your routine can help reduce your psoriasis as well. For example, studies show that more than 70 percent of people having psoriasis flare-ups report recent emotional trauma.
Because psoriasis is an autoimmune disorder, it takes a variety of lifestyle changes and remedies to bring about significant relief, especially if the autoimmune disorder has become severe and also causes other symptoms, such as joint pain and fatigue. Thankfully, if you follow a psoriasis diet and make other lifestyle changes, you can help manage these symptoms.
Most Common Psoriasis Symptoms
Plaque psoriasis is the most common type of this condition, but there are also several other forms of psoriasis. All types cause discomfort in the skin in one way or another, although when symptoms first appear and which parts of the body they impact most depend on the specific form.
Psoriasis symptoms appear on the skin of the knees, elbows and scalp most often. Less frequently some people also develop psoriasis symptoms on their stomaches, backs, hands and feet.
There are several forms of psoriasis, all of which have their own hallmark symptoms:
- Plaque psoriasis (the most common form) causes red, scaly skin patches. Compared to other forms, plaque psoriasis tends to develop even if someone wasn’t severely ill beforehand or suffering from any noticeable autoimmune disorder symptoms.
- Nail or scalp psoriasis affects the nail beds and head, causing dryness and detached nails.
- “Mild psoriasis” causes less severe psoriasis symptoms than other forms and might be mistaken for eczema or even dandruff. This type is usually the most receptive to remedies using natural skin care products.
- “Severe psoriasis” is a term usually given to painful forms of psoriasis, including pustular and guttate psoriasis.
- Pustular psoriasis causes pus-filled, inflamed blisters on the skin that are usually painful.
- Inverse psoriasis causes bright red, shiny lesions that appear in areas where skin folds (including the armpits, groin and under the breasts).
- Erythrodermic psoriasis causes the red skin scales to peel off in “sheets,” which can lead to severe sunburns or infections when someone is not careful about protecting skin or leaves it untreated. This type is usually caused by a withdrawal effect after stopping psoriasis medications.
- Guttate psoriasis is the type most common among children and teens. This usually causes small red bumps or patches that can be triggered by low immune function, stress or infections, such as strep throat and tonsillitis.
The most common symptoms of psoriasis, especially those seen in people with plaque psoriasis, include:
- plaques of red skin, sometimes also covered with a crust of scales that tend to be silver or white
- loose skin or lesions that can be sensitive, itchy and painful
- dandruff on the scalp
- cracked, discolored skin that easily bleeds and bruises
- discoloration in the finger and toenails or growth of toenail fungus
- nails that detach from the nail beds and can be painful or bloody
Many people with psoriasis also suffer from emotional problems due to feeling embarrassed and hopeless about their skin.
Other than plaque psoriasis, additional psoriasis symptoms can result from other form, including:
- joint pain and inflammation — common among those with psoriatic arthritis and affects about 10 percent to 30 percent of people with any form psoriasis
- severe plaque, scales and pain in the hands and feet — most common among people with pustular psoriasis
- worsened immune function — psoriasis can contribute to recurring infections, slow skin healing and permanent damage to the skin
- fatigue
- other symptoms common among people with autoimmune disorders, like digestive complaints, brain fog and allergies

Causes
Like other autoimmune disorders, psoriasis is caused by a combination of different factors. Most doctors are unsure about what exactly leads most people to develop this skin condition, but research suggests that the major contributing factors include:
- genetics — scientists have now identified about 25 genetic variants that make a person more likely to develop psoriatic disease
- being under high amounts of physical or emotional stress — just another way chronic stress kills your quality of life
- high levels of inflammation and weakened immunity, specifically the activation of T lymphocytes leading to release of cytokines
- eating a poor diet and having difficulty digesting fats and protein
- hormonal changes (such as puberty, pregnancy or menopause)
- deficiency in certain nutrients, such as vitamin D deficiency
- poor liver function
- reactions to medications and over-the-counter pain pills (such as Advil, Motrin, blood pressure prescriptions, beta-blockers and anti-malarial medications, like hydroxychloroquine)
How to Treat Psoriasis Symptoms Naturally
1. Eat an Anti-Inflammatory Diet
Many people see great improvements in their psoriasis symptoms when they clean up their diets and boost their nutrient intake. Some of the best foods for helping ease psoriasis symptoms and lower autoimmune reactions include:
- Probiotic foods: Raw, cultured dairy (like kefir, amasai, yogurt) plus cultured vegetables support digestion, reduce inflammation and boost immunity.
