This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
How to Manage Ankylosing Spondylitis Symptoms Naturally
December 3, 2017

Ankylosing spondylitis is a type of arthritis. The condition causes pain and stiffness in the back, and over time it can actually cause the bones in the spine (called the vertebrae) to fuse together. It also causes arthritis between the spine and pelvis, and may also affect other joints. Because it is a long-term inflammatory condition affecting the joints, it is called a spondyloarthropathy, like psoriatic arthritis and reactive arthritis. (1)
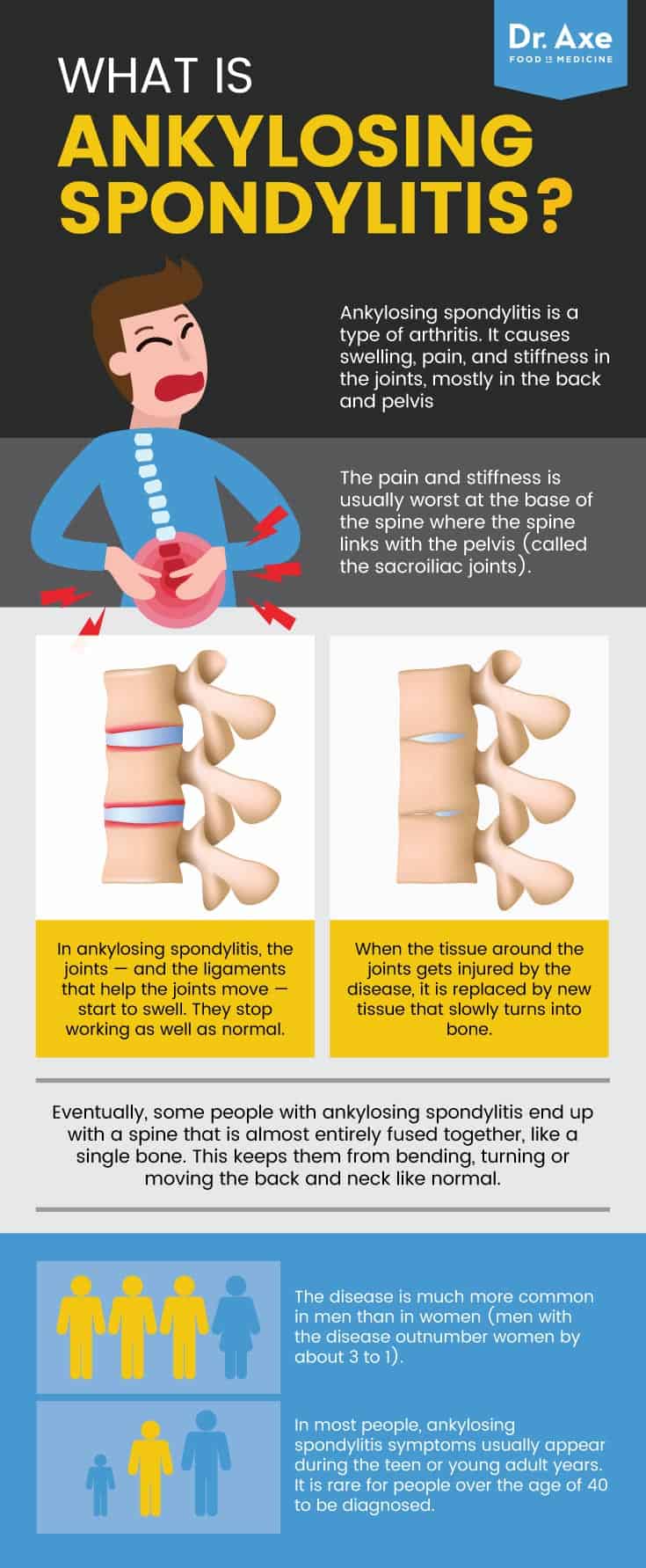
The disease is much more common in men than in women (men with the disease outnumber women by about 3 to 1). It is almost as common as another arthritic condition that is more well known: rheumatoid arthritis. Ankylosing spondylitis affects between 0.35 and 1.3 percent of people in the U.S. (2)
Although ankylosing spondylitis can cause severe pain and mobility problems, it can be managed well in many people. By following a few natural lifestyle tips, you may be able to help ease your symptoms and keep the disease from getting worse. (3)
What Is Ankylosing Spondylitis?