- High-fiber foods: Fiber is found in just about all plant foods that are high in nutrients and antioxidants, such as fresh fruits, vegetables, sprouted legumes and seeds/nuts.
- Wild-caught fish: Salmon, mackerel, sardines and halibut are examples of fish high in anti-inflammatory omega-3 fats.
- Foods high in zinc: Zinc is critical for keeping skin healthy. Good sources include pumpkin seeds, grass-fed beef, seeds and legumes.
- Foods high in vitamin D and vitamin A: Brightly colored veggies and fruit are your best source of vitamin A, including leafy greens, berries and broccoli. Research shows that vitamin A is critical for skin healing and acts like an antioxidant that reduces inflammation. Vitamin D affects the immune system and skin cells in positive ways and can be obtained from cage-free eggs, raw milk and certain mushrooms.
On the other hand, foods that can aggravate psoriasis symptoms and contribute to autoimmune reactions include:
- Common allergens: Conventional dairy products and gluten can both cause sensitives or food allergies within the digestive tract that trigger inflammation. Many people with psoriasis have difficulty digesting A1 casein, a protein found in most cow’s milk. Instead, look for cultured goat’s milk products (like kefir or yogurt) or cow’s milk that is labeled as exclusively A2 casein. Instead of consuming foods with gluten (all those made with wheat, barley, rye), try ancient grains that are gluten-free, like oats, buckwheat, amaranth and quinoa.
- Factory-farmed meats: These tend to be lower in nutrients and higher in omega-6 fats, which can raise inflammation.
- Hydrogenated oils and fried foods: Found in most packaged or fast foods, these foods may be difficult to digest for people with psoriasis and are very high in omega-6s, which most people already get way too much of.
2. Use Natural Herbs and Supplements
The top natural remedies for psoriasis include:
- Hydrochloric acid (one to three capsules per meal): helps with protein digestion and decreases psoriasis flare-ups
- Omega-3 fish oil (1,000–2,000 grams daily): lowers inflammation
- Vitamin D3 (5,000 IU daily): low levels of vitamin D and vitamin D deficiency are associated with psoriasis
- Milk thistle (250 milligrams three times daily): helps promote liver detoxification and reduces cellular growth
- Probiotics (50 billion units daily): lower autoimmune reactions and improve digestion by increasing good bacteria and crowding out bad bacteria
- Adaptogen herbs and vitamin B12: help the body deal with the effects of stress
- Digestive enzymes: boost nutrient absorption and can help lower food sensitives
- Bone broth: provides many nutrients, like collagen and glucosamine, which repair damaged skin, digestive tissues and joints
Studies also indicate that urea cream can help soothe skin issues, including psoriasis.
3. Get at Least 20 Minutes of Sunshine Daily
Getting 20 minutes of sunshine daily, three to four days a week, can greatly improve psoriasis symptoms by raising vitamin D levels.
Research shows that vitamin D changes the way cells grow and might help slow down skin cell production in people with psoriasis, which reduces plaque. This helps ease psoriasis symptoms like thick skin and scaling.
Vitamin D also positively affects how the immune system functions and can lower autoimmune reactions or inflammation.
If you have sensitive psoriasis patches due to ending medication use or experiencing a flare-up, be very careful about sun exposure until you’re healed in order to prevent burns. Wear sunscreen if you’re prone to burns, and try to get sunlight when the sun isn’t at its strongest, which is usually between 10 a.m. to 2 p.m.
Another option besides spending time in the sun is to use an indoor light box, although it’s not known if this works as well to boost vitamin D levels.
4. Lower Stress
Both emotional and physical stress can cause psoriasis to develop or psoriasis symptoms to become worse. People with psoriasis who use relaxation techniques and make an effort to reduce stress usually notice improvements in symptoms, which makes sense considering this condition is an autoimmune disorder.
Autoimmune disorders are often aggravated by stress due to how the “fight or flight” response impacts the immune system, releasing higher levels of inflammatory proteins called cytokines and contributing to hormonal imbalances.
Many studies have found that a large proportion of patients with high amounts of emotional stress experience some sort of disease or illness, which can then cause even more stress and trigger a vicious cycle. As mentioned above, the vast majority of people with psoriasis report high amounts of stress prior to the outbreak of their symptoms.
Stress relievers (like exercise, meditation, yoga and spending time outdoors) can help keep inflammation at bay and therefore psoriasis symptoms under control.
5. Moisturize and Use Soothing Essential Oils
Psoriasis symptoms are usually at their worst when skin is very dry and inflamed. Moisturizing the skin and using natural anti-inflammatory oils can ease symptoms like redness, scaling and pain.
Depending on where itchiness and flaking occur, moisture can be increased by using natural shampoos, lotions, gels, foams, creams and more greasy ointments. Keep skin moisturized by applying thick creams or oils, such as virgin coconut oil for skin, raw shea butter or a homemade body butter lotion.
Other options to help lock in moisture include petroleum jelly (Vaseline), almond oil or virgin olive oil. Try moisturizing after a warm shower (avoiding very hot water), but be careful not to add too much oil before exercising or during the warm months of the year since sweat mixed with thick creams can make psoriasis symptoms worse.
You can keep skin damp during the night by applying lotion, wrapping a bandage around the area and then gently washing away the lotion in the morning — just be careful to use natural products that are not drying.
Essential oils like lavender, frankincense, geranium and tea tree oil can also soothe inflamed skin and support the healing process, without the need for irritating prescription creams.
First perform a small patch test to make sure you don’t react badly to the oils. Use a very small amount, since essential oils are highly concentrated.
Mix three drops of lavender oil and three drops of frankincense oil with one teaspoon of coconut oil, and rub onto the affected area one to three times daily.
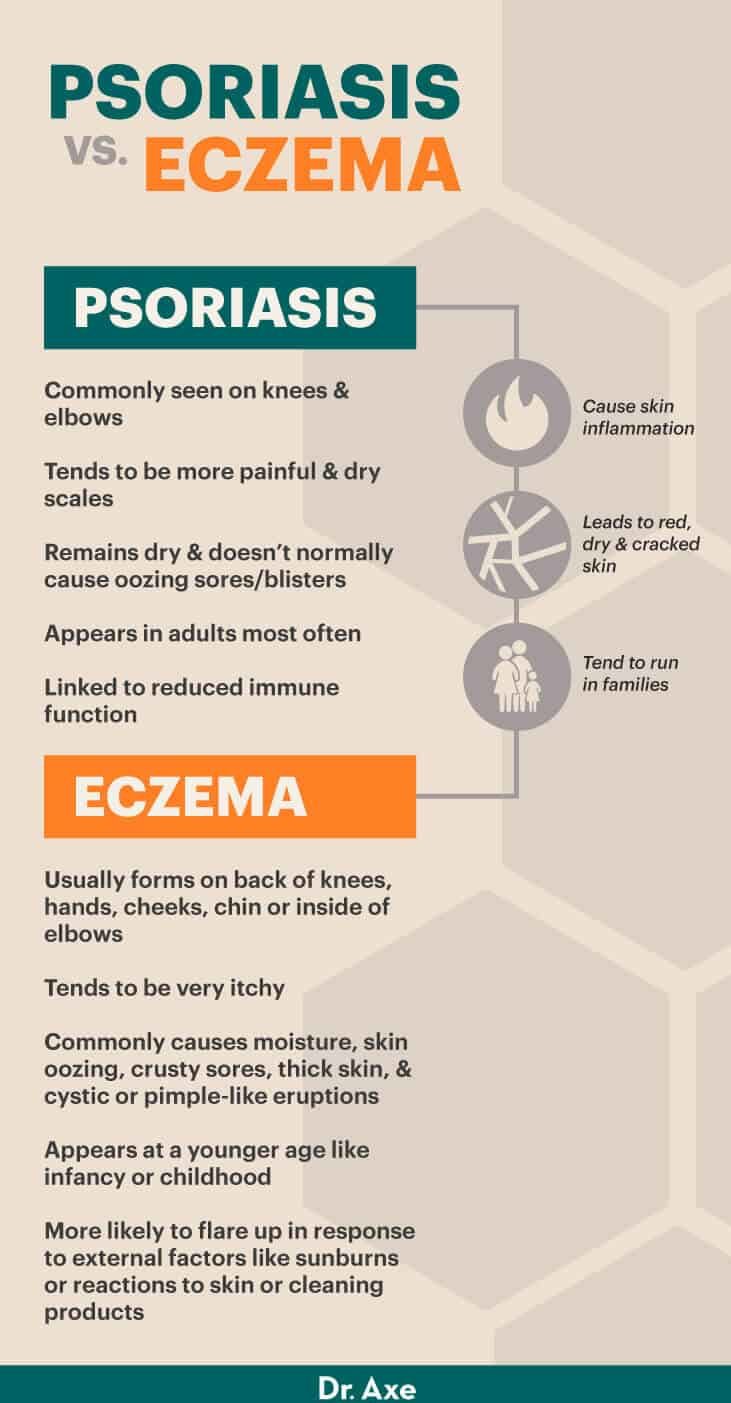
Psoriasis vs. Eczema
It’s easy to mistake psoriasis for other skin conditions, including eczema, which has some of the same symptoms, or even rosacea.
Compared to eczema — which also causes skin inflammation and red, dry, cracked skin — what does psoriasis look like that makes it noticeably different? First off, location: Psoriasis is commonly seen on the knees and elbows, while eczema usually forms on sensitive areas like the backs of knees, hands, cheeks or chin, and the inside of the elbows.