Ankylosing spondylitis is a type of arthritis. It causes swelling, pain, and stiffness in the joints, mostly in the back and pelvis. (4) The pain and stiffness is usually worst at the base of the spine where the spine links with the pelvis (called the sacroiliac joints). (5)
In ankylosing spondylitis, the joints — and the ligaments that help the joints move — start to swell. They stop working as well as normal. In some people, the pain and stiffness in the back comes and goes. In others, the pain and mobility limitation is constant and the disease gets worse over time. (6)
When the tissue around the joints gets injured by the disease, it is replaced by new tissue that slowly turns into bone. Over time, this can fuse the joints in the spine together. Eventually, some people with ankylosing spondylitis end up with a spine that is almost entirely fused together, like a single bone. This keeps them from bending, turning or moving the back and neck like normal. (7)
In most people, ankylosing spondylitis symptoms usually appear during the teen or young adult years. It is rare for people over the age of 40 to be diagnosed. Unfortunately, it takes many people a long time to get the right diagnosis — an average of eight years! Since its symptoms can be confused with those of more common types of arthritis, and since the symptoms usually develop slowly, an ankylosing spondylitis diagnosis usually comes after people have seen several different types of doctors. (8)
How do you diagnose ankylosing spondylitis?
While there is no simple ankylosing spondylitis test to confirm a diagnosis, there are several tests and exams you are likely to get if a doctor suspects you have the condition. You can expect these health checks before you are diagnosed: (9)
- A full physical exam
- Questions about your medical history
- Questions about all of your symptoms, even the ones that come and go
- Lab tests:
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) to check for inflammation in the body
- Human leukocyte antigen B27 (HLA-B27) to check for the HLA-B27 protein, which is more common in people with ankylosing spondylitis
- X-rays or MRI to check your joints for changes
The doctor will look at all of your results and symptoms, as well as other possible causes for your health problems, before making a diagnosis.
Is ankylosing spondylitis an autoimmune disease?
This is a bit more complex than it sounds. The current answer is “sort of.” It is believed that ankylosing spondylitis is both an autoinflammatory and autoimmune condition, since it has features of both types of conditions. (10)
For example, HLA-B27 causes cells to attack your own healthy tissue, which makes it like an autoimmune disease. But the disease is also helped when inflammatory signals are blocked, suggesting it’s an autoinflammatory condition. It is not widely considered an autoimmune disease, but rather an autoinflammatory disease, like psoriatic arthritis. (11)
HLA-B27 Testing
The HLA-B27 test checks for a protein on your white blood cells. HLA-B27 causes the immune system to attack healthy cells. (12) Up to 95 percent of people who do have ankylosing spondylitis are HLA-B27 positive. (13)
The test is a simple blood draw. Your doctor may order the test if he or she suspects your symptoms are caused by an autoimmune or autoinflammatory condition. Your doctor should also help you interpret your test results, but you can find the basics below.
- What does HLA-B27 negative mean?
- If you are HLA-B27 negative, it means you don’t have HLA-B27 on your white blood cells.
- Can you be HLA-B27 negative and still have ankylosing spondylitis?
- You can be negative for HLA-B27 and still have ankylosing spondylitis. (14)
- What does HLA-B27 positive mean?
- If you are HLA-B27 positive, it means you do have some HLA-B27 on your white blood cells. You inherited the HLA-B27 gene from your parents.
- Can you be HLA-B27 positive and not have ankylosing spondylitis?
- Not everyone who tests positive for HLA-B27 in the blood has an immune or inflammatory disorder.
- If you are HLA-B27 positive, you have a 10 percent chance (or less) of developing a spondyloarthritis condition. (15)
- If you do not have ankylosing spondylitis, you may have a different condition. The presence of HLA-B27 in you blood means you are at greater risk of developing such a disease. (16)
Ankylosing Spondylitis Signs & Symptoms
Ankylosing spondylitis symptoms vary from person to person. In some cases, symptoms start early and are unrelenting and severe. In others, symptoms may be mild or may come and go. Men are more likely to have more severe symptoms than women. (17)
Common signs and symptoms of ankylosing spondylitis include: (18, 19)
- Pain or stiffness in the lower back or hips
- Buttock pain
- Neck pain
- Fatigue
- Less often, pain or stiffness in other areas, such as the shoulders, ribs, hands and feet, or heels
Usually, the pain doesn’t start suddenly. It comes on slowly over months or years. It is also common for pain and stiffness to be worse in the morning or after you have been inactive (for example, after sitting at a desk or watching television). (20) Many people with ankylosing spondylitis feel better after they start moving.
In advanced disease, ankylosing spondylitis causes a stiff, fused spine that makes it difficult to move. People with severe anykosing spondylitis may have a stooped posture caused by the fused spine. The condition can also fuse bones in the rib cage and make it hard to breathe. Other complications may include eye inflammation, called uveitis, compressed bones in the spine caused by weakening of the bone, or problems with your heart. (21)
The disease may also cause problems affecting the gut or skin. In rare cases, the main symptom of the disease is swelling in the arms and legs. This type of disease is known as peripheral spondyloarthritis. (22)
Ankylosing Spondylitis Causes & Risk Factors
What is the cause of ankylosing spondylitis?
The exact cause of this condition is unknown. It has both environmental and genetic causes. (23) This means that if someone in your family has it, you are more likely to have it. This is in part due to the HLA-B27 gene, which increases your risk of a diagnosis of ankylosing spondylitis or another spondyloarthritis.
However, you could have a family history of it, carry the HLA-B27 gene and still not develop the disease. (24) This means that there are some factors in your environment that are at play as well in determining whether you get the condition.
What are the risk factors for ankylosing spondylitis?
You are at a greater risk of being diagnosed with ankylosing spondylitis if you are: (25, 26)
- Male
- Related to someone with the disease
- HLA-B27 positive
- In your teens, 20s, or 30s
- Ethnically Alaskan, Siberian, Eskimo, Scandinavian Lapps or from another far-north culture
- Native American, descended from certain tribes in the western U.S. or Canada
- Diagnosed with a related disease, such as Crohn’s disease, ulcerative colitis or psoriasis
African Americans are less likely than other races to be diagnosed with spondyloarthritis. (27) People with certain combinations of risk factors, such as having a family history of the disease and being HLA-B27 positive, have a greater chance of developing ankylosing spondylitis. (28)
Conventional Treatment
There is currently no cure for ankylosing spondylitis. However, some people with mild disease or early stages of the illness have periods of remission, when symptoms disappear. When ankylosing spondylitis treatment is required, it is aimed at reducing pain and stiffness as well as trying to prevent deformity and limits on your activities.
There are several common types of treatments used to treat the symptoms and prevent disease progression, including: (29, 30)
- Pain relievers, such as acetaminophen, or opioids such as tramadol
- Nonsteroidal anti-inflammatory drugs (NSAIDs, used to ease inflammation and stiffness), such as ibuprofen and naproxen sodium (over-the-counter) or indomethacin, diclofenac and celecoxib (prescription)
- Disease-modifying antirheumatic drugs (DMARDs, used to reduce pain and swelling and possibly prevent further joint damage), such as adalimumab, golimumab, etanercept and infliximab
- Corticosteroids to ease pain and stiffness in areas other than the spine
- Joint replacement surgery to help when use of certain joints, such as the hip, are significantly damaged by the disease
Most people start treatment using over-the-counter pain relievers and NSAIDs. If symptoms don’t improve, health care providers may recommend prescription pain or anti-inflammatory drugs, corticosteroids, or DMARDs. Some people may need a combination of drugs to help control pain and increase their joint function.