Eczema tends to be very itchy, while psoriasis may cause more pain and dry scales on the skin in addition to plaques. Another factor that distinguishes eczema from psoriasis is that eczema commonly causes moisture on the skin and skin oozing, crusty sores, thick skin, and cystic or pimple-like eruptions, but psoriasis normally doesn’t cause such sores/blisters and remains very dry.
Both conditions tend to run in families, although their major causes are somewhat different. Eczema commonly appears at a younger age, such as during infancy or childhood, while psoriasis is an autoimmune disorder that appears in adults most often and emerges whenever immunity has been compromised, such as following other illnesses or stress.
There’s a link between reduced immune function and psoriasis — for example, respiratory infections, diabetes and arthritis might all contribute to its formation. While eczema can also be triggered by inflammation and sensitivities, it’s more likely to flare up in response to external factors, such as sunburns or reactions to skin care or household products (soaps, detergents, lotion, etc.).
Final Thoughts
- It’s believed psoriasis affects greater than 3 percent of the U.S. population.
- Plaque psoriasis is the most common type of this condition, but there are also several other forms, including nail or scalp psoriasis, mild psoriasis, sever psoriasis, pustular psoriasis, inverse psoriasis, erythrodermic psoriasis, and guttate psoriasis.
- The most common psoriasis symptoms include plaques of red skin, sometimes also covered with a crust of scales that tends to be silver or white; loose skin or lesions that can be sensitive, itchy and painful; dandruff on the scalp; cracked, discolored skin that easily bleeds and bruises; discoloration in the fingers and toenails or growth of toenail fungus; and nails that detach from the nail beds and can be painful or bloody. Many people with this condition also suffer from emotional problems due to feeling embarrassed and hopeless about their skin.
- Other psoriasis symptoms include joint pain and inflammation, severe plaque, scales and pain in the hands and feet, worsened immune function, fatigue, and common autoimmune symptoms.
- Causes include genetics, high amounts of physical or emotional stress, inflammation, weakened immunity, poor diet, difficulty digesting fats and protein, hormonal changes, nutrient deficiencies, poor liver function, and reactions to medications.
- You can help naturally treat psoriasis symptoms by eating an anti-inflammatory diet, using natural herbs and supplements, getting at least 20 minutes of sunshine daily, lowering stress, and moisturizing and using essential oils.