13 Natural Ways to Manage Ankylosing Spondylitis Self-Care
Natural approaches to self-care are essential in the effective, long-term management of ankylosing spondylitis. They are part of conventional treatment recommendations and the cornerstone to maintaining mobility and limiting pain.
You can follow the natural strategies below to self-manage many symptoms of ankylosing spondylitis:
- Exercise
- Practice good posture
- Participate in physical therapy
- Use hot or cold packs
- Ask about transcutaneous electrical nerve stimulation (TENS)
- Consider acupuncture
- Get a therapeutic massage
- Eat to reduce pain, inflammation and other symptoms
- Ask about folate supplements or probiotics
- Avoid potentially harmful supplements and diets
- Maintain a healthy weight
- Don’t smoke
- Use task-related accommodations
These strategies can help relieve symptoms and in some cases may improve your overall health. As always, speak with a doctor before changing your diet or exercise habits drastically, or before taking or stopping any supplements or medications.
Manage ankylosing spondylitis naturally
1. Exercise, exercise, exercise!
Daily physical activity is essential for people with this disease, and can reduce pain, improve mobility and posture, and help you maintain your flexibility. (31) As an added bonus, exercising can help you achieve a healthy weight (see step 11).
Helpful ankylosing spondylitis exercises
Despite the pain and stiffness that comes with ankylosing spondylitis, rest is not the answer. Regular exercise for your back, neck, chest and limbs is critical to maintain your flexibility and mobility. (32) You may also notice that your symptoms decrease after exercise or activity. Benefits of exercise for people with ankylosing spondylitis include increased flexibility, better range of motion, better posture, better sleep, and less stiffness and pain. (33)
The following resources have specific examples of ankylosing spondylitis exercises you can use to help keep yourself in good physical health:
2. Practice good posture techniques.
Being diligent about practicing good posture can help prevent spinal fusion in a stooped or deformed position. (37) Not everyone will have fusion in the spine, but practicing good posture can help keep your spine in a position that looks and feels better. Posture exercises should be practiced daily to have the best impact on your spine’s symptoms.
3. Participate in physical therapy.
A formal program with a physical therapist who understands ankylosing spondylitis can help your posture, joint mobility, pain, and ability to participate in activities. (38) It may include working on your posture, strength, flexibility, stretching, breathing, pain management and targeted activities for your needs.
4. Use heat or cold packs.
Warm compresses and heating pads or ice packs may be helpful for the temporary relief of pain and inflammation. (39)
5. Ask about a TENS (transcutaneous electrical nerve stimulation) machine for pain relief.
This may help reduce pain associated with the condition and can sometimes be rented from physical therapy centers or purchased over-the-counter. (40)
6. Consider acupuncture.
Research suggests acupuncture — done by a professional using sterile needles — may safely help reduce pain. (41) More research is needed to understand its full impact on different types of arthritis, however.
7. Get a therapeutic massage from an expert who is familiar with ankylosing spondylitis.
When done with care and an understanding of the individual’s disease, professional massage therapy can reduce stress and may have some temporary positive impacts on pain, stiffness and flexibility. However, some people find that massage can make their symptoms worse, so proceed with caution. (42)

8. Eat to reduce pain, inflammation and other symptoms. (43)
For example, avoid alcohol, get plenty of calcium and vitamin D to support bone health, and eat a diet rich in fruits, vegetables and whole grains. Limit fats, animal products and processed foods, and try to drink eight to 10 glasses of water each day. Work with your health care provider to find other diet options for altering your ankylosing spondylitis symptoms. (44)
Finding the best ankylosing spondylitis diet for you
As with many conditions with autoimmune and auto-inflammatory elements, there are many possible ways that diet can impact your health. Some people find that certain foods or food groups trigger symptoms. Others may find that eating a certain way keeps their ankylosing spondylitis symptoms in check or even in remission. Ask your health care provider about ways to study and tweak your diet to maintain a healthy intake of nutrients and maximize your ankylosing spondylitis-related health.
Research suggests that a low-starch diet may be beneficial for people with ankylosing spondylitis. This is likely because of its ability to reduce inflammation. (45, 46) Low-starch diets may also be referred to as ketogenic or the keto diet, and it is possible that this type of diet may be particularly beneficial when used in conjunction with medical therapy. (47) However, there can be downsides to following a low-carb diet for people with certain health conditions or medications.
Another study suggests that a diet rich in omega-3 fatty acids may decrease disease activity in people with ankylosing spondylitis. (48) Although other research makes it unclear how close a tie exists between omega-3 consumption and disease activity, it does appear to have some impact on disease-related indicators. (49)
9. Ask your doctor if you need folate supplements or probiotics.
Some of the drugs used to treat ankylosing spondylitis can affect your liver and gut. In some cases, taking a folic acid supplement or adding active-culture yogurt and a banana to your daily diet can help your body protect itself against the possible side effects of the drugs. (50)
10. Avoid certain diets or dietary additives.
The Arthritis Foundation reports that diets high in alfalfa, zinc, or copper salts — as well as the “immune power diet” or a diet low in calories, fat and protein — are known to be harmful. (51)
11. Maintain a healthy weight.
Both overweight and underweight people can have complications with their ankylosing spondylitis. Certain medications can impact your weight, and illnesses that often occur at the same time as ankylosing spondylitis can also cause weight gain or loss. (52) Let your health care provider know if you gain or lose weight quickly or if you need help getting to a healthy weight.
12. Don’t smoke.
Ankylosing spondylitis can restrict the movement of your rib cage, making it hard to take deep breaths. (53) That can make the strain of smoking on your lungs even more dangerous than it otherwise is.
13. Use task-related accommodations.
For example, if you have trouble bending to put your shoes on, use a long-handled shoehorn. If walking is challenging, use a cane or walker. Similarly, if you are in stooped or difficult positions during work, adjust the height of your desk or monitor, or alternate your activities as frequently as possible. And if you have other activities that are difficult because of your condition, work with an occupational therapist to find new ways to do them. (54)
Precautions
Ankylosing spondylitis is a chronic disease. That means it lasts a long time — usually a lifetime — once diagnosed. You can minimize symptoms, delay disease progression and optimize your health by following the advice of your health care provider and working hard to take care of yourself in other ways. However, you should not start taking supplements or change your diet drastically without discussing it with a health care professional. Supplements and dietary changes can impact the effectiveness of medications and can affect both your ankylosing spondylitis and other health issues you may have.
Likewise, do not stop or change your medication regimen without speaking with a health care professional. Some medications for ankylosing spondylitis require tapering if you wish to stop taking them, making it risky for you to stop on your own. If you have side effects from a medication or supplement, call your health care provider or seek emergency care if needed.
You should also work with a doctor or physical therapist to find and begin physical activities safely. Because exercise is so essential to your long-term health, make sure you are doing it right by checking in with the experts from time to time.
Chiropractic care is not considered safe for people with ankylosing spondylitis, according to the Spondylitis Association of America. (55) This is because manipulation of the spine can result in injury (such as spinal fracture) or nerve damage, especially if bone fusion has begun.
Ankylosing Spondylitis Key Points
- Ankylosing spondylitis is a chronic form of arthritis that eventually causes limited mobility of the spine. However, some people go into remission.
- Symptoms and their severity vary from person to person.
- There is currently no cure for ankylosing spondylitis. When ankylosing spondylitis treatment is required, it is aimed at reducing pain and stiffness as well as trying to prevent deformity and limits on your activities.
- Generally, an ankylosing spondylitis prognosis for someone who receives medical therapy and engages in regular physical activity is good. People live with and manage the disease for decades and can usually overcome the pain and mobility limitations without severe limits in their day-to-day lives.
- By staying physically active, working with a health care professional to find the right treatments for you, and taking good care of your physical health, you should be able to effectively manage your ankylosing spondylitis